The contents of this review may appear odd. After a brief description of the coxofemoral joint, the entities discussed include ilioinguinal neuropathy within the context of the nerves that may be damaged during lower abdominal surgery, meralgia paresthetica, piriformis syndrome with the appropriate caveats, trochanteric syndrome, “ischial bursitis” and trochanteric syndrome caused by ischemia. These cases were chosen to stress our belief that rheumatologists are first and foremost internists. We further believe that being current in other pathologies such as peripheral neuropathies and certain vascular syndromes sooner or later benefits our patients.
Este texto sobre pelvis y cadera pudiera causar sorpresa. Después de algunas consideraciones acerca de la articulación coxofemoral, se discuten, en sus aspectos anatómicos, la neuropatía ilioinguinal en el contexto de los nervios expuestos a daño iatrogénico, la meralgia parestésica, el síndrome del músculo piriforme con las reservas del caso, el síndrome trocantérico, la “bursitis isquiática”, y un caso de pseudosíndrome trocantérico por oclusión arterial. Elegimos estos casos para enfatizar que antes de ser reumatólogos fuimos internistas y que no debemos perder una visión integral de nuestros pacientes. Estamos convencidos de que los reumatólogos, además de poseer conocimientos de medicina interna y del sistema musculoesquelético, deben estar informados acerca de otras patologías que entran en el diagnóstico diferencial del dolor regional.
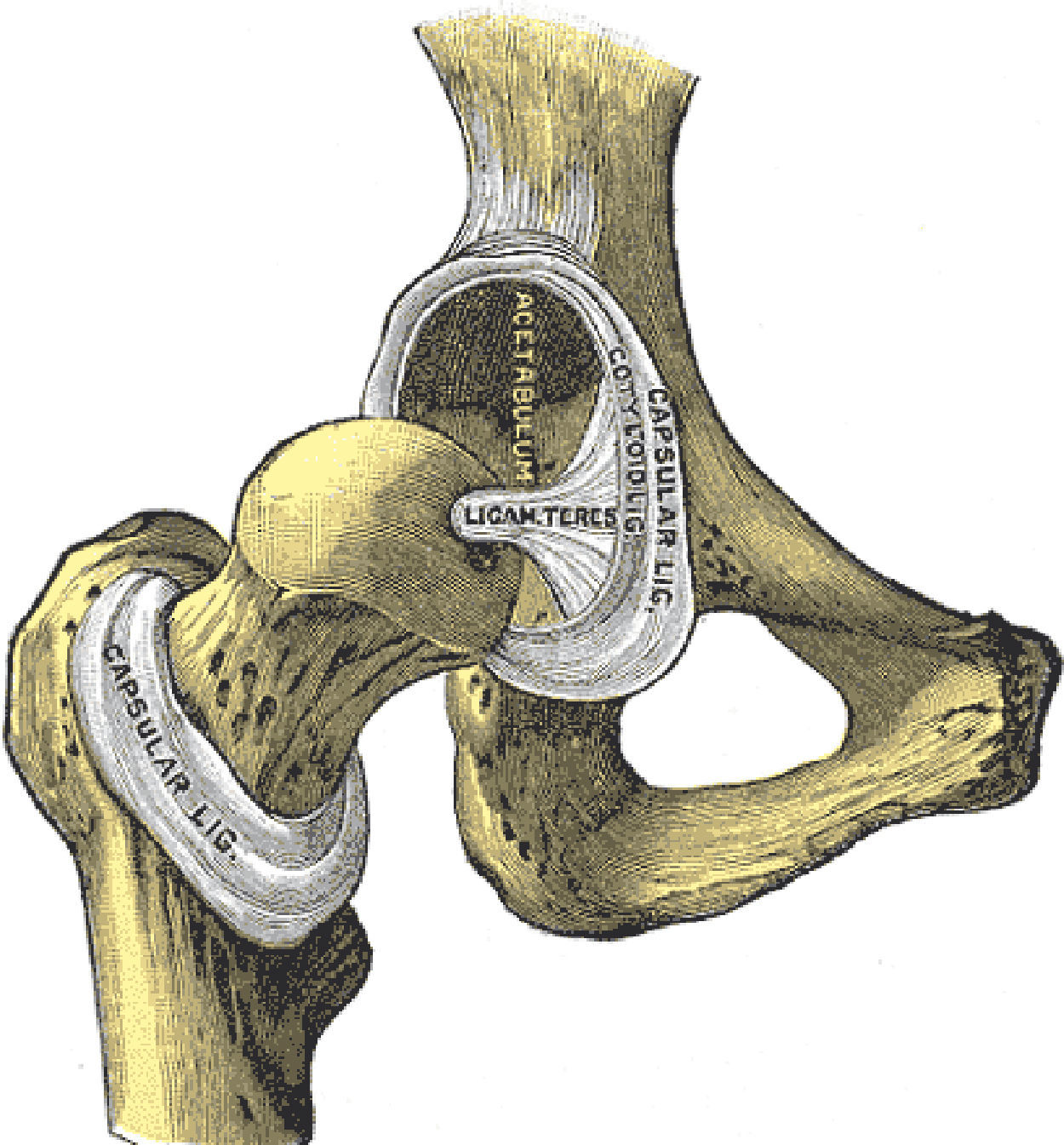
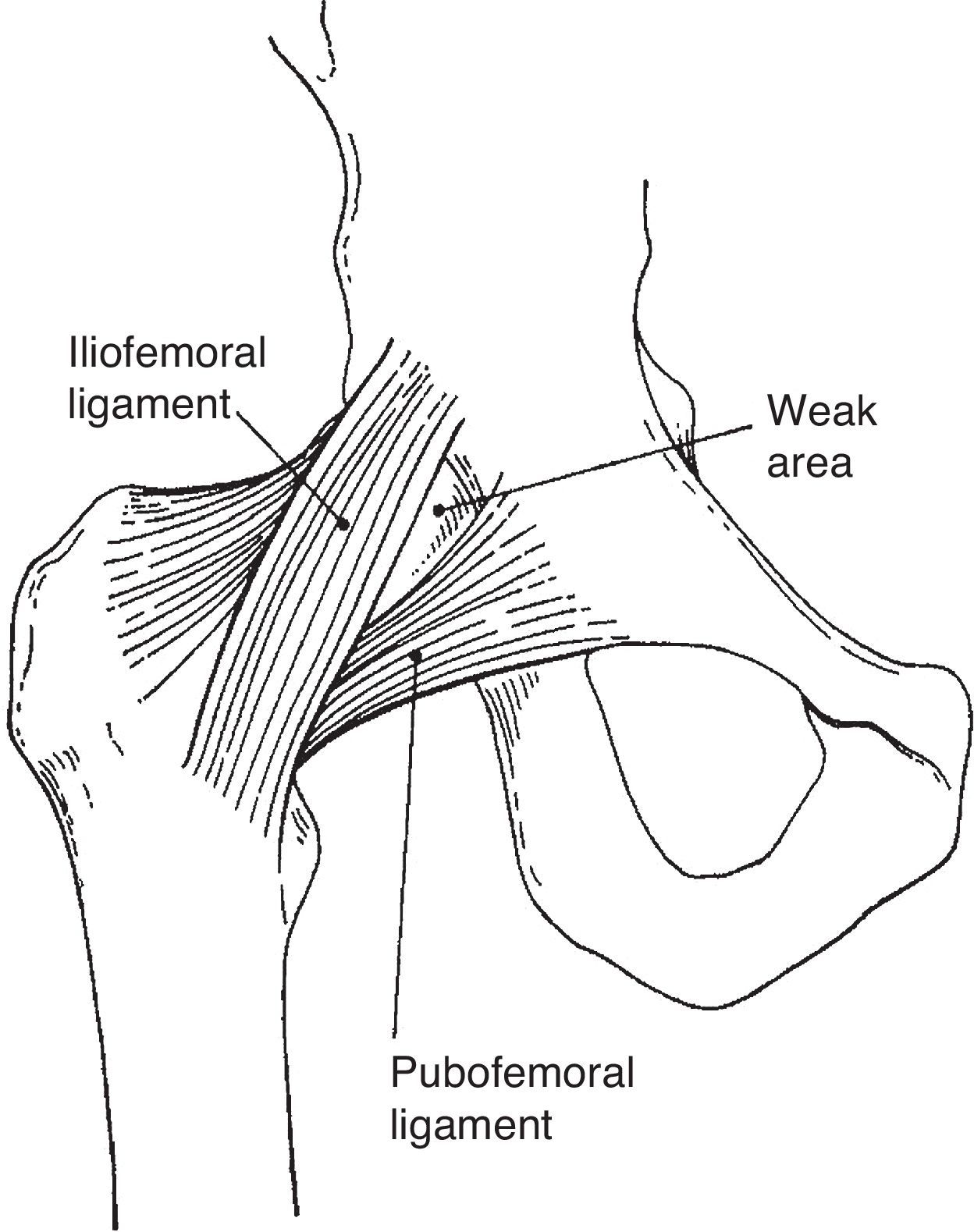
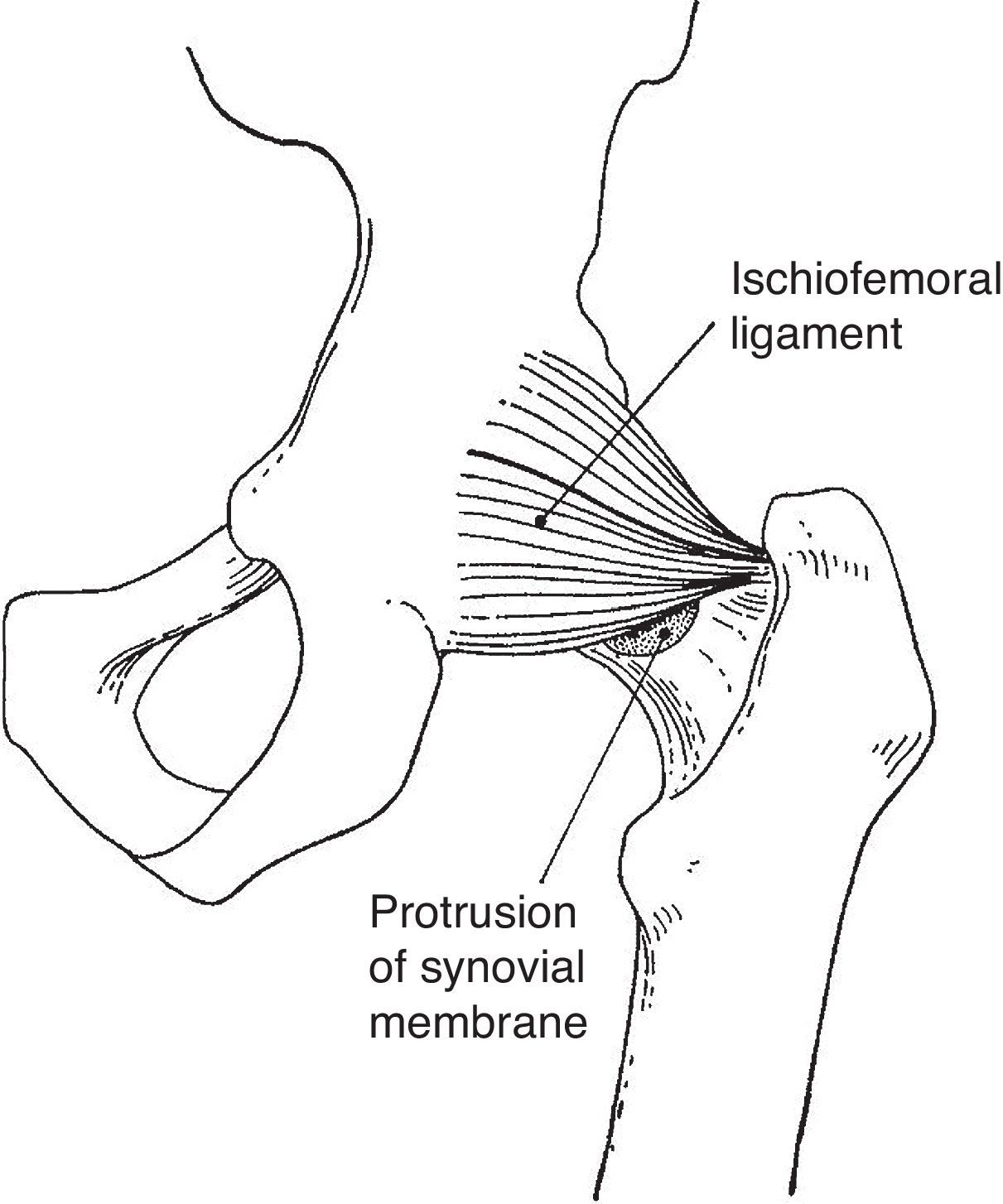
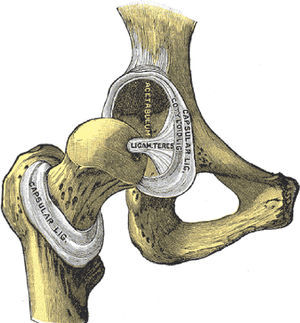
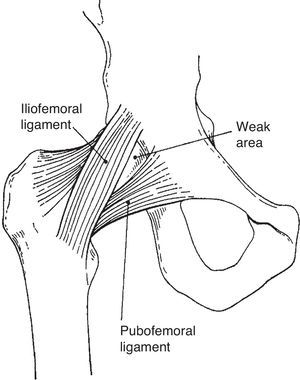
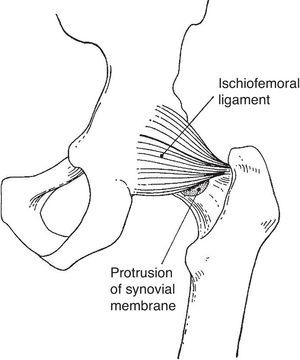
The coxofemoral joint is a ball-and-socket or spheroidal joint in which the femoral head is largely contained in the acetabulum of the pelvis (Fig. 1). Embryologically, 2/5 of the acetabulum are derived from the ilium, 2/5 from the ischion and 1/5th from the pubis. While hyaline cartilage covers the femoral head, on the acetabular side the cartilage is C-shaped leaving in the center the acetabular fossa. The C is completed into an O by the transverse ligament of acetabulum. Peripherally, the acetabular cartilague is extended by the labrum acetabulare, a tough fibrous and fibrocartilaginous rim.1,2 The ligament of the head of femur or ligamentum teres extends from the transverse ligament of the acetabulum to a fovea in the head of femur. This ligament conveys important nutrient vessels for the humeral head. The capsule of the coxofemoral joint is thickest in its upper portion where in the erect posture the load is maximal. The longitudinally-arranged external fibers of the capsule are reinforced at specific sites by ligaments that provide stability and limit certain motions of the coxofemoral joint (Figs. 2 and 3). The iliofemoral ligament or Y ligament of Bigelow, the most powerful ligament in the human body, reinforces the superior and anterior aspects of the capsule and limits extension. The pubofemoral ligament reinforces the inferior aspect of the capsule and limits external rotation in extension. The ischiofemoral ligament reinforces the posterior aspect of the capsule and limits internal rotation and adduction. Finally, the inner portion of the capsule encircles the femoral neck as a buttonhole and reinforces the joint at the orbicular zone or anular ligament. In cadaveric studies the hip position in which a given volume of effusion is at its lowest pressure is from 30 to 65 degrees of flexion, 15 degrees of abduction and 15 degrees of external rotation.3 This is the position that patients with acute arthritis of the hip spontaneously adopt. A most important point in the examination of patients with lower extremity pain is that pain that originates in the hip tends to radiate distally toward the knee. Patients are frequently surprised when they are told that an anteromedial pain in the thigh that they had previously blamed on the knee in fact originates in the hip. Hip pain typically involves the groin and the anteromedial thigh. Additional areas of radiation include the trochanteric region and the buttock. Reproduction of this pain with hip motion and an absence of pain with lumbar and knee motion should clearly incriminate the hip as the affected joint.4,5 This paper is unorthodox in that other than coxofemoral conditions and even other than regional rheumatologic conditions will be discussed. Instead, emphasis will be made on neural and vascular structures that surround the hip. This paper further emphasizes our tenet that rheumatologists are internists not only with a specialization in musculoskeletal conditions, but in the peripheral nervous system and the vascular system as well. A review of hip examination can be found in recent accounts.6–10
The hip joint with the capsule removed. Notice the ligamentum teres that connects the transverse ligament of the acetabulum and the fovea in the humeral head. The acetabulum is placed at the intersection of the iliac, pubic and ischial bones.
The iliofemoral and pubofemoral ligaments. The weak area is the capsular area where in adults a connection is often created spontaneously between the hip joint and the iliopsoas bursa. This acquired connection allows joint fluid enter and disted the bursa as an iliopsoas cyst.
Patient 1. Ilioinguinal neuropathy. “A 59 year-old man walked into the office bent over and in acute pain. Three months prior, one month after a left inguinal herniorrhaphy, he begun to experience shooting inguinoscrotal pains along with a dragging feeling at the base of the penis every time he tried to stand erect. On examination an irregular induration was felt at the surgical scar. A CT scan showed an irregular opacity at the tender site. Brought to the operating room, a piece of gauze was removed. Next day he was able to stand erect”
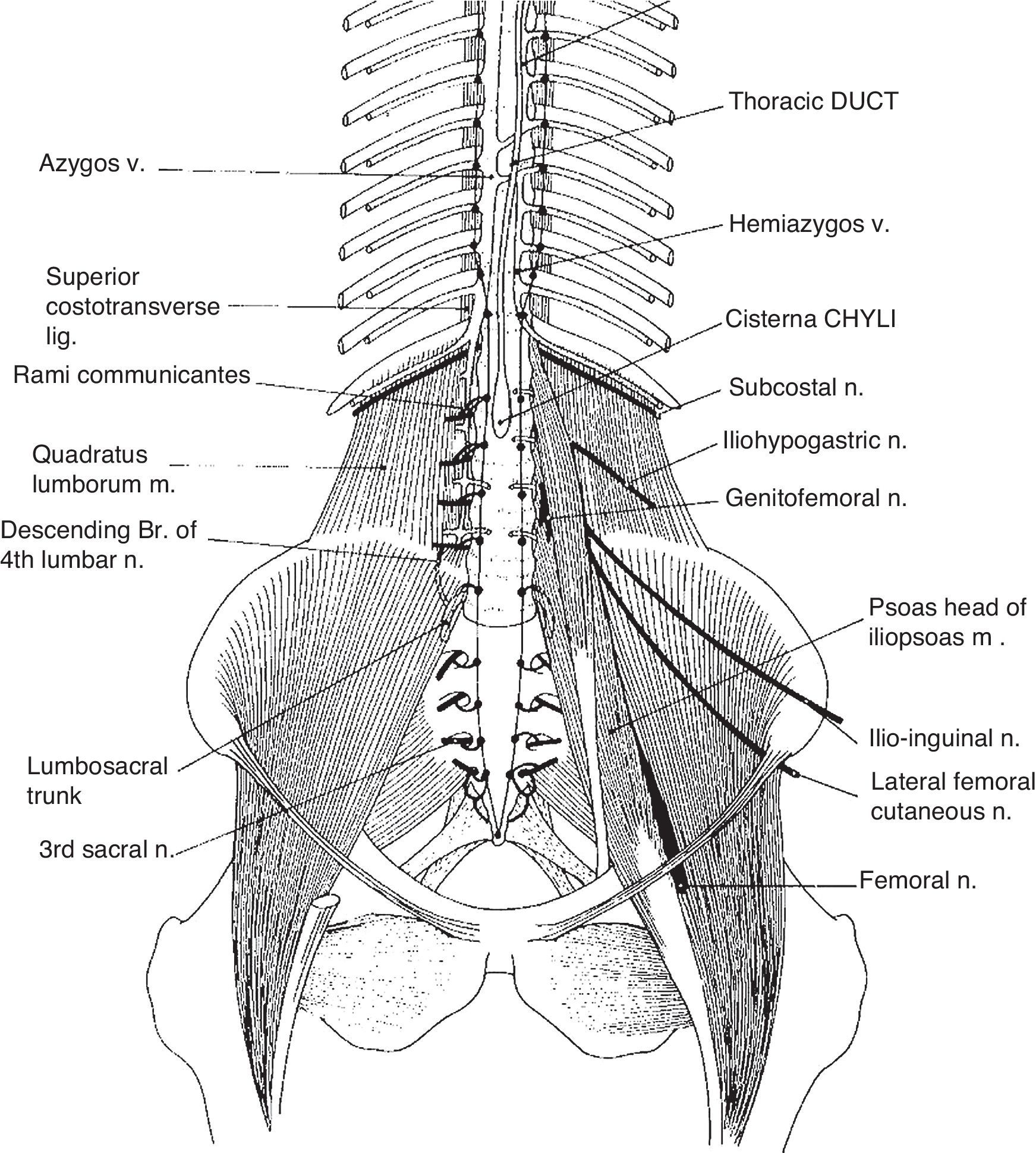
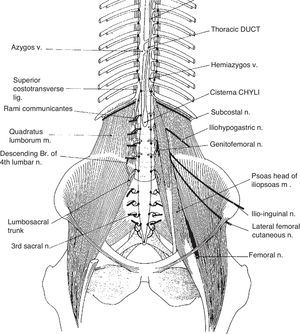
This case illustrates an inguinal-genital-femoral pain syndrome resulting from a nerve injury in the abdominal wall. The abdominal wall is comprised of 3 lateral muscles, from deep to superficial transversus abdominis, internal oblique and external oblique. Anteriorly, rectus abdominis connects the xyphoid and neighboring costal cartilages, and the pubis. Three nerves, the iliohypogastric, the genitofemoral and the ilioinguinal, which bear an intimate relation with the abdominal wall muscles, may be injured at such routine surgical procedures as an appendectomy, an inguinal herniorrhaphy, endoscopic hernia repairs, a Pfannestiel incision and a lipectomy.11–15 These three nerves originate in the upper lumbar plexus, run from back to front and from up down and are anterior to the flexion-extension axis of the coxofemoral joint (Fig. 4). Thus, they are stretched by extension and relieved by flexion of the hip joint. In our patient, paroxysmal pain occurred on any attempt at extension and pain was relieved by a progressively stooped position.15 The iliohipogastric nerve arises from L1, T12 and pierces the iliopsoas and transversus abdominis above the iliac crest; a lateral branch innervates the superolateral gluteal region and an anterior branch, the suprapubic skin. The ilioinguinal nerve, which is the nerve that was entrapped in our patient, arises from L1, emerges from the psoas, pierces transversus abdominis and internal oblique, enters the inguinal canal and supplies the skin at the base of the scrotum, the root of the penis and the labium majus. The genitofemoral nerve arises from L2 and descends posterior to the ureter. One branch of this nerve enters the inguinal canal and innervates a small portion of the lateral scrotum, mons pubis and labium majus and another branch, the femoral, innervates the skin just distal to the groin (the upper part of the femoral triangle). Another nerve of interests to rheumatologists is the twelfth intercostal (or subcostal) nerve. This nerve has, same as the iliohypogastric, a lateral branch which in severe scoliosis may be compressed between the last rib and the iliac crest causing trochanteric pain. A final nerve to be discussed is the lateral femoral cutaneous nerve. This nerve arises from L2, L3, enters the thigh beneath the inguinal ligament about 1.5cm medial to the anterosuperior iliac spine and follows a short subfascial course before piercing the fascia lata to innervate the skin in the anterolateral thigh.16 Damage to this nerve causes a well-known clinical syndrome, meralgia paresthetica. Extrinsic compression may be caused by the weight of abdominal wall in obesity, ascitis, pregnancy or other local causes such as the use of corsets.17,18 It may also result from diabetic neuropathy. One of the authors saw 94 cases of meralgia paresthetica, usually in association with some other condition, among 6900 new rheumatologic patients seen during the past 19 years. Thus, the condition is common in a general rheumatologic practice – if one looks for it. Hyperextension of the thigh is said to increase pain in this condition.16 A constant finding is tenderness medial to the anterior superior iliac spine. Percussion at this site may trigger paresthesiae in the symptomatic area.
The complex arrangement of the lumbar plexus-derived nerves is shown from the front. The iliohypogastric and the iliolumbar nerves are close to each other and their course is roughly parallel. The genitofemoral nerve has a vertical course following the ureter and the iliac artery. The lateral femorocutaneous nerve has a lower origin and, as seen in the Figure, exits the pelvis medial to the anterior superior iliac spine.
Patient 2. Piriformis syndrome. “A 50 year old grandmother developed, after caring for 3 small grandchildren over the weekend, a severe left buttock pain with shooting paresthesiae in the posterior thigh. Physical examination revealed a well-looking woman with normal lower back motion. Leg length was equal. Passive internal rotation of her extended left leg triggered the pain and the paresthesiae. The Lasègue maneuver was negative.”
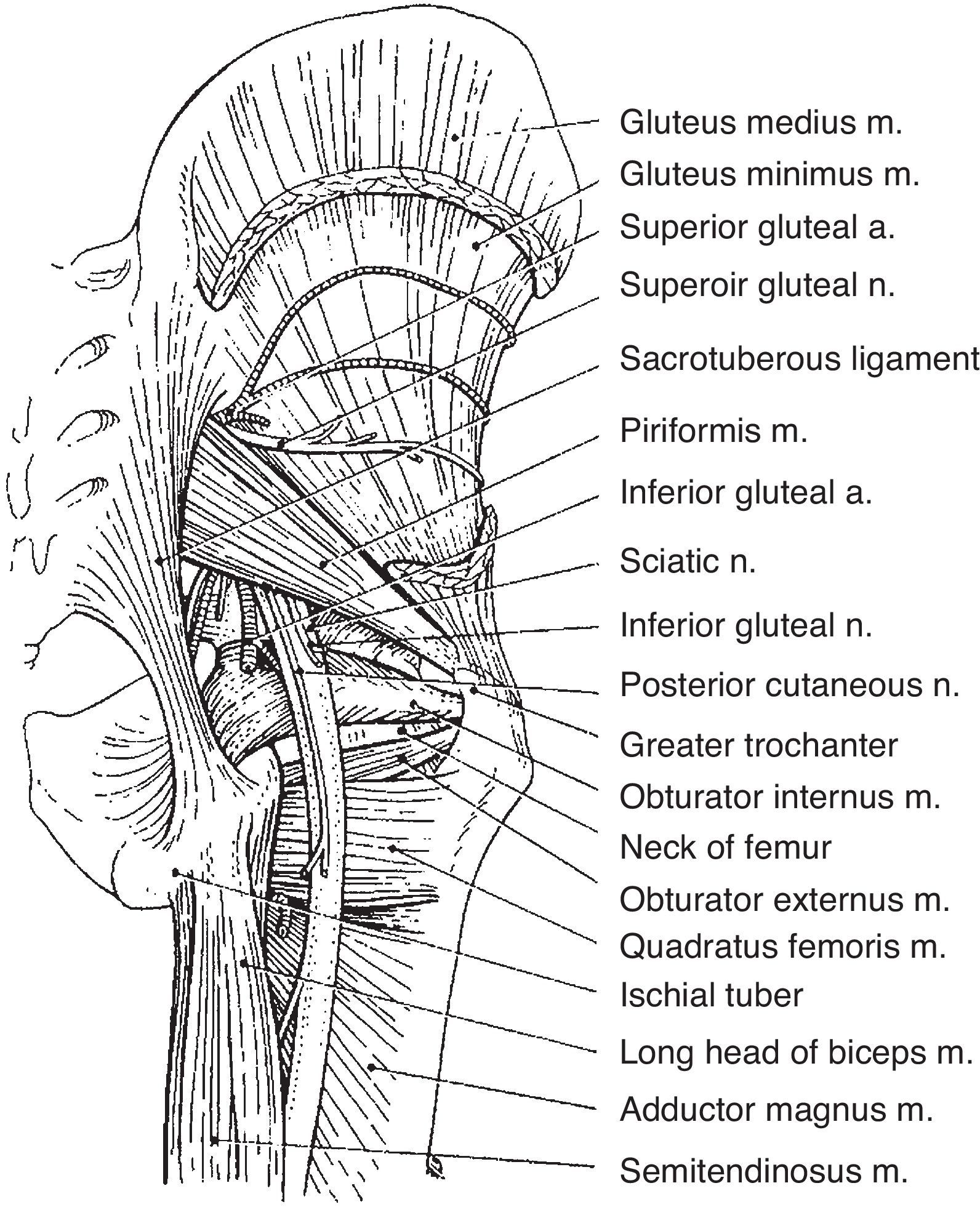
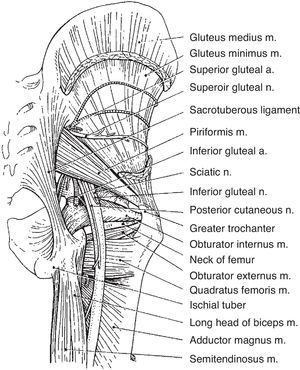
Sciatica, which is the clinical syndrome that denotes the irritation, reflex changes and muscle atrophy that result from dysfunction of the sciatic nerve, may have intraspinal and extraspinal causes. An extraspinal cause of sciatica that remains controversial in terms of frequency, pathogenesis and investigation is the piriformis syndrome. This issue is further complicated by a tendency to ascribe to the piriformis cases of buttock pain made worse by passive internal rotation of the hip in the absence of sciatica. Piriformis, a lateral rotator of the hip, arises from the anterior surface of the sacral vertebrae S2, S3 and S4, exits the pelvis through the greater sciatic notch and inserts via a rounded tendon in the medial surface of the greater trochanter (Fig. 5). This is in the proximity to the insertion of the obturator internus and the gemelli muscles, all of them, as piriformis, external rotators of the hip. The sciatic nerve emerges from the pelvis below the piriformis muscle in about 90% of cadaveric dissections.19 In the remaining 10% anatomical variations are found, in particular a bifid sciatic nerve or a bifid piriformis muscle, in various positions relative to each other, which in some individuals may be a predisposing factor to a piriformis syndrome. Additional variables include a bulky piriformis muscle and abnormal connective tissue strands. The issue is made even more complex due to the use of different diagnostic criteria and a lack of validation of diagnostic maneuvers. Commonly described findings in piriformis syndrome include buttock pain, sciatica, tenderness over the greater sciatic notch, aggravation of pain in the sitting position and, in long standing cases, gluteal atrophy. A positive Lasègue maneuver is present in most cases. Provocation maneuvers that increase piriformis muscle tension include passive internal rotation and resisted external rotation of the hip with the thigh in extension.20–22 Since piriformis is an abductor when the hip is at 90 degrees flexion, an additional, perhaps more specific provocation maneuver is to resist abduction in the sitting position or Pace test.22 Our bias is this: a localized buttock pain triggered by local compression, passive internal rotation and resisted external rotation do not necessarily implicate piriformis, as any of the external rotators of the hip may be the cause. Also, the specificity of the resisted abduction of the hip in a sitting patient is uncertain. Thus, unless sciatica is triggered or an abnormal piriformis is shown on imaging studies in the symptomatic side, we would be reluctant to diagnose a piriformis muscle syndrome based on buttock pain triggered by the provocative maneuvers.
The external rotators of the hip are shown including piriformis, the external and internal obturator muscles and quadriceps femoris. The sciatic nerve emerges from the pelvis beneath piriformis.
Patient 3. Trochanteric syndrome. “A 60 year-old man is seen because of a lateral right hip pain that is severe at night while lying on his right side. Physical examination reveals a normal lumbar spine, normal hip motion, a right leg 2cm longer than the left, and severe tenderness on palpation of the posterior angle of the greater trochanter.”
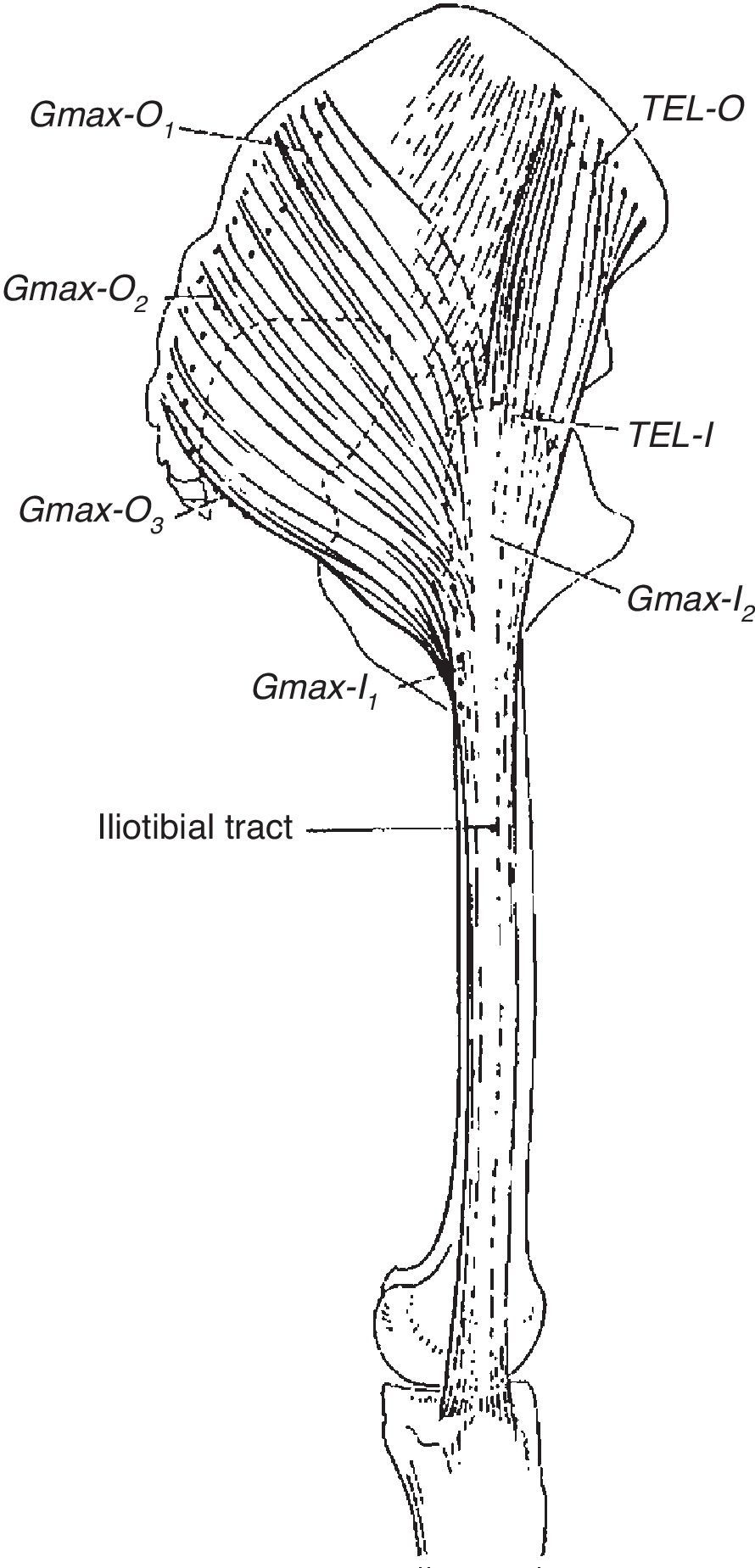
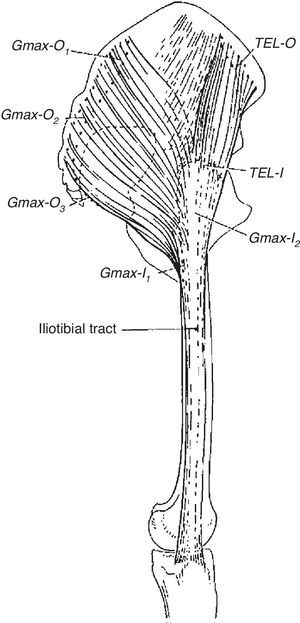
The anatomy of the trochanteric region can be best understood in layers. Deep to the subcutaneous fat lies the iliotibial tract, which is a strong lateral condensation of the fascia lata or aponeurotic fascia of the thigh. The iliotibial tract inserts in the iliac crest, overlies the greater trochanter, inserts indirectly in the lateral femoral condyle and reaches its distal insertion in the lateral tuberosity of the tibia (Gerdy's tubercle) (Fig. 6). Tensor fascia lata arises in the vicinity of the anterior superior iliac spine and inserts in, or descends as an anterior fascicle of, the iliotibial tract.23 Gluteus maximus, the hallmark of bipedality, has an extensive origin in the iliac bone behind the posterior gluteal line, the sacrotuberous ligament, the thoracolumbar fascia, the sacrum and the coccix.24,25 The superficial fibers and the upper deep part of this muscle merge into the iliotibial tract while its lower deep fibers insert in the gluteal tuberosity of the femur. Thus, two muscles attach in the iliotibial tract, one anteriorly and the other posteriorly, at or just distal to the greater trochanter. The trochanteric bursa separates the iliotibial tract from the greater trochanter. The next layer is comprised of two overlapping muscles, gluteus medius and gluteus minimus. Gluteus medius has a wide origin on the surface of the iliac bone between the anterior and the posterior gluteal lines and inserts in 3 facets in the greater trochanter, the anterior, the lateral and the posterosuperior.26 Gluteus minimus, which is covered by the former, also arises from the iliac bone below the anterior gluteal line and inserts in the anterior facet of the greater trochanter and partially in the joint capsule. Gluteus medius, gluteus minimus and tensor fascia lata stabilize the pelvis, and abduct and internally rotate the hip. Gluteus maximus also stabilizes the pelvis, helps in abducting the hip, and is an external rotator and an extensor of the hip. Tensor fascia lata, gluteus medius and gluteus minimus are innervated by the superior gluteal nerve that exits the pelvis above piriformis and runs between the latter two muscles. This nerve, particularly the branch for tensor fascia lata, runs quite close to the greater trochanter and may be damaged during surgical procedures.27 Gluteus maximus is innervated by the inferior gluteal nerve which exits the pelvis below piriformis. The greater trochanter receives sensory innervation by a branch of the femoral nerve that approaches the trochanter from its back.28
The iliotibial tract. There is a poorly defined attachment to the iliac crest. At the greater trochanter the tract receives the insertion of tensor fascia lata anteriorly and most fibers of gluteus maximus in the back. Distaly, the iliotibial tract inserts in the lateral tubercle of tibia. Thus, the iliotibial tract is a bi-articular ligament (hip and knee) that functions as a static and a dynamic stabilizer of the knee.
Patient 4. Ischial “bursitis”. “A 40 year old office clerk was seen because of a severe left buttock pain present while sitting but not while standing. He had been given a doughnut cushion and nonsteroidal anti-inflammatory agents with minor and transient relief. Marked tenderness was noted on the left ischion when he was lying down face up holding his flexed legs against his chest. The most tender area was identified and he was given an infiltration with a depo steroid mixed with a local anesthetic. He was also advised to use a higher chair and to seat putting his weight on the thighs rather than on the tender point. He had complete relief.”
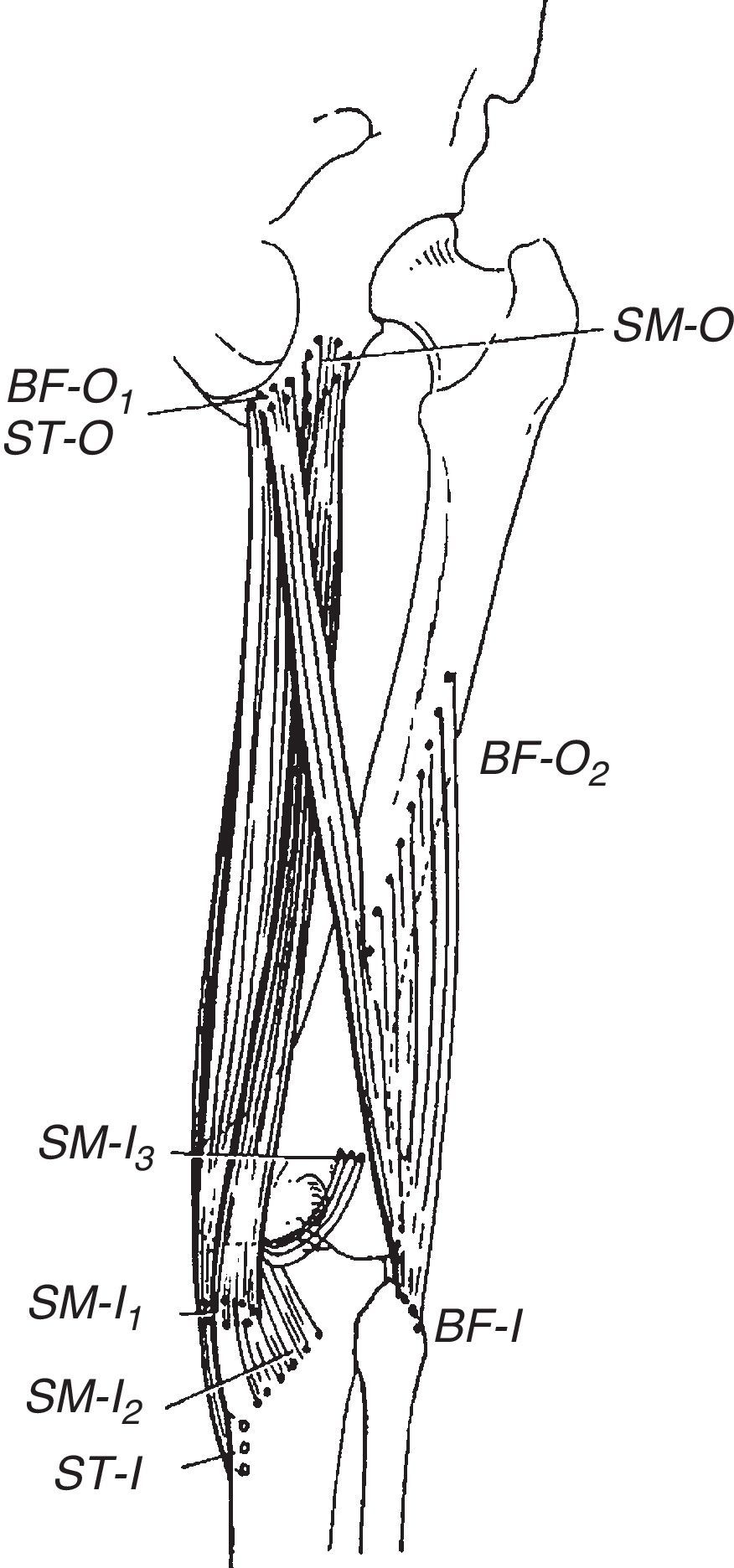
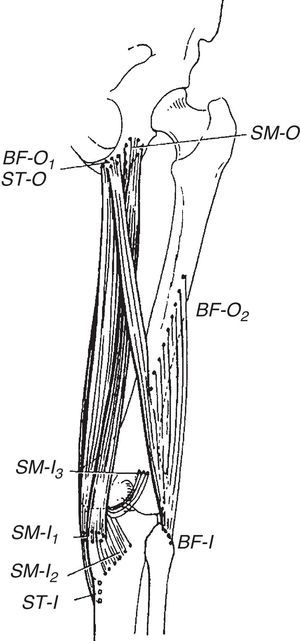
The ischial tuberosity is the site of origin of the long head of biceps femoris, semitendinosus and semimembranosus (Fig. 7). This can be attested by palpation of one's ischion while standing and flexing the knee. The long head of biceps and semitendinosus insert in the posteromedial surface of the ischial tuberosity and semimembranosus in its anterolateral surface.29 These muscles extend the hip and because their insertion is past the knee they are also knee flexors. The ischions are covered by the glutei maximi in the standing position but in the sitting position these muscles move to the sides leaving the ischial tuberosities unprotected. Thus, weight is discharged on the ischion and the surrounding tissues. Excessive load at this site may lead to the formation of an adventitious bursa, the ischiogluteal bursa.30 In addition to a depo-steroid injection these patients should be given a lower back support, review the chair height and shift their weight from the ischiae to the thighs and the back support. Anterior flexion of the pelvis increases the contact pressure on the thighs and relieves pressure in the ischial tuberosities and the sacrum.31
The origin and insertions of the ischiotibial muscles (semitendinosus, semimembranosus) as well as the ischial and femoral origins of bicerps cruris muscle, which insert in the fibula, are shown. These muscles are extensors of the hip and flexors of the knee.
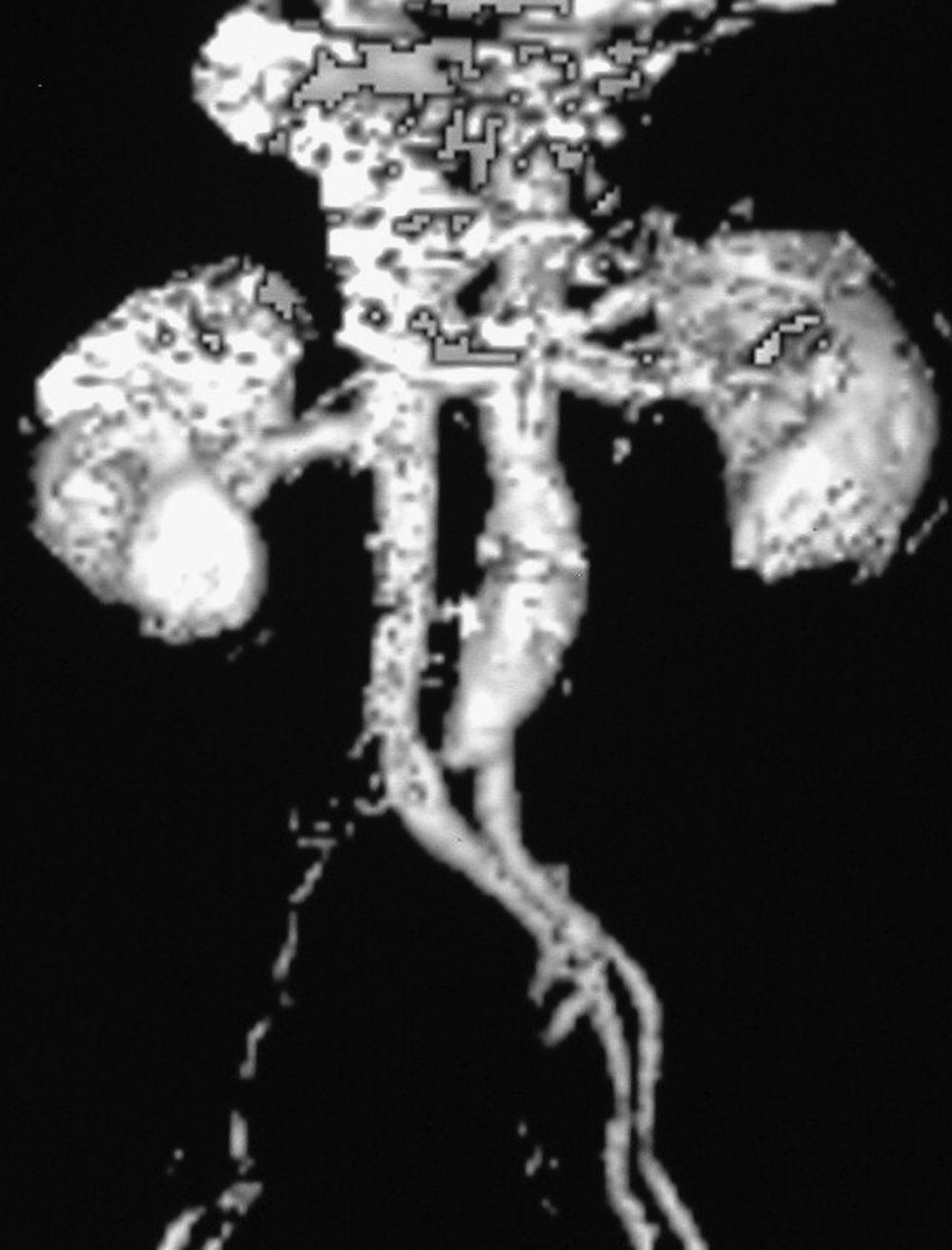
Patient 5. Pseudotrochanteric syndrome caused by ischemia. “An 81 year-old man was seen because of a refractory right trochanteric syndrome. Symptoms begun 1 month prior. An orthopedic colleague had administered 4 corticosteroid infitrations. In addition, he had intensive physical therapy treatment. He was unimproved and indeed felt worse. He arrived to the office in a wheel chair. He was interrogated with emphasis in the very onset of symptoms. He recalled that the initial pain was above the right iliac crest. Pain radiated to the foot where he had numbness and tingling of the great toe. Upon examination there was severe tenderness on the right greater trochanter. The right foot was cold. No pulses were noted on the pedal, posterior tibialis, popliteal and femoral arteries of the right leg. Pulses in the left leg were normal. A vascular surgeon was immediately consulted and an angio-TAC was performed. A complete occlusion of the right iliac artery was present (Fig. 8). The patient was brought to the operating room, a thrombectomy was performed and a stent was placed. There was immediate reperfusion of the leg and the next day the trochanteric pain had disappeared.
This case, indeed rare, was included because it illustrates how important is to obtain a detailed history in patients who present with a regional pain syndrome. We do not have an explanation for the unusual location of the ischemic pain. Rheumatology is a discipline that is learned after internal medicine training and we should never forget this background. This should make us able to step back, obtain a broader perspective and in so doing find an explanation of our patient's symptoms.
Practical review of the hip and related anatomical structures- •
The anterior superior iliac spine
- •
Exit point of the lateral femoral cutaneous nerve of the thigh
- •
Superficial territories of the ilioinguinal nerve, the iliohypogastric nerve and the genitofemoral nerve
- •
Greater trochanter
- •
Walking self-test for:
Tensor fascia lata
Gluteus medius
Gluteus maximus
- •
Lequesne tests 1 and 2 for internal rotators tendinopathy (gluteus medius and gluteus minimus)
- •
Ober's maneuver with its variants for the two muscular components of the iliotibial tract, tensor fascia lata and gluteus maximus
- •
Sacrum, sacral hiatus
- •
Dimples of venus, relation to posterior superior iliac spine, SI joint, sacral tubercles
- •
The ischial tuberosity
- •
Self examination of the ischial region while standing up (gluteus maximus, hamstring muscles)
- •
Self examination of the ischial region while standing and flexing one leg to 90 degrees
- •
Test for piriformis with the leg in extension and with the knee flexed 90 degrees
The authors have no conflict of interest to declare.