In 2000, Zeitouni et al. updated the diagnostic criteria of Rowell's syndrome (RS).1,2 They included the development of lupus erythematosus (LE) in its systemic, discoid and subacute cutaneous forms, erythema multiforme (EM) and antinuclear antibodies (ANA) (a speckled pattern) as the more important criteria. Moreover, they associated rheumatoid factor (RF), positive anti-Ro/SS-A or anti-La/SS-B antibodies and pernio (chilblains) as less significant criteria.2
The patient was a 91-year-old woman with a 2-month history of generalized itching and painful dermatitis, with a poor response to corticosteroid therapy. She had not had infections or previous use of these medications.
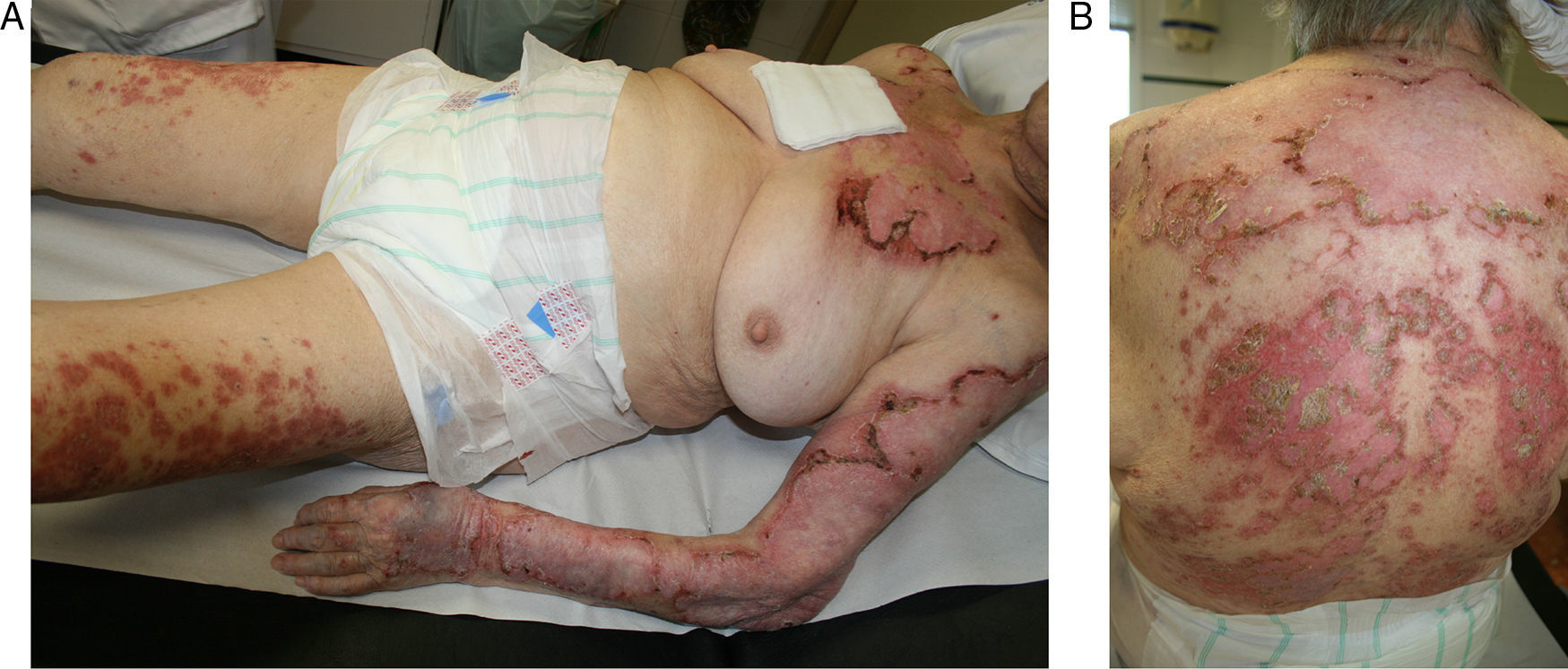
The physical examination showed a scaly, maculopapular eczema, with crusting areas in trunk and all 4 extremities, creating a typical result has shown (Fig. 1A and B).
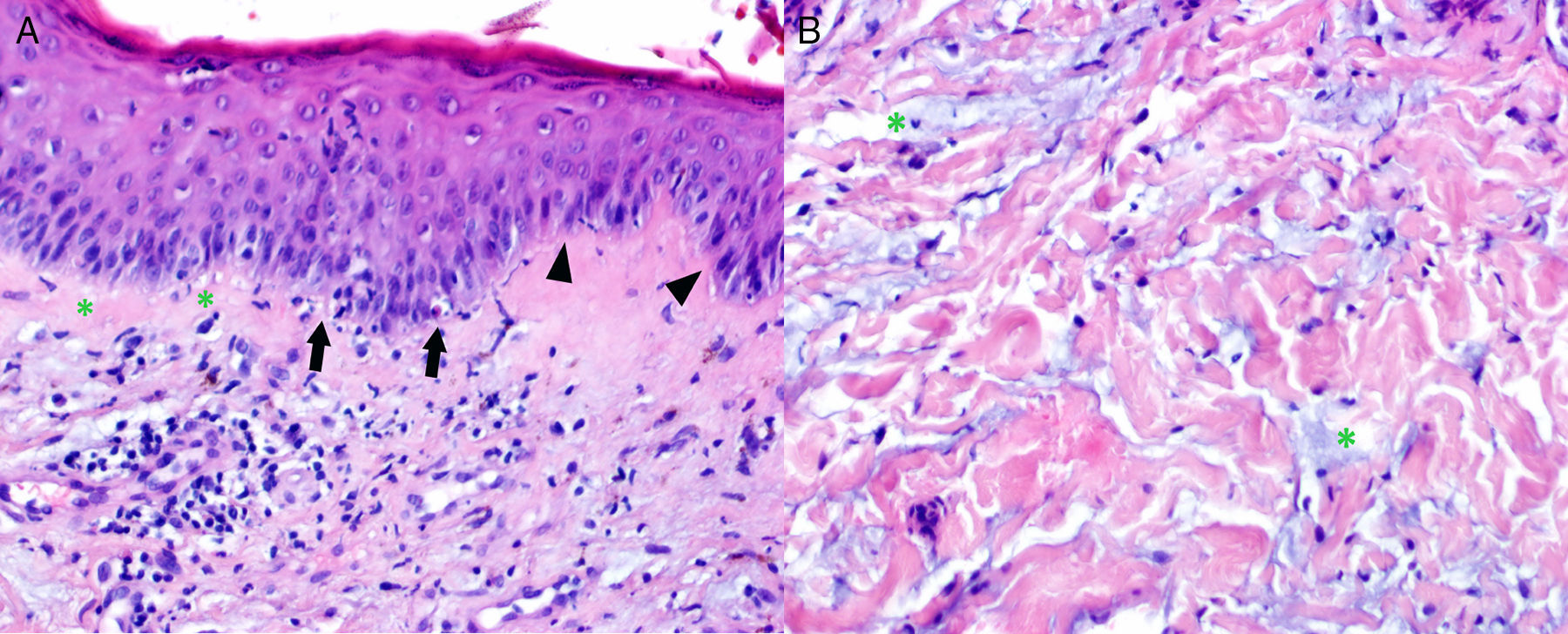
The laboratory tests included RF (83.1IU/mL), ANA (1/2560 speckled pattern) and positive anti-Ro/SSA and anti-La/SSB. The skin biopsy was compatible with LE and EM (Fig. 2A and B).
(A) Epidermis with vacuolar degeneration of the basal cells (asterisks), isolated necrotic keratinocytes (arrows) and associated lymphocyte infiltrate. The image shows the verticality of the basal cells (arrowheads), a histological feature associated with erythema multiforme. Infiltrated lymphocytes and melanophages in papillary dermis. (B) Reticular dermis with interstitial mucin (asterisks).
For some authors, the coexistence of LE and EM are not considered different entities.3
It is difficult to distinguish between subacute cutaneous LE (SCLE) and EM.4,5 However, other authors insist that the classical EM be acute and self-limited, and that the lesions be bull's-eyes. This is commonly associated with infections and previous drug exposure.6,7
In RS, the typical findings are recurrent, EM-like lesions, with no triggering factors and with positive antibodies and RF.7
The speckled pattern of the ANA is the immunological characteristic most consistent of RS, appearing in 60.4% to of the cases, although it is not exclusive of this condition.8 Therapy should be initiated with corticosteroid and hydroxychloroquine. In some cases, success was obtained with dapsone, cyclosporine or azathioprine.9,10
Although the pathological finding is not a diagnostic criterion, it is indispensable for the identification of this disorder.
The diagnostic criteria should be reviewed in order to limit the forms of LE and to assess the need of EM-like lesions without a known triggering agent as essential.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest with regard to this work.
Please cite this article as: López Caleya JF, Martín Rodrigo L, Gonzalvo Rodriguez P, Hidalgo García Y. Síndrome de Rowell: las 2 caras de la verdad. Reumatol Clin. 2016;12:354–355.