Pulmonary involvement in the form of acute pneumonitis in adult-onset Still's disease (AOSD) is an uncommon manifestation, with few cases reported in the literature. We report the case of a 61-year-old male with 3 years of AOSD evolution, treated with methotrexate (MTX) and half-dose corticosteroids, which debuted with symptoms of fever, dyspnea and dry cough after 3 weeks of receiving the first dose of tocilizumab (TCZ). In the follow-up study showed leukocytosis with left shift, elevated serum ferritin and C-reactive protein standard. The chest CT scan showed ground-glass pattern predominantly in central and upper lobes and the BAL shows an increase in the percentage of lymphocyte with normal subpopulations and negative cultures. MTX and TCM were suspended, prednisone was increased to 30mg/day and within a week Anakinra 100mg/day SC was iniciated, noting in a few days a progressive clinical, analytical and radiological improvement.
La afectación pulmonar en forma de neumonitis aguda en la enfermedad de Still del adulto (ESA) es una manifestación infrecuente, existiendo pocos casos descritos en la literatura. Presentamos el caso de un varón de 61 años con ESA de 3 años de evolución, en tratamiento con metotrexato (MTX) y corticoides a dosis medias, que comenzó con cuadro de fiebre, disnea y tos seca a las 3 semanas de recibir la primera dosis de tocilizumab (TCZ). En la analítica destacaban leucocitosis con desviación izquierda, ferritina sérica muy elevada y proteína C reactiva normal. La TAC de tórax mostró un patrón en vidrio deslustrado de predominio central y lóbulos superiores, y el BAL, un incremento del porcentaje de linfocitos, con subpoblaciones normales y cultivos negativos. Se suspendieron el MTX y el TCZ, se aumentó la prednisona a 30mg/día y al cabo de una semana se inició anakinra 100mg/día por vía subcutánea, observando en pocos días una mejoría progresiva espectacular clínica, analítica y radiológica.
Adult-onset Still's disease (AOSD) is an inflammatory disorder of unknown etiology, characterized by intermittent high fever, a salmon-colored evanescent maculopapular rash, polyarthritis or oligoarthritis, and leukocytosis. These signs are frequently accompanied by odynophagia, adenopathy, hepatosplenomegaly and pleuropericarditis. Pulmonary involvement is uncommon, with an estimated prevalence of between 12% and 53% for pleuritis and from 0 to 7% for interstitial pneumonia.1,2
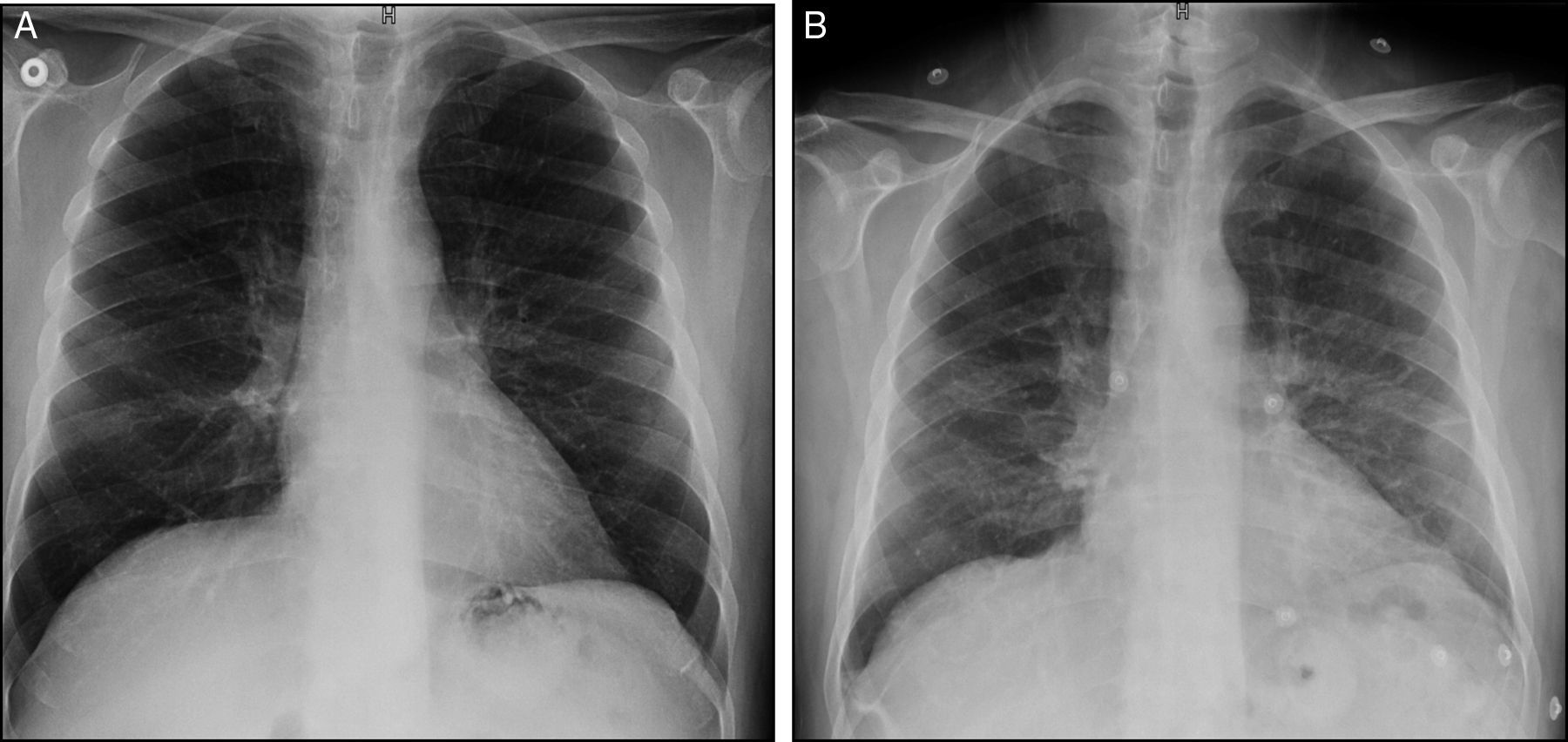
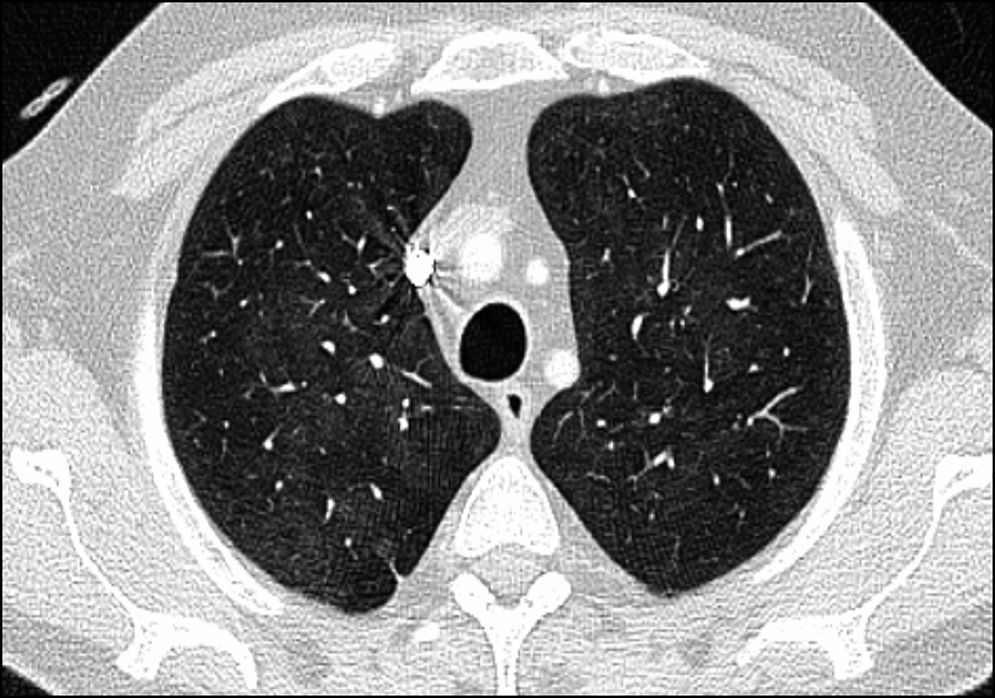
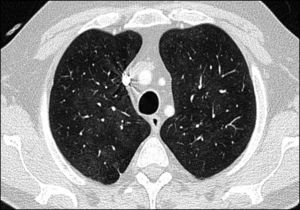
Case ReportThe patient was a 61-year-old man with a personal history of asthma who was diagnosed with AOSD in October 2011. He was initially treated with nonsteroidal anti-inflammatory drugs (NSAID). After 1 month, glucocorticoid (GC) therapy was started because of the development of skin involvement. In March 2012, subcutaneous methotrexate (MTX) was added as a steroid-sparing agent, and was escalated up to 25mg a week. For 2 years, a good control of the disease was achieved and maintained, making it possible to reduce the prednisone dose to 2.5mg/day. However, in November 2014, the patient experienced a severe joint and cutaneous flare that required hospital admission and an increase in corticosteroid therapy. After 1 month, the decision was made to initiate treatment with tocilizumab (TCZ) because of persistent arthralgia, fever and neutrophilic leukocytosis with hyperferritinemia, despite the treatment with MTX and high-dose oral GC. Three weeks after receiving the first and only dose of TCZ at 8mg/kg body weight, he presented to the outpatient clinic with dyspnea on moderate exertion. There was no evidence of infection or cardiac decompensation. The only noteworthy finding on physical examination was a baseline oxygen saturation (SO2) of 93%. An emergency chest radiograph (Fig. 1A) showed a faint image of bilateral interstitial involvement and the patient was referred to the emergency department. The results of the laboratory analyses performed there included a slightly decreased partial pressure of oxygen (PO2) (70.900mmHg), leukocytosis (13.54×103/μL), neutrophilia (11.93×103/μL), lymphopenia (0.59×103/μL), C-reactive protein < 0.5mg/L and elevated D-dimer (1.77μg/mL). The electrocardiogram was normal. Computed tomography (CT) angiography served to rule out pulmonary thromboembolism. However, the lung window (Fig. 2) revealed an increased ground glass density, predominantly in middle and upper lobes, suggestive of alveolar inflammation. In agreement with the pulmonology department, and given that the clinical signs were mild at that time, the decision was made to carry out pulmonary function tests (PFT), to perform a clinical reevaluation over the following days and to discontinue treatment with MTX and TCZ, as we suspected their possible implication in this condition. He returned 2 days later, complaining of a significant deterioration in his clinical status, with the development of fever and a dry cough, and was unable to complete the scheduled PFT. On the other hand, he had been taking amoxicillin/clavulanic acid for the preceding 2 days because of a dental abscess. A chest radiograph performed at that time (Fig. 1B) showed an increase in diffuse density in the region of the hilum and base of the lung. He was admitted to the hospital to complete the study and begin treatment with prednisone at 30mg/day. The laboratory tests revealed a ferritin level of 4023ng/mL (previously 1997ng/mL), C-reactive protein at 17.7mg/L, leukocytosis at 15,280×103/μL, neutrophils at 12,360×103/μL and lymphocytes at 1870×103/μL, there being no other noteworthy findings. Bronchoalveolar lavage revealed an increase in the percentage of lymphocytes, with normal lymphocyte subsets and negative results for cytology and cultures for fungi, cytomegalovirus, herpes, influenza/parainfluenza and adenovirus, and negative staining of acid-alcohol fast bacilli. The PFT disclosed a restrictive change with a reduced diffusing capacity (48%), which was not corrected for at alveolar volume. During his hospital stay, the patient initially required oxygen therapy at 1.5bpm and, subsequently, treatment with subcutaneous anakinra was introduced at 100mg/day. Within a few days, he began to show progressive improvement in both clinical signs and laboratory results, as well as normalization of the radiographic pattern after 10 days and, after 1 month, control of ferritin and CT images.
The percentage of patients with AOSD exhibiting pulmonary involvement in the form of acute pneumonitis is estimated to be quite low. It is characterized by the presence of transient pulmonary infiltrates in upper and lower lobes, often associated with small pleural effusions.3 An infectious process is frequently suspected from the start, especially in immunocompromised patients, as in the case we report here, because of the association with fever, dyspnea and leukocytosis. The absence of a response to antibiotic therapy and negative results in a microbiological study help to rule out this origin. On the other hand, there is a wide variety of drugs that can induce pulmonary toxicity. Thus, concomitant treatment with MTX, which our patient received, was proposed as a possible trigger for the pneumonitis. Methotrexate can produce acute or subacute pneumonitis and, less commonly, chronic pneumonitis, and the incidence of acute pneumonitis in patients being treated with MTX for rheumatic diseases is estimated to be between 0.3% and 8%.4 However, the clinical manifestations (dyspnea, nonproductive cough, fever) usually develop a few days after the initiation of MTX therapy or, less frequently, weeks or months later. We should point out that the patient had been taking MTX for 3 years and had never mentioned respiratory symptoms. On the other hand, he had not shown pulmonary involvement in any of the AOSD flares that he had experienced prior to receiving TCZ, and we were able to review a previous CT study and recent chest radiographs in which no changes were observed. These facts, together with the sudden development of the symptoms following the first dose of TCZ, lead us to think of a highly relevant role of this drug in the development of the pneumonitis or even a possible paradoxical induction of a pulmonary flare of AOSD.
To our knowledge, only 8 cases of pulmonary toxicity allegedly induced by TCZ have been reported to date, most of the patients were receiving monotherapy and all of them had rheumatoid arthritis.5–9 The reported pulmonary involvement was, in one case, the fatal exacerbation of interstitial lung disease associated with rheumatoid arthritis after the initiation of TCZ therapy. In one patient, de novo interstitial lung disease was observed and, in the other, pulmonary fibrosis. Of the 3 cases that were noninfectious, 2 of the patients received concomitant MTX, which was the case of our patient. There has been a case of allergic pneumonitis and another of organizing pneumonia with TCZ.
In short, we report lung involvement in AOSD in therapy with MTX, following treatment with TCZ, a complication that is uncommon and is presented by a satisfactory response to anakinra.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Sangüesa Gómez C, Flores Robles BJ, Jara Chinarro B, Espinosa Malpartida M, Barbadillo Mateos C. Neumonitis aguda en un paciente con enfermedad de Still del adulto tras tratamiento con tocilizumab con buena respuesta a anakinra. Reumatol Clin. 2016;12:345–347.