To describe the impact of the COVID-19 on the psychosocial health of patients with rheumatoid arthritis (RA), spondyloarthritis (SpA), and systemic lupus erythematosus (SLE).
DesignLongitudinal observational study of a series of patients with rheumatic disease.
MethodsThe main outcome measure was impairment of the ability to participate in social activities, as measured using the PROMIS-APS instrument Short Form-8a. We evaluated social activities in various settings and performed a multivariate analysis to study the association between worsening of social participation during the COVID-19 pandemic and implicated factors.
ResultsOne hundred and twenty-five patients had completed the prospective follow-up: 40 with AR (32%), 42 with SpA (33.6%), and 43 with SLE (34.4%). Overall, poorer mean PROMIS scores were recorded after the COVID-19 pandemic for: satisfaction with social roles (p=0.029), depression (p=0.039), and ability to participate in social activities (p=0.024). The factors associated with ability to participate in social activities after the COVID-19 pandemic were older age (β=−0.215; p=0.012), diagnosis of SLE (β=−0.203; p=0.015), depression (β=−0.295; p=0.003) and satisfaction with social roles (β=0.211; p=0.037).
ConclusionThe ability to participate in social activities after the COVID-19 pandemic is affected in patients with rheumatic disease, especially in SLE.
Describir el impacto de la COVID-19 en la salud psicosocial de los pacientes con artritis reumatoide (AR), espondiloartritis (EspA) y lupus eritematoso sistémico (LES).
DiseñoEstudio observacional longitudinal de una serie de pacientes con enfermedades reumáticas.
MétodosLa principal medida de resultado fue el deterioro de la capacidad para participar en actividades sociales, medido por el instrumento PROMIS-APS Short Form-8a. Evaluamos las actividades sociales en varios entornos y realizamos un análisis multivariado para estudiar la asociación al empeoramiento de la participación social durante la pandemia de COVID-19 y los factores involucrados.
ResultadosCiento veinticinco pacientes completaron el seguimiento prospectivo: 40 con AR (32%), 42 con EspA (33,6%) y 43 con LES (34,4%). En general, se registraron puntuaciones medias PROMIS más bajas después de la pandemia de COVID-19 en: satisfacción con los roles sociales (p=0,029), depresión (p=0,039) y capacidad para participar en actividades sociales (p=0,024). Los factores asociados con la capacidad para participar en actividades sociales después de la pandemia de COVID-19 fueron: edad avanzada (β=−0,215; p=0,012), diagnóstico de LES (β=−0,203; p=0,015), depresión (β=−0,295; p=0,003) y satisfacción con los roles sociales (β=0,211; p=0,037).
ConclusiónLa capacidad de participar en actividades sociales después de la pandemia por COVID-19 se ve afectada en los pacientes con enfermedades reumáticas, especialmente con LES.
Inflammatory rheumatic diseases are characterized by an immune-mediated inflammatory response against various body tissues, especially in joints and neighboring structures. These diseases can cause joint pain, inflammation, and stiffness, leading to functional disability and impaired quality of life.1 Inflammatory rheumatic diseases constitute a well-known public health problem worldwide owing to their morbidity, associated disability, and economic and social consequences.2
The most common inflammatory rheumatic diseases include rheumatoid arthritis (RA), spondyloarthritis (SpA), and systemic lupus erythematosus (SLE). Affected individuals often find it difficult to participate in social activities3 and experience greater social isolation and feelings of loneliness than persons with other diseases and the general population. Social exclusion and more marked stigmatization can affect psychological health, leading to mood disorders and social dissatisfaction.3–5 Consequently, social relationships and support networks play a key role in improving the quality of life of affected patients. In fact, previous studies have shown that social participation is closely linked to patient well-being and quality of life.3,5 Moreover, secondary health conditions, functional deficiencies, and comorbid conditions can affect satisfaction with social roles in up to 52% of patients.6
One of the most widely used tests for evaluating participation in social activities today is the Patient-Reported Outcomes Measurement Information System Ability to Participate in Social Roles (PROMIS-APS) v2.0 Short Form. This instrument has been shown to have suitable measurement properties.7 However, while PROMIS-APS has been used in patients with musculoskeletal disorders,8,9 it was not specifically evaluated in patients with inflammatory rheumatic diseases until a recent study by our research group was published.3
The coronavirus disease (COVID-19) pandemic had a significant impact throughout the world.10 The damage to physical, emotional, and psychological health, especially mental health, seriously affected social life. Social distancing measures and the absence of social activities aimed at preventing the spread of COVID-19 impacted people's social relationships, leading many to experience loneliness and isolation owing to restrictions on visits from relatives and friends. Patients with rheumatic disease were especially concerned by COVID-19, since they had to cancel or postpone medical treatment and found it difficult to access health care services, thus further worsening their situation. Consequently, the prevalence of depression, anxiety, and insomnia increased in patients with rheumatic disease.11 Despite cross-sectional studies that associate anxiety and depression with the impact of the pandemic on the general population,12–14 less is known about the specific impact of the pandemic on participation in social activities by patients with inflammatory rheumatic disease. However, knowledge of this situation could have major implications for improving the quality of life of affected patients and may provide useful information for health care decision making in similar health crises.
We were unable to find longitudinal studies that assessed the ability to participate in social activities measured using PROMIS-APS before and after the pandemic in patients with inflammatory rheumatic disease.
MethodsAimsOur aims were: (a) to assess the influence of socio-sanitary restrictions linked to the COVID-19 pandemic on the capacity to engage in social activities within a cohort of patients with rheumatic diseases, who underwent evaluation in 20193; (b) to detect discrepancies between the pre- and post-pandemic scenarios; and (c) to identify the factors linked to the ability to participate in social activities subsequent to the COVID-19 pandemic.
Study designWe performed a longitudinal observational study of a series of patients with rheumatic disease (RA, SpA, and SLE).
ParticipantsWe consecutively included patients with RA diagnosed according to the criteria of the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) for the classification of RA (2010 revision),15 SpA diagnosed according to the criteria of the Assessment of SpondyloArthritis International Society (ASAS 2010),16 and SLE diagnosed according to the criteria of EULAR/ACR 2019.17 Patients were aged 18–80 years and had participated in the baseline study performed to evaluate social satisfaction using PROMIS-APS in 2019.3 We excluded patients with other inflammatory or rheumatic diseases and patients with difficulties reading, writing, and understanding the questionnaire owing to mental disorders. We also excluded patients who could not complete the questionnaire at the end of the follow-up.
Data collection and definitionsThe main outcome measure was the ability to participate in social activities, as assessed using PROMIS-APS,4 which comprises 8 questions with 35 items. These were used to evaluate the perceived ability to engage in social activities in various settings, such as social roles, depression, companionship, social isolation, emotional support, instrumental support, informational support, and the ability to participate in social activities. PROMIS-APS does not specifically assess specific social activities, but rather dimensions and aspects related to participation in social activities and roles. Scores are numerical and are expressed as the T-score, which is a standard scoring system with a mean of 50 and standard deviation (SD) of 10. A higher score indicates a greater ability to participate in social activities. In the PROMIS-APS “depression” dimension, a higher T-score indicates a greater presence of depressive symptoms. T-scores to provide standardized scores that allow for comparisons against a reference population. These scores help in quantifying the level of an individual's psychosocial health in each of the areas assessed.
As secondary outcome measures, we evaluated other social activities in different settings, as follows: satisfaction with social roles and activities, instrumental support, depression, informational support, ability to participate in social activities, companionship, and social isolation. These measures were obtained using the PROMIS questionnaire and are expressed using quantitative T-scores (SD). All the questionnaires are available at the following link: https://commonfund.nih.gov/promis/index.
We collected demographic, clinical, and therapy-related data as exploratory and additional variables. The information collected included age (in years), sex, ethnic origin, educational level (none, primary, secondary, higher), and socioeconomic level (monthly income <€1000, €1000–1500, and >€1500). We also introduced current cardiovascular risk factors or risk factors requiring treatment before data collection, such as diabetes mellitus, arterial hypertension, dyslipidemia, obesity, and comorbid conditions included in the Charlson comorbidity index.18 Disease activity was assessed for all patients at visits to the Rheumatology Department using the following instruments: 28-joint Disease Activity Score (DAS) with erythrocyte sedimentation rate (DAS28-ESR) for RA,19,20 Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for SpA, and Safety of Estrogens in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index (SELENA-SLEDAI) for SLE.21 We also classified patients according to inflammatory activity as low activity (DAS28-ESR <3.2 for RA, BASDAI <4 for SpA, and SELENA-SLEDAI <3 for SLE) and as high activity (DAS28-ESR ≥3.2 for RA, BASDAI ≥4 for SpA, and SELENA-SLEDAI ≥3 for SLE).
ProceduresPatients who fulfilled the inclusion criteria completed the PROMIS-APS instrument in person between June and December 2021, after previously giving their informed consent to participate. The results were compared with those of the same PROMIS-APS questionnaire they had completed in 2019 in order to determine whether there were significant differences in disease impact on social relationships after the COVID-19 pandemic.
Statistical analysisWe performed a descriptive analysis. Qualitative variables are expressed as absolute numbers and percentages; quantitative variables are expressed as mean and standard deviation or median and interquartile range (depending on the normality of the distribution). The fit of continuous variables to the normal distribution was assessed using the Kolmogorov–Smirnov test. The χ2 test and ANOVA or the Kruskal–Wallis test (depending on the normality of the distribution) were applied to compare the main characteristics between the three groups of patients (RA, SpA, and SLE). Changes in PROMIS-APS scores from baseline to 24 months were assessed using the paired t-test or Wilcoxon test, as appropriate. The first multiple linear regression model was then applied to study factors that were independently associated with impaired ability to participate in social activities for all patients with rheumatic disease (continuous dependent variable: ability to participate in social activities). Because SLE patients experienced the greatest post-pandemic changes, a second model was applied in these patients. Statistical significance was set at two-tailed p<0.05 for all the analyses, which were performed using SPSS 22.0 for MAC OS X (IBM Corp.) (property of the University of Málaga).
ResultsBetween June and December 2021, we prospectively followed up 151 patients with rheumatic diseases who had completed the questionnaire before the pandemic. A total of 125 patients completed the post-COVID-19 follow-up questionnaire (40 with RA [32%], 42 with SpA [33.6%], and 43 with SLE [34.4%]). Furthermore, 26/151 patients (17.2%) were excluded owing to loss to follow-up (2 patients died, 5 patients changed autonomous community or hospital, and 19 patients did not wish to complete the post-COVID-19 questionnaire).
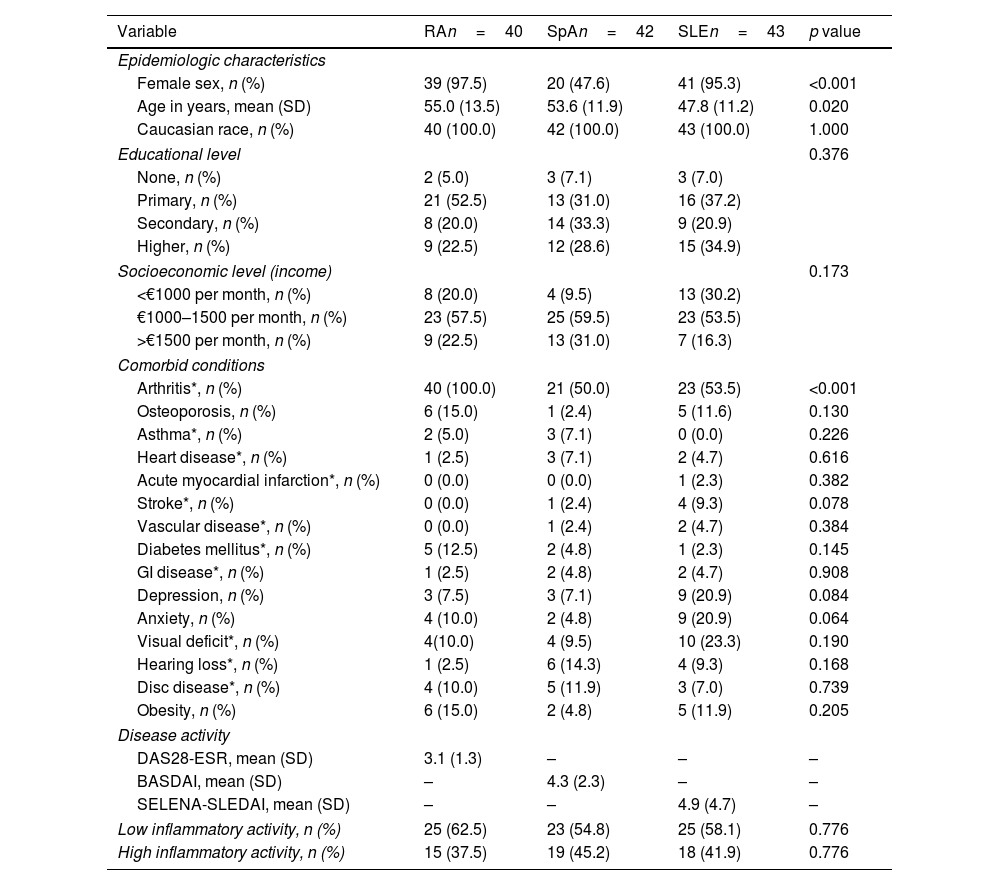
Study sampleThe baseline characteristics of the patients included are shown according to disease in Table 1. More women than men had RA and SLE (p<0.001), but not SpA, and the mean (SD) age was significantly lower for patients with SLE than for those with RA and SpA (p=0.020). No significant differences were found between the groups for socioeconomic or educational level, or for most of the comorbid conditions analyzed, except for arthritis, which was more prevalent in patients with RA than in the other groups (p<0.001). Inflammatory activity in patients with RA and SLE was low on average or in remission according to the indices applied (DAS28-ESR and SELENA-SLEDAI), whereas that of SpA was, on average, moderate according to the BASDAI.
Baseline clinical characteristics of 125 patients with rheumatic disease.
| Variable | RAn=40 | SpAn=42 | SLEn=43 | p value |
|---|---|---|---|---|
| Epidemiologic characteristics | ||||
| Female sex, n (%) | 39 (97.5) | 20 (47.6) | 41 (95.3) | <0.001 |
| Age in years, mean (SD) | 55.0 (13.5) | 53.6 (11.9) | 47.8 (11.2) | 0.020 |
| Caucasian race, n (%) | 40 (100.0) | 42 (100.0) | 43 (100.0) | 1.000 |
| Educational level | 0.376 | |||
| None, n (%) | 2 (5.0) | 3 (7.1) | 3 (7.0) | |
| Primary, n (%) | 21 (52.5) | 13 (31.0) | 16 (37.2) | |
| Secondary, n (%) | 8 (20.0) | 14 (33.3) | 9 (20.9) | |
| Higher, n (%) | 9 (22.5) | 12 (28.6) | 15 (34.9) | |
| Socioeconomic level (income) | 0.173 | |||
| <€1000 per month, n (%) | 8 (20.0) | 4 (9.5) | 13 (30.2) | |
| €1000–1500 per month, n (%) | 23 (57.5) | 25 (59.5) | 23 (53.5) | |
| >€1500 per month, n (%) | 9 (22.5) | 13 (31.0) | 7 (16.3) | |
| Comorbid conditions | ||||
| Arthritis*, n (%) | 40 (100.0) | 21 (50.0) | 23 (53.5) | <0.001 |
| Osteoporosis, n (%) | 6 (15.0) | 1 (2.4) | 5 (11.6) | 0.130 |
| Asthma*, n (%) | 2 (5.0) | 3 (7.1) | 0 (0.0) | 0.226 |
| Heart disease*, n (%) | 1 (2.5) | 3 (7.1) | 2 (4.7) | 0.616 |
| Acute myocardial infarction*, n (%) | 0 (0.0) | 0 (0.0) | 1 (2.3) | 0.382 |
| Stroke*, n (%) | 0 (0.0) | 1 (2.4) | 4 (9.3) | 0.078 |
| Vascular disease*, n (%) | 0 (0.0) | 1 (2.4) | 2 (4.7) | 0.384 |
| Diabetes mellitus*, n (%) | 5 (12.5) | 2 (4.8) | 1 (2.3) | 0.145 |
| GI disease*, n (%) | 1 (2.5) | 2 (4.8) | 2 (4.7) | 0.908 |
| Depression, n (%) | 3 (7.5) | 3 (7.1) | 9 (20.9) | 0.084 |
| Anxiety, n (%) | 4 (10.0) | 2 (4.8) | 9 (20.9) | 0.064 |
| Visual deficit*, n (%) | 4(10.0) | 4 (9.5) | 10 (23.3) | 0.190 |
| Hearing loss*, n (%) | 1 (2.5) | 6 (14.3) | 4 (9.3) | 0.168 |
| Disc disease*, n (%) | 4 (10.0) | 5 (11.9) | 3 (7.0) | 0.739 |
| Obesity, n (%) | 6 (15.0) | 2 (4.8) | 5 (11.9) | 0.205 |
| Disease activity | ||||
| DAS28-ESR, mean (SD) | 3.1 (1.3) | – | – | – |
| BASDAI, mean (SD) | – | 4.3 (2.3) | – | – |
| SELENA-SLEDAI, mean (SD) | – | – | 4.9 (4.7) | – |
| Low inflammatory activity, n (%) | 25 (62.5) | 23 (54.8) | 25 (58.1) | 0.776 |
| High inflammatory activity, n (%) | 15 (37.5) | 19 (45.2) | 18 (41.9) | 0.776 |
Abbreviations: RA: rheumatoid arthritis; SpA: spondyloarthritis; SLE: systemic lupus erythematosus; GI: gastrointestinal; DAS28-ESR: 28-joint Disease Activity Score-erythrocyte sedimentation rate; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; SELENA-SLEDAI: Safety of Estrogens in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index.
At the end of follow-up, no significant differences were found with baseline for most of the epidemiological characteristics, comorbid conditions, or inflammatory activity (Supplementary Table 1), except, as was to be expected, that mean age was higher (p<0.001).
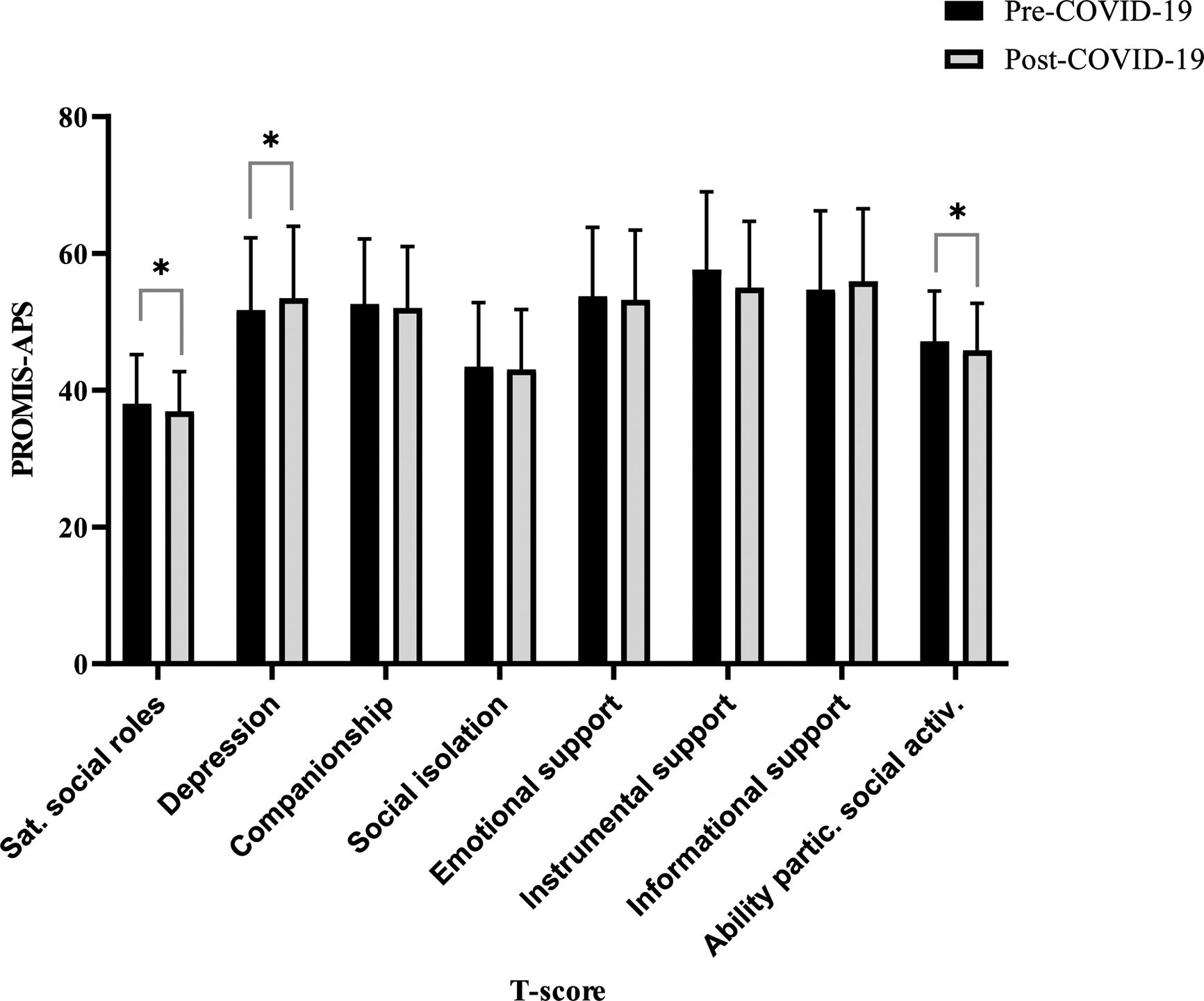
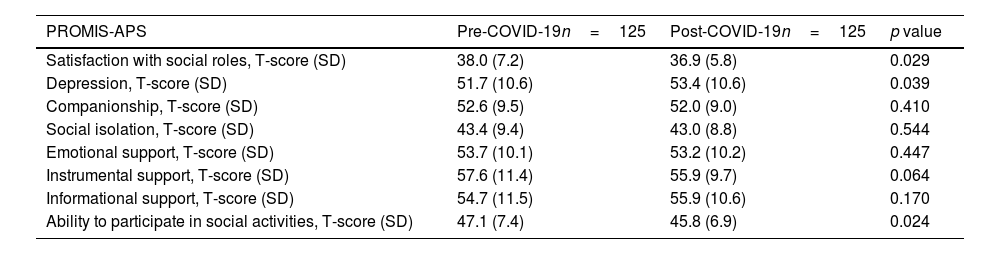
Ability to participate in social activitiesTable 2 and Fig. 1 show the results from the social questionnaires analyzed before and after the COVID-19 pandemic for the whole sample. The PROMIS-APS scores worsened after the pandemic for satisfaction with social roles (T-score mean [SD]=38.0 [7.2] vs 36.8 [5.9]; p=0.029), depression (T-score mean [SD]=51.7 [10.6] vs 53.4 [10.6]; p=0.039), and ability to participate in social activities (T-score mean [SD]=47.1 [7.4] vs 45.8 [6.9]; p=0.024).
Results for social questionnaires analyzed before and after the COVID-19 pandemic in patients with rheumatic disease.
| PROMIS-APS | Pre-COVID-19n=125 | Post-COVID-19n=125 | p value |
|---|---|---|---|
| Satisfaction with social roles, T-score (SD) | 38.0 (7.2) | 36.9 (5.8) | 0.029 |
| Depression, T-score (SD) | 51.7 (10.6) | 53.4 (10.6) | 0.039 |
| Companionship, T-score (SD) | 52.6 (9.5) | 52.0 (9.0) | 0.410 |
| Social isolation, T-score (SD) | 43.4 (9.4) | 43.0 (8.8) | 0.544 |
| Emotional support, T-score (SD) | 53.7 (10.1) | 53.2 (10.2) | 0.447 |
| Instrumental support, T-score (SD) | 57.6 (11.4) | 55.9 (9.7) | 0.064 |
| Informational support, T-score (SD) | 54.7 (11.5) | 55.9 (10.6) | 0.170 |
| Ability to participate in social activities, T-score (SD) | 47.1 (7.4) | 45.8 (6.9) | 0.024 |
Abbreviation: SD: standard deviation.
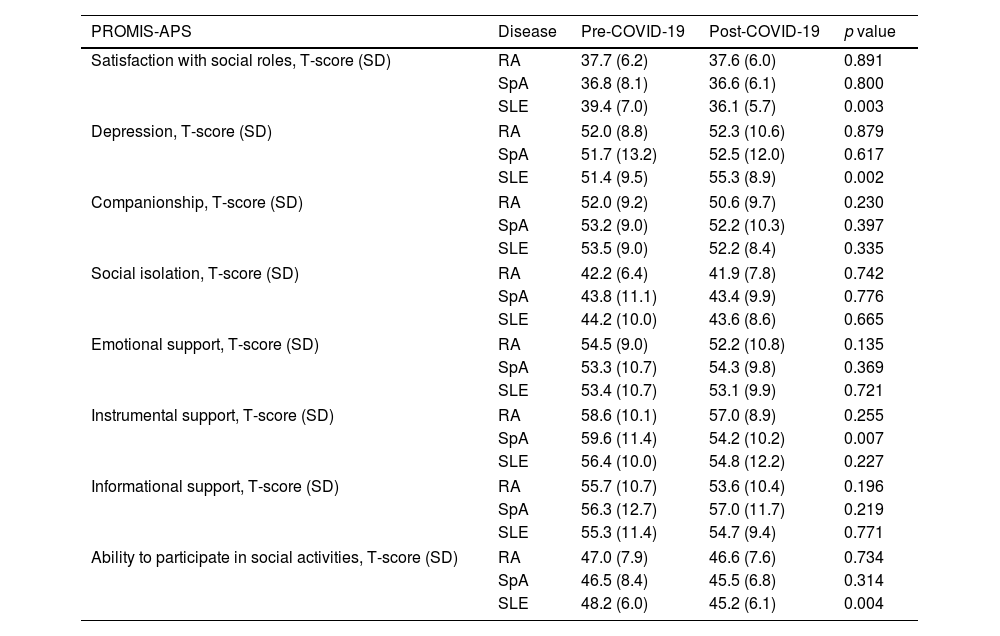
Table 3 shows the results comparing the three rheumatic diseases. As shown, patients with SLE worsened the most with social isolation measures compared to the other patients. Patients with SLE worsened more in satisfaction with social roles (T-score mean [SD]=39.4 [7.0] vs 36.1 [5.7]; p=0.003), depression (T-score mean [SD]=51.4 [9.5] vs 55.3 [8.9]; p=0.002), and the ability to participate in social activities (T-score mean [SD]=48.2 [6.0] vs 45.2 [6.1]; p=0.004). Furthermore, according to the PROMIS-APS values, instrumental support was worse among patients with SpA (T-score mean [SD]=59.6 [11.4] vs 54.2 [10.2]; p=0.007). No significant differences were found in the PROMIS-APS values between patient subgroups at baseline or after the COVID-19 pandemic (Table 3).
Social questionnaires analyzed before and after the COVID-19 pandemic in different types of rheumatic disease.
| PROMIS-APS | Disease | Pre-COVID-19 | Post-COVID-19 | p value |
|---|---|---|---|---|
| Satisfaction with social roles, T-score (SD) | RA | 37.7 (6.2) | 37.6 (6.0) | 0.891 |
| SpA | 36.8 (8.1) | 36.6 (6.1) | 0.800 | |
| SLE | 39.4 (7.0) | 36.1 (5.7) | 0.003 | |
| Depression, T-score (SD) | RA | 52.0 (8.8) | 52.3 (10.6) | 0.879 |
| SpA | 51.7 (13.2) | 52.5 (12.0) | 0.617 | |
| SLE | 51.4 (9.5) | 55.3 (8.9) | 0.002 | |
| Companionship, T-score (SD) | RA | 52.0 (9.2) | 50.6 (9.7) | 0.230 |
| SpA | 53.2 (9.0) | 52.2 (10.3) | 0.397 | |
| SLE | 53.5 (9.0) | 52.2 (8.4) | 0.335 | |
| Social isolation, T-score (SD) | RA | 42.2 (6.4) | 41.9 (7.8) | 0.742 |
| SpA | 43.8 (11.1) | 43.4 (9.9) | 0.776 | |
| SLE | 44.2 (10.0) | 43.6 (8.6) | 0.665 | |
| Emotional support, T-score (SD) | RA | 54.5 (9.0) | 52.2 (10.8) | 0.135 |
| SpA | 53.3 (10.7) | 54.3 (9.8) | 0.369 | |
| SLE | 53.4 (10.7) | 53.1 (9.9) | 0.721 | |
| Instrumental support, T-score (SD) | RA | 58.6 (10.1) | 57.0 (8.9) | 0.255 |
| SpA | 59.6 (11.4) | 54.2 (10.2) | 0.007 | |
| SLE | 56.4 (10.0) | 54.8 (12.2) | 0.227 | |
| Informational support, T-score (SD) | RA | 55.7 (10.7) | 53.6 (10.4) | 0.196 |
| SpA | 56.3 (12.7) | 57.0 (11.7) | 0.219 | |
| SLE | 55.3 (11.4) | 54.7 (9.4) | 0.771 | |
| Ability to participate in social activities, T-score (SD) | RA | 47.0 (7.9) | 46.6 (7.6) | 0.734 |
| SpA | 46.5 (8.4) | 45.5 (6.8) | 0.314 | |
| SLE | 48.2 (6.0) | 45.2 (6.1) | 0.004 | |
Abbreviations: RA: rheumatoid arthritis; SpA: spondyloarthritis; SLE: systemic lupus erythematosus.
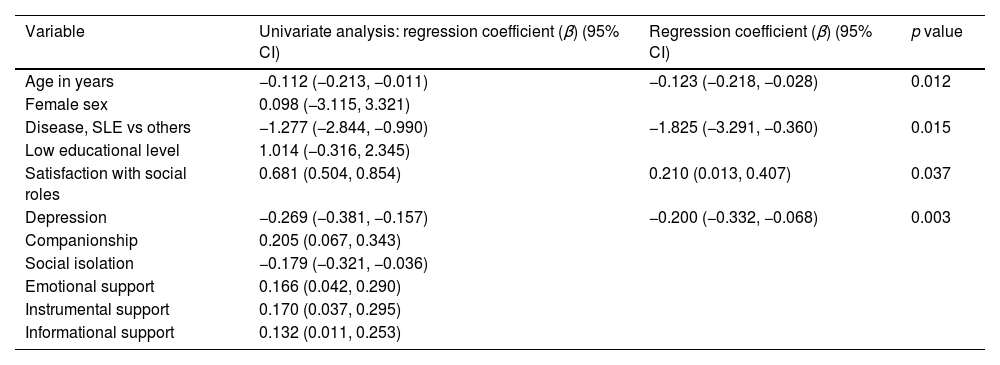
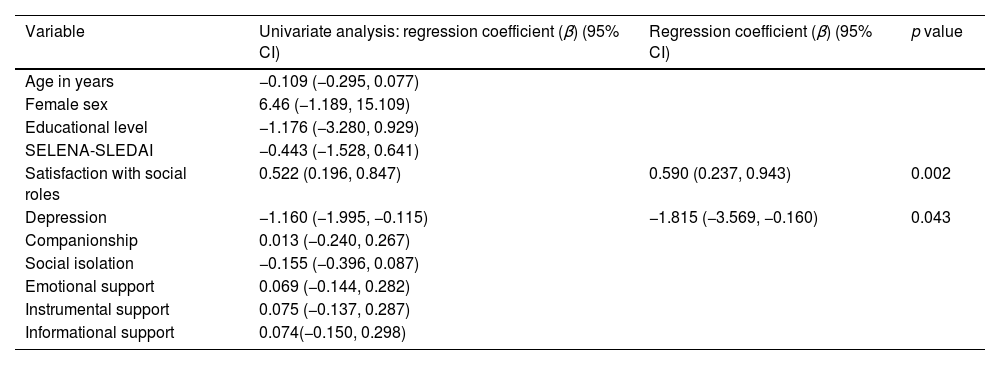
Table 4 shows the results of the multivariate linear regression analysis for the sample of patients with rheumatic disease included in the study. The dependent variable was ability to participate in social activities after the COVID-19 pandemic. We observed an independent, inverse association between ability to participate in social activities and age (β=−0.215; p=0.012), diagnosis of SLE vs other rheumatic diseases (β=−0.203; p=0.015), and depression (β=−0.295; p=0.003), whereas a direct association was found with satisfaction with social roles (β=0.211; p=0.037). Table 5 shows the results of the multivariate linear regression analysis of patients with SLE (dependent variable, ability to participate in social activities). We found an independent and direct association between ability to participate in social activities and satisfaction with social roles (β=0.505; p=0.002) and an independent and inverse association with depression (β=−0.319; p=0.043).
Multiple linear regression analysis of the characteristics associated with participation in social activities after the COVID-19 pandemic in patients with rheumatic disease.
| Variable | Univariate analysis: regression coefficient (β) (95% CI) | Regression coefficient (β) (95% CI) | p value |
|---|---|---|---|
| Age in years | −0.112 (−0.213, −0.011) | −0.123 (−0.218, −0.028) | 0.012 |
| Female sex | 0.098 (−3.115, 3.321) | ||
| Disease, SLE vs others | −1.277 (−2.844, −0.990) | −1.825 (−3.291, −0.360) | 0.015 |
| Low educational level | 1.014 (−0.316, 2.345) | ||
| Satisfaction with social roles | 0.681 (0.504, 0.854) | 0.210 (0.013, 0.407) | 0.037 |
| Depression | −0.269 (−0.381, −0.157) | −0.200 (−0.332, −0.068) | 0.003 |
| Companionship | 0.205 (0.067, 0.343) | ||
| Social isolation | −0.179 (−0.321, −0.036) | ||
| Emotional support | 0.166 (0.042, 0.290) | ||
| Instrumental support | 0.170 (0.037, 0.295) | ||
| Informational support | 0.132 (0.011, 0.253) |
Nagelkerke R2=0.243.
The variables included in the equation were as follows: sex, age, socioeconomic level, type of disease, satisfaction with social roles, depression, companionship, social isolation, emotional support, instrumental support, and informational support.
Abbreviation: SLE: systemic lupus erythematosus.
Multiple linear regression analysis of the characteristics associated with ability of SLE patients to participate in social activities after the COVID-19 pandemic.
| Variable | Univariate analysis: regression coefficient (β) (95% CI) | Regression coefficient (β) (95% CI) | p value |
|---|---|---|---|
| Age in years | −0.109 (−0.295, 0.077) | ||
| Female sex | 6.46 (−1.189, 15.109) | ||
| Educational level | −1.176 (−3.280, 0.929) | ||
| SELENA-SLEDAI | −0.443 (−1.528, 0.641) | ||
| Satisfaction with social roles | 0.522 (0.196, 0.847) | 0.590 (0.237, 0.943) | 0.002 |
| Depression | −1.160 (−1.995, −0.115) | −1.815 (−3.569, −0.160) | 0.043 |
| Companionship | 0.013 (−0.240, 0.267) | ||
| Social isolation | −0.155 (−0.396, 0.087) | ||
| Emotional support | 0.069 (−0.144, 0.282) | ||
| Instrumental support | 0.075 (−0.137, 0.287) | ||
| Informational support | 0.074(−0.150, 0.298) |
Nagelkerke R2=0.286.
The variables included in the equation were as follows: sex, age, SELENA-SLEDAI, satisfaction with social roles, depression, companionship, social isolation, emotional support, instrumental support, and informational support.
Abbreviation: SELENA-SLEDAI: Safety of Estrogens in Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index.
Interpersonal relationships and participation in social activities play an important role in various health domains.22 In the general population, changes in the ability to participate in social activities have been associated with poorer quality of life and increased morbidity.23
The Spanish government declared the state of emergency for the whole of Spain on March 14, 2020, with the aim of managing the health care crisis brought about by the COVID-19 pandemic. The declaration obliged the population to remain at home until early May, when progressive de-escalation was implemented. This lasted until June 21, 2020, in a period known as the “new normal”. Nevertheless, during 2020 and 2021, fresh restrictions on social interaction and mobility were implemented at different times depending on the progress of the pandemic in Spain. The measures taken led to a series of social, health, and psychological situations whose impact remains difficult to assess in the medium and long terms. While the situation affected the whole population, its repercussions were greater in sick people, including persons with rheumatic disease receiving immunosuppressants.24–26
The objective of the present study was to prospectively evaluate the impact of the COVID-19 pandemic on the psychosocial health of patients with RA, SpA, and SLE using validated questionnaires. Fortunately, this group of patients had been evaluated immediately before the declaration of the state of emergency in Spain.3 Patients were followed up between June and December 2021, immediately after the beginning of the “new normal”. Therefore, our findings can help to identify mental health problems, design coping strategies, and improve patient quality of life.
Based on this approach, we observed a decrease in the mean PROMIS-APS scores for satisfaction with social roles, depression, and ability to participate in social activities because of the measures restricting social interaction put in place during the COVID-19 pandemic. In this sense, our data are consistent with those reported in the literature, since patients with rheumatic diseases tend to experience more psychological problems such as depression, anxiety, insomnia, and difficulty adapting to and participating in social life; the COVID-19 pandemic may have acted as a trigger of these conditions.27,28 Before the pandemic, social isolation had already been associated with higher rates of premature morbidity and mortality in persons with rheumatic disease.4 In addition, the pandemic affected mental health and increased isolation among the population in general29 and among patients with rheumatic disease in particular.27 Therefore, lockdown has clearly increased psychological and social malaise in these patients.
Also noteworthy, our findings revealed factors associated with impairment of the ability to participate in social activities after COVID-19. Among the independent factors affecting the three groups, greater vulnerability to problems participating in social activities was more frequently observed in patients with SLE than in patients with RA or SpA. In addition, age, satisfaction with social roles, and depression also had a significant impact on the ability of patients with rheumatic disease to participate in social activities after the COVID-19 pandemic. Thus, in their cross-sectional study of patients with SLE performed in 2021, Kim et al.30 found that pain, fatigue, and impaired cognitive function reduced participation in social, work, family, and leisure activities, as measured using PROMIS-APS. The chronic nature and severity of the disease frequently lead to psychological symptoms such as anxiety, depression, and diminished quality of life, with a serious impact on self-esteem and social skills. Furthermore, several studies on SLE report that patients are misunderstood and stigmatized by their relatives, friends, and doctors, thus further intensifying their feelings of isolation.8,9,31 In addition, Drenkard et al.32 confirmed that social isolation and stigmatization lead to depression in affected patients.
Depression was also an independent factor associated with reduced ability to participate in social activities after COVID-19, both for the sample as a whole and for patients with SLE. This finding is consistent with those reported by Ingegnoli et al.,33 who studied patients with various rheumatic diseases in order to evaluate their psychological well-being. The results showed that mood worsened in patients with anxiety or depression before the pandemic, thus necessitating an increase in their antidepressive and anxiolytic medication. Moreover, during lockdown, the mental and physical health of patients with SLE worsened significantly. Another cross-sectional study compared a group of women with SLE during lockdown to a different group evaluated before the pandemic and found a significant increase in levels of depression, anxiety, phobia, obsession, somatization, interpersonal sensitivity, and psychoticism. Furthermore, almost half of the patients experienced inflammatory flares of their disease during this period, suggesting that psychopathologic symptoms may have contributed to onset. The study highlighted the importance of addressing psychosocial aspects in patients with SLE during the pandemic and in situations of lockdown.34
Regarding satisfaction with social roles and ability to participate in social activities, our results reveal a change after the pandemic. A study by Eriksen et al.35 during the same period found that patients with rheumatic disease felt more isolated than healthy persons. This isolation, which was caused by the fear of infection by COVID-19, may have affected behavior, satisfaction with social roles, and emotional well-being. Similarly, van Genderen et al.36 showed that patients with SpA experienced greater physical difficulties and lower satisfaction in their interpersonal relationships and leisure activities than healthy individuals. These factors were significantly associated with poorer quality of life in patients with SpA, thus underscoring the importance of evaluating satisfaction with social roles and ability to participate in social activities in this group of patients. Finally, the relationship between older age and ability to participate in social activities and social isolation after the pandemic has also been observed in studies performed in the general population.37 This has been associated with greater physical and psychological vulnerability in older patients, who tend to be more dependent and more at risk of anxiety and depression.
Our study has both strengths and limitations. With respect to strengths, we must highlight that, to date, studies performed in the setting of the COVID-19 pandemic in patients with rheumatic diseases are cross-sectional. We were unable to find well-structured longitudinal studies based on PROMIS that take into account the pre- and post-COVID-19 periods in this population.
Our study is limited by its small sample size. It is also limited by losses during the prospective follow-up, indicating that results for some of the participants most affected by the pandemic may be missing. The influence of this limitation is difficult to predict in this setting. Notwithstanding, we did find significant differences in the sample analyzed, and, in any case, no similar studies have been performed under these conditions. Furthermore, losses were lower than 20% of the original sample, which could be considered admissible in this type of study, especially in such a socially complicated context.
Our study was also limited by the fact that, to date, PROMIS-APS has not been validated for rheumatic disease. Nevertheless, it has been shown to have good measurement properties in patients with musculoskeletal disease.8,9 Moreover, the association between the PROMIS-APS questionnaires and PROMIS-APS scores for participation in different social activities in affected patients had already been evaluated in our previous study,3 as well as in the present one, thus indicating the validity of these instruments. Another limitation of our study was the absence of a control group, which would have enabled us to exclusively attribute the observed changes to the COVID-19 pandemic. Nonetheless, given the longitudinal nature of the study, each patient essentially acted as an internal reference. Furthermore, the scoring system of the PROMIS-APS questionnaires involves the use of T-scores. These T-scores offer a standardized metric compared against a comprehensive and diverse normative reference population, facilitating the evaluation of individual scores. Finally, it is noteworthy that the questionnaires were completed in person, not online. While online data collection has the advantage of being easier to administer and process, it has the drawback of a lower response rate and greater probability of selection bias than in-person collection.
ConclusionsIn conclusion, our results reveal a significant and lasting psychosocial impact of the COVID-19 pandemic on patients with rheumatic diseases, particularly those with SLE. Age, SLE diagnosis, and depression were inversely associated with the ability to participate in social activities, while satisfaction with social roles had a positive association. These findings emphasize the importance of continuous evaluation of mental and social health in patients with rheumatic diseases, especially in times of greater social isolation such as the post-pandemic era. Addressing these factors is essential to meet the psychosocial needs of these patients, which must be reinforced by providing continuous support and personalized nursing interventions to improve the participation of patients with rheumatic diseases in social activities and improve their quality of life. This study adds value to the published literature by addressing a relevant research question and employing a robust study design. The results can be valuable healthcare professionals and researchers dealing with patients with rheumatic diseases, especially in the context of social isolation.
Ethical approvalThe study was approved by the Clinical Research Ethics Committee of Hospital Regional Universitario de Málaga (Code. No. 2062-N-19).
FundingRRR was supported by a “Rio Hortega” contract (CM21/00252) from the ISCIII-Madrid (Spain), co-funded by the Fondo Europeo de Desarrollo Regional-FEDER.
JMLM was supported by the “Ayuda de Garantía Juvenil 2020” of the University of Malaga, Spain (SNGJ5Y6-12); AMR was supported by the “Redes de Investigación Cooperativa Orientadas a Resultados en Salud (RICORS)-ISCIII, Red de Enfermedades Inflamatorias (REI) (RD21/0002/0037). Fondos de Next Generation EU, que financian las actuaciones del Mecanismo para la Recuperación y la 4 Resiliencia (MRR).
Conflicts of interestThe authors declare no conflict of interest.
The authors thank the Spanish Foundation of Rheumatology for providing medical writing/editorial assistance during the preparation of the manuscript. FERBT2021