To date few studies have examined whether ultrasonography can depict morphologic differences in painful and painless osteoarthritis (OA). This study describes and compares the clinical, radiographic and ultrasonographic findings of patients with both painful and painless proximal interphalangeal (PIP) and/or distal interphalangeal (DIP) OA.
MethodsPatients with PIP and/or DIP OA (ACR criteria) were prospectively recruited. The clinical rheumatologist chose up to 3 painful joints and up to 3 painless symmetric joints in each patient to define 2 cohorts of OA: symptomatic (SG) and asymptomatic (ASG). A conventional postero-anterior hand X-ray was performed and read by one rheumatologist following the OARSI atlas, blinded to clinical and sonographic data. Ultrasound (US) was performed by an experienced rheumatologist, blinded to both clinical and radiographic data in joints previously selected by the clinical rheumatologist. US-pathology was assessed as present or absent as defined in previous reports: osteophytes, joint space narrowing, synovitis, intra-articular power Doppler signal, intra-articular bony erosion, and visualization of cartilage. Radiographic and ultrasonographic intrareader reliability test was performed.
ResultsA total of 50 joints in the SG and ASG were included from 20 right-handed women aged 61.85 (46–73) years with PIP and DIP OA diagnosed 6.8 (1–17) years ago. In all, 70% SG and ASG joints were right and left sided respectively. The SG showed significantly more osteophytes, synovitis and non-visualization of joint cartilage. Intrareader radiographic and ultrasonographic agreement was excellent.
ConclusionThis study demonstrates that painful PIP and/or DIP OA has more ultrasonographic structural changes and synovitis.
Pocos estudios han examinado si existen diferencias morfológicas detectables con ecografía entre las articulaciones sintomáticas y las que no lo son en pacientes con artrosis. Este estudio describe y compara los hallazgos clínicos, radiológicos y ecográficos de los pacientes con artrosis interfalángica proximal (IFP) y/o distal (IFD) que tienen articulaciones con y sin dolor.
MétodosProspectivamente, se incluyó a pacientes con artrosis IFP y/o IFD según los criterios ACR. El reumatólogo clínico eligió hasta un máximo de 3 articulaciones dolorosas y 3 articulaciones no dolorosas de localización simétrica en cada paciente para formar 2 cohortes de artrosis: grupo con dolor (GD) y grupo sin dolor (GSD). La radiografía simple postero-anterior de las manos fue leída por un reumatólogo según las recomendaciones del atlas OARSI, ciego a toda información clínica y ecográfica. El estudio ecográfico fue realizado por un reumatólogo en las articulaciones previamente seleccionadas por el clínico ciego a los datos clínicos y radiológicos. Se registraron como ausente o presente: osteofitos, pinzamiento articular, sinovitis, señal Doppler intraarticular, erosiones y visualización del cartílago. Se realizó un estudio de fiabilidad intralector para la radiología y para la ecografía.
ResultadosSe estudió un total de 50 articulaciones en cada cohorte de 20 mujeres diestras de 61,85 años de edad (46–73) con artrosis IFP y IFD diagnosticada hace 6,8 años (1–17 años). El 70% de las articulaciones del GD y GSD se localizaron en la mano derecha e izquierda, respectivamente. El GD tenía significativamente más osteofitos, sinovitis y ausencia de cartílago que el GSD. La fiabilidad interlector radiológico y ecográfico fue excelente.
ConclusiónLa ecografía detecta más daño estructural y sinovitis en las IFP y/o IFD artrósicas que presentan dolor.
Osteoarthritis of the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints is the most common cause of hand pain and disability in the developed world. At present, both its diagnosis and its follow-up are based on clinical and radiological parameters. However, as is well known, there is no correlation between symptoms and radiographic changes. We may find patients with joint pain and little or no radiological changes and patients with significant radiological structural lesions without pain. There are numerous alterations, inflammatory, morphological and structural, on the joint and extra-articularly that can cause joint pain, effusion, synovitis, mucinous cysts, cartilage lesions, erosions and osteophytes. Ultrasound has innate characteristics that no other imaging techniques have, such as excellent spatial resolution, the ability to obtain multiplanar and dynamic images in real time, and is safe, accessible and performable by the clinician. All the above make this imaging modality widely researched and developed for osteoarthritis.
Helen Keen's group in Leeds, UK, has demonstrated construct validity for ultrasonography versus radiology and the ability of this technique in detecting osteophytes, joint impingement and synovitis in osteoarthritis of the fingers.1 These same authors have shown that ultrasound detected more osteophytes than conventional radiology and, in symptomatic osteoarthritis of the fingers, more synovitis, osteophytes and articular impingement are detected in the joints of2 healthy controls. However, to date no one has explored whether there are detectable morphological differences found by ultrasound between painless and painful PIP or DIP joints in the same patient with osteoarthritis of the fingers.
The objective of this study was to describe and compare the clinical, radiographic and ultrasonographic findings in patients with osteoarthritis of the PIP and/or DIP joints with and without pain. Moreover, morphological alterations related to painful joints were identified.
Patients and MethodsThis descriptive, prospective, cross-sectional study was approved by the local ethics committee and conducted at the University Hospital of Móstoles, Madrid. Patients recruited from the hospital's rheumatology outpatient clinic gave their written consent and had been diagnosed with PIP and/or PIP osteoarthritis according to the criteria of the “American College of Rheumatology”.3 No patient had inflammatory arthropathy, microcrystalline arthritis or fibromyalgia. Intra-articular injection was not allowed at least 6 months before the study. In each patient, the clinician identified 2 or 3 symptomatic and asymptomatic PIP and/or DIP joints with deformity upon inspection, to form osteoarthritis pain (PG) and without pain (PFG) groups. PG joints exhibited pain intensity greater than or equal to 3 on the numeric scale as well as tenderness and joint deformity on inspection, while PFG joints exhibited only articular deformity. All patients underwent clinical, radiological and ultrasound tests as detailed below.
Clinical StudySex, age, duration of disease from diagnosis, dominant hand, profession/occupation and current treatment were recorded. The clinical rheumatologist asked each patient which PIP and/or DIP joint was most painful and the numerical global pain intensity scale (ENID 0-10) score of the finger joints was calculated. The clinician palpated each joint and determined the presence or absence of pain, deformity and effusion. In addition, the clinician chose and recorded the joints of each patient for each cohort. In a diagram of the joints of the hand, the clinician marked with an X those he intended to explore using joint ultrasound.
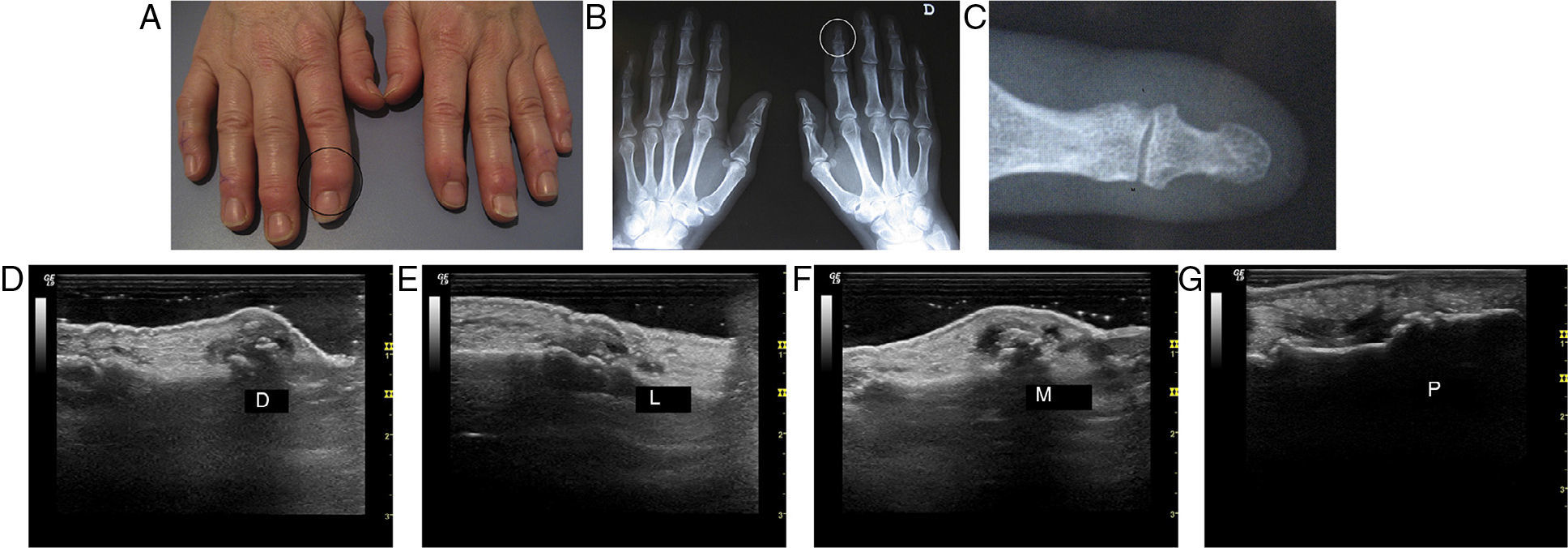
Radiological StudyOne posteroanterior conventional radiography of both hands in the same week as the clinical study was performed. The reading was performed by the same rheumatologist (CFE), blinded to the clinical and ultrasound testing. The following structural lesions were interpreted, as recommended by the OARSI atlas,4 as absent or present: medial and lateral osteophytes in the proximal and distal phalanges of the proximal and distal interphalangeal joints, and joint impingement. Erosions were defined as a cessation of the intrajoint cortex. The intraobserver reliability was tested each month with radiographs of the last 5 of the included patients (Fig. 1).
UltrasonographyAn ultrasound expert rheumatologist (JU) performed the test blinded to clinical and radiological information, a maximum 48h after the clinical examination. A General Electric Logic 9 ultrasound machine with an M12 linear probe (GE Medical Systems Ultrasound and Primary Care Diagnostics, LLC, Wauwatosa, USA) was employed. In their longitudinal and transverse axis, the dorsal, palmar, lateral and medial aspects of each PIP and DIP joint, with the hand outstretched on the table, were explored. Ultrasound semiology of the lesions5 is described below. Each lesion was recorded as absent or present.
Osteophytes: hyperechoic cortical protrusions visualized in 2 planes in the dorsal aspects, palmar, lateral, medial proximal and distal phalanges of the PIP and DIP joints.
Joint impingement: decrease in the space between the cortical margins.
Mucinous cysts: extraarticular anechogenic collection communicating with the joint.
Ultrasonographic synovitis (effusion and/or synovial hypertrophy): distension of the joint capsule ≥1.5mm in its anteroposterior diameter with compressible and/or movable material measured in the dorsal or palmar face.
Signal power Doppler intraarticular Doppler signal (Doppler frequency from 6.3 to 7.5MHz PRF 600Hz, gain set to remove noise).
Erosion by ultrasound: intraarticular cortical defect visualized in 3 planes and in extension and flexion.
Cartilage phalanx head on maximum longitudinal flexion and with the probe on the head of the proximal phalanx, the display or non-display of an anechoic band over the head of the phalanx was assessed.
Once a month, the intraobserver reliability was assessed with video clips of the joints of the last 5 of the patients included.
Statistical AnalysisStatistical analysis was performed using SPSS version 15.0. Quantitative variables were calculated as the average and 95% confidence interval. Qualitative variables were calculated as the percentages. A radiological osteophyte index was calculated as the sum of proximal and distal osteophytes of a medial and lateral location divided by 4, and the ultrasonographic osteophyte index was calculated as the sum of proximal and distal osteophytes of dorsal, palmar, medial and lateral location divided by 8. To study the statistical contrasts, the McNamara and Fisher's tests for related dichotomous independent variables and Student's t-test for independent or related variables were employed. The percentage of radiographic and ultrasonographic intraobserver agreement was calculated.
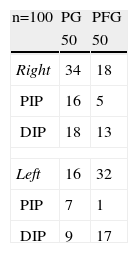
ResultsA total of 50 joints were studied in the PG and 50 in the PFG in 20 right-handed women, 61.85 (46–73) years of age, diagnosed with osteoarthritis of the PIP and/or DIP for a mean 6.80 years (1–17). Seven women worked as maids, 6 as housewives, 3 as laboratory technicians, 3 as seamstresses and one was a manipulative graphic artist. Seventeen of the 20 patients were taking pain medications, NSAIDs being the most common (60%). Table 1 shows the distribution of the joints of the PG and PFG. In all, 70% of painful joints were located in the right hand and their corresponding non-painful joints on the left hand; 40% of PG joints were located on the second right DIP, right third DIP and left second DIP.
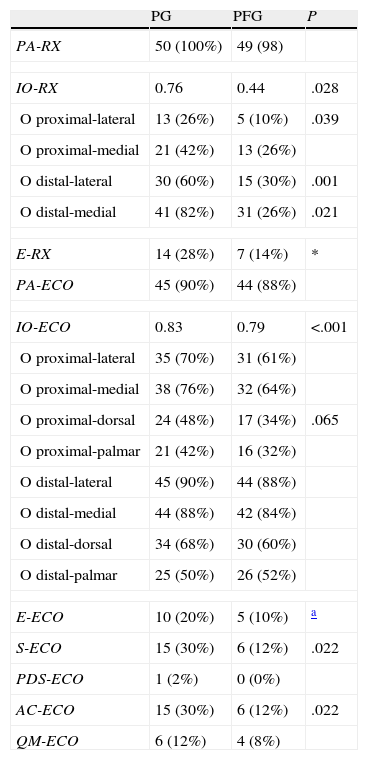
Table 2 shows the radiographic and ultrasonographic findings in the PG and PFG. The PG had significantly greater radiographic and ultrasonographic osteophyte index scores, with no sonographic visualization of synovitis and cartilage. Sonography detected more osteophytes than radiology. The ultrasound osteophyte index was higher in PG and PFG than radiologically (P<.001 and P<.006, respectively). Ultrasound detected synovitis in 15 and 6 joints of the PG and PFG, respectively, while clinical palpation led to the suspicion of arthritis in 14 and 0 joints of the PG and PFG, respectively.
Radiographic and Ultrasound Findings in PG and PFG.
| PG | PFG | P | |
| PA-RX | 50 (100%) | 49 (98) | |
| IO-RX | 0.76 | 0.44 | .028 |
| O proximal-lateral | 13 (26%) | 5 (10%) | .039 |
| O proximal-medial | 21 (42%) | 13 (26%) | |
| O distal-lateral | 30 (60%) | 15 (30%) | .001 |
| O distal-medial | 41 (82%) | 31 (26%) | .021 |
| E-RX | 14 (28%) | 7 (14%) | * |
| PA-ECO | 45 (90%) | 44 (88%) | |
| IO-ECO | 0.83 | 0.79 | <.001 |
| O proximal-lateral | 35 (70%) | 31 (61%) | |
| O proximal-medial | 38 (76%) | 32 (64%) | |
| O proximal-dorsal | 24 (48%) | 17 (34%) | .065 |
| O proximal-palmar | 21 (42%) | 16 (32%) | |
| O distal-lateral | 45 (90%) | 44 (88%) | |
| O distal-medial | 44 (88%) | 42 (84%) | |
| O distal-dorsal | 34 (68%) | 30 (60%) | |
| O distal-palmar | 25 (50%) | 26 (52%) | |
| E-ECO | 10 (20%) | 5 (10%) | a |
| S-ECO | 15 (30%) | 6 (12%) | .022 |
| PDS-ECO | 1 (2%) | 0 (0%) | |
| AC-ECO | 15 (30%) | 6 (12%) | .022 |
| QM-ECO | 6 (12%) | 4 (8%) | |
AC: absence of cartilage; E: erosion; IO: osteophyte index; O: osteophytes; PA: joint impingement; PDS: power Doppler synovitis; QM: mucinous cyst; S: synovitis.
The radiological intraobserver agreement was 100% for joint impingement and erosion, and 98% for the osteophyte index. The ultrasound intraobserver agreement was 100% for joint impingement, erosion, synovitis and absence of articular cartilage, and 98% for the osteophyte index.
The analysis of all radiological and ultrasonographic variables grouping the PIP and DIP showed no statistical significance. While the analysis of radiological and ultrasound variables in the 2 cohorts according to age showed that patients aged 60 years or less tended to have a higher rate of ultrasound osteophyte, erosion and synovitis, patients older than 61 years tended to present a greater radiographic osteophyte index and no ultrasound visualization of articular cartilage.
DiscussionThis study, which was conducted in PIP and DIP of 20 women who were skilled manual workers, demonstrated that symptomatic joints (PG) are found mostly (70%) in the dominant hand and exhibit a higher radiological-ultrasound structural damage and inflammation-through-ultrasound than asymptomatic joints (PFG). This clinical–morphological finding indicates that mechanical stress on the dominant hand plays a pathogenic role in osteoarthritis of the fingers and supports some of the few epidemiological studies designed to demonstrate the association between manual activity and osteoarthritis of fingers.6–9
Patients with osteoarthritis of the hands have more ultrasonographic synovitis than healthy controls.1,10 and ultrasonographic synovitis in painful osteoarthritic hands than in painless ones.2,11,12 Keen et al.,2 and Kortekaas et al. studied11 30 hand joints, finding synovitis in approximately 80% of joints in patients with osteoarthritis of the hands, while Arrestier et al.18 studied the interphalangeal joints of the hands, finding synovitis in about 25% of the joints; however, they did not distinguish the asymptomatic from the symptomatic. We found synovitis in 21% of the studied joints, and was significantly higher in the painful joints than in the non-painful (15 vs 6, P=.02). As for intraarticular Doppler signal, this was lower in our study compared with that in the studies by Keen et al.,2 and Kortekaas et al.,11 but similar to the values found in other studies such as Arrestier et al.,12 and Mancarella et al.,10 Unlike previous studies,2,11,12 in our study 98% of the patients were taking NSAIDs, which decreases the detection of synovitis in gray scale and Doppler modes.13,14
The higher spatial resolution of ultrasound versus radiology allows for the detection of osteophytes on the palm and back of fingers not visible using radiology. Like other studies,1,2,15 and especially in the study of Mathiessen et al.,15 which is the largest cohort to date, with 127 patients with osteoarthritis of the hand, ultrasound clearly detected more osteophytes than plain radiography of the hands. Curiously, given that MRI detects few osteophytes in the palm of the hand,16 Mathiessen et al.15 did not include palmar ultrasound examination, while we did include it.
It has been shown that radiographic erosive hand osteoarthritis exhibits more ultrasound B mode and Doppler synovitis than nonerosive cases.11,17,18 We did not differentiate these phenotypes in the inclusion criteria or study it. We found that patients aged 60 years or less tended to have more erosions and synovitis than those aged more than 60 years, which indicates the possibility of differences in the phenotype of the patients.
To date, this pilot study is the first to compare morphological causes of pain in the same patient with osteoarthritis of the fingers. When compared with the same patient, the bias of the patient's personality decreases in the pain assessment. Also, the fact that the clinician seeks the most similar non-painful joint in appearance for comparison reduces bias at the articular level. Kortekaas published 2 different studies; the first demonstrates that synovitis is associated with pain in patients with osteoarthritis of the hand11 and the second shows that both osteophytes and joint space narrowing are independently associated with pain.19 We jointly studied the inflammation and structural damage, observing that painful joints have more synovitis and structural damage on ultrasound with regard to the presence of radiographic osteophytes, as well as the absence of ultrasonographic cartilage, with a trend toward significance in radiological and ultrasound joint erosion, as other authors have indicated.10,19 Although ultrasound articular impingement is a non-standardized qualitative variable, our results suggest that it is not related to pain.
Our study has some drawbacks. On the market there is a shorter, narrower “hockey stick” high frequency B transducer which is easier to use in small joints on Doppler mode. However, a small linear 2.5cm long probe and a high-end ultrasound were employed, as well as a very experienced rheumatologist sonographer. The total number of patients included in the study is small and we believe it is mandatory that our results are confirmed with a larger population.
In conclusion, this work demonstrates that patients with joint pain have major structural damage and ultrasonographic synovitis than those without pain in osteoarthritis of the PIP and DIP. It confirms that ultrasound detected more osteophytes than conventional radiology of the hands. We hope that longitudinal studies of the diagnostic–therapeutic clinical importance are performed to elucidate whether synovitis predicts structural damage in patients with osteoarthritis of the hands or vice versa.
Ethical ResponsibilitiesProtection of persons and animalsThe authors declare that the performed procedures conformed to the ethical standards of the committee responsible for human experimentation and were in accordance with the World Medical Association Declaration of Helsinki.
Data privacyThe authors declare that they have followed the protocols of their workplace on the publication of data from patients, and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
FinancingThe authors declare that this study did not have funding.
Conflict of InterestThe authors declare that they have no conflict of interest.
Please cite this article as: Usón J, Fernández-Espartero C, Villaverde V, Condés E, Godo J, Martínez-Blasco MJ, et al. Artrosis interfalángica sintomática y asintomática: un estudio ecográfico. Reumatol Clin. 2014;10:278–282.