The patient was a 52-year-old man with a 20-year history of limited scleroderma, as well as antiphospholipid syndrome. He was positive for antinuclear antibodies (1:2560), with a centromere pattern, and for lupus anticoagulant, and was receiving oral anticoagulants due to thrombosis in a lower limb.
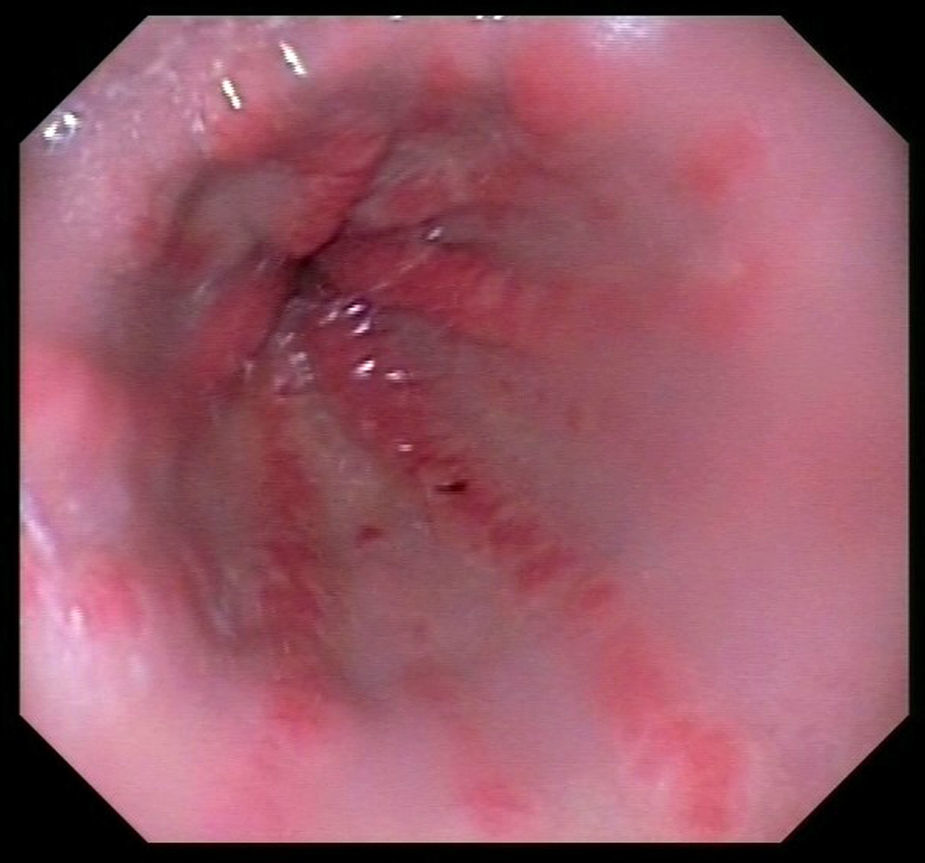
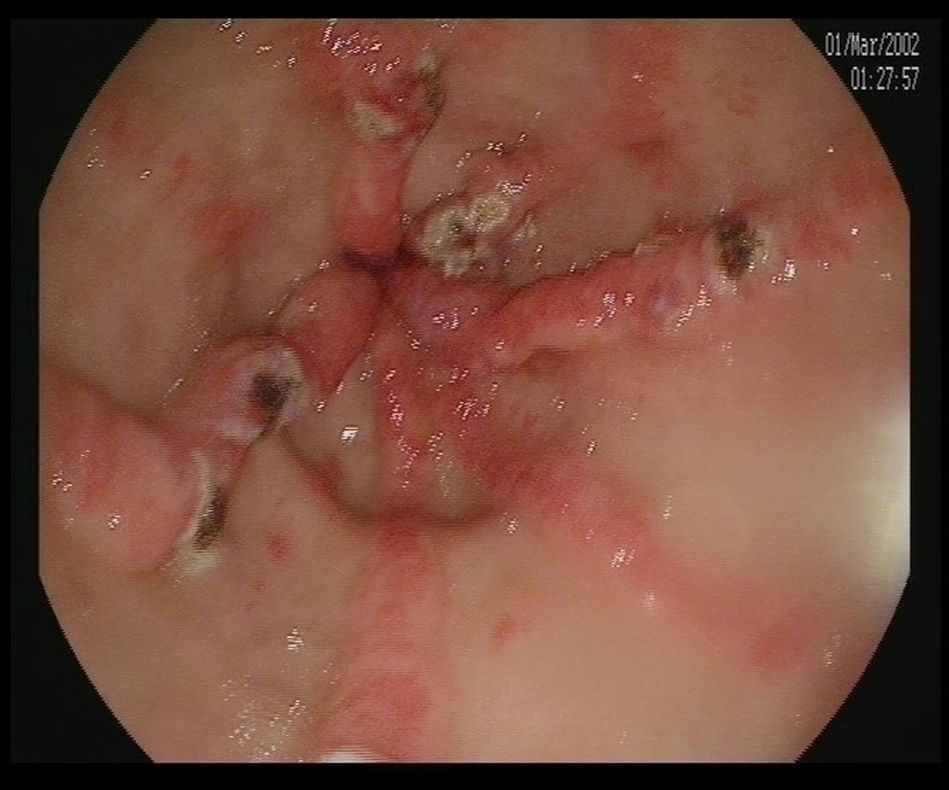
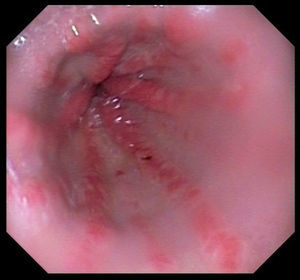
He was admitted to the hospital with an episode of blood in stool and evidence of anemia. Endoscopic study revealed vascular-like lesions in antrum converging as they neared the pylorus, compatible with watermelon stomach1,2 (Fig. 1). In the presence of active bleeding, he was treated with argon plasma coagulation3 (Fig. 2).
Gastric antral vascular ectasia (GAVE) is a rare, but serious, cause of upper gastrointestinal bleeding (4% of all gastric hemorrhages). The endoscopic findings are characteristic: linear images, oriented radially and converging on the pylorus (watermelon stomach1,4).
This condition is associated with underlying chronic diseases, mostly with liver cirrhosis. In autoimmune diseases, it is related to the presence of Raynaud's phenomenon, and is the form most widely reported of the limited subtype of scleroderma (calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, telangiectasia [CREST syndrome]).5,6 The largest series of patients with GAVE includes 45 individuals, 62% of whom also had a connective tissue disease, predominantly with Raynaud's phenomenon (31%) and sclerodactyly (20%).7
The etiology and pathogenesis of GAVE are unknown; one hypothesis is that the histological changes, especially in the lamina propria, are due to a fibromuscular proliferation, vascular dilatation and thrombosis, caused by the vascular disease associated with this condition.8 It can be suspected in patients with scleroderma and iron deficiency anemia who do not respond to iron supplements.
At the present time, we are unable to avoid its development and, given the presence of bleeding, the treatment with the best results is endoscopic, including the use of laser ablation, argon plasma coagulation or cold. With respect to the possible surgical solution, like antrectomy, it can be utilized if other therapies fail.9,10 There are medical treatments if endoscopy cannot be performed, but they are usually associated with more severe adverse effects.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Turrión Nieves AI, Moruno Cruz H, Romero Bogado ML, Perez Gómez A. Hemorragia digestiva alta (estómago watermelon) en paciente con esclerodermia limitada (síndrome de CREST). Reumatol Clin. 2017;13:361–362.