A 62 year old male presented with long-term back pain, which was inflammatory/mixed in rhythm and had been progressively worsening. He also presented with pain in his hips, knees, and feet, with no other signs or symptoms of osteoarthritis.
Physical examination of the patient revealed that his movement was limited in all axes and Schöber's test was 3cm.
Our hospital performed X-rays of the cervical, dorsal, lumbar and pelvic spine which showed a calcification of the anterior common vertebral ligament with preservation of the disc spaces (Figs. 1 and 2).
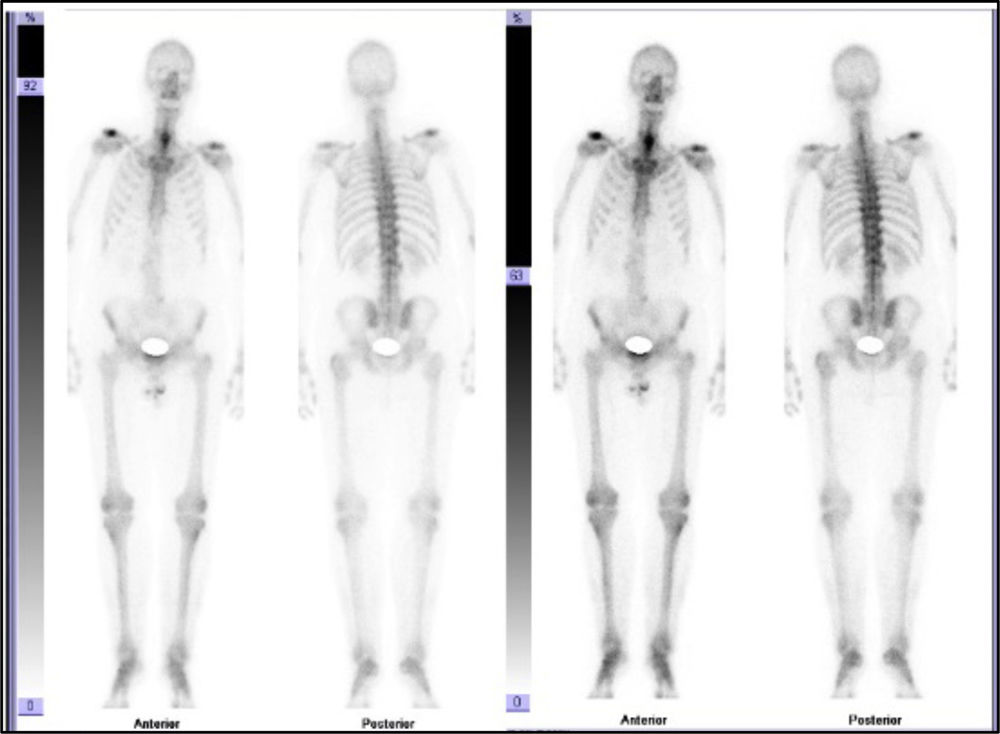
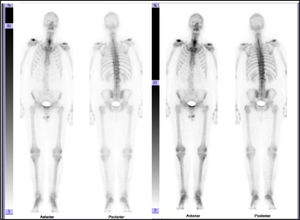
In view of these findings the patient was referred to the nuclear medical unit for a bone scan to rule out several causes of osteoarthritis, Forestier's disease among them.
Forestier's disease is related to abnormal bone growth.1–3 The main disease symptoms is calcification of the longitudinal ligaments of the spine, involving at least 4 contiguous vertebrae. Other criteria are the preservation of intervertebral disc spaces and the absence of inflammatory changes in intrapophysary or sacroiliac joints.4–6
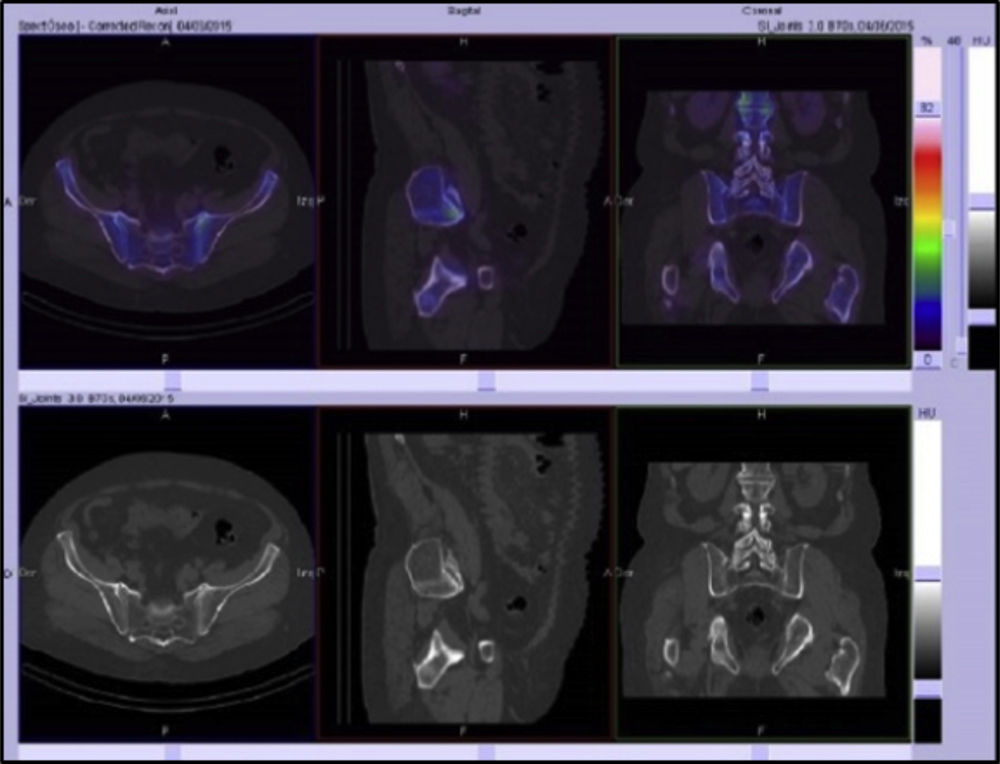
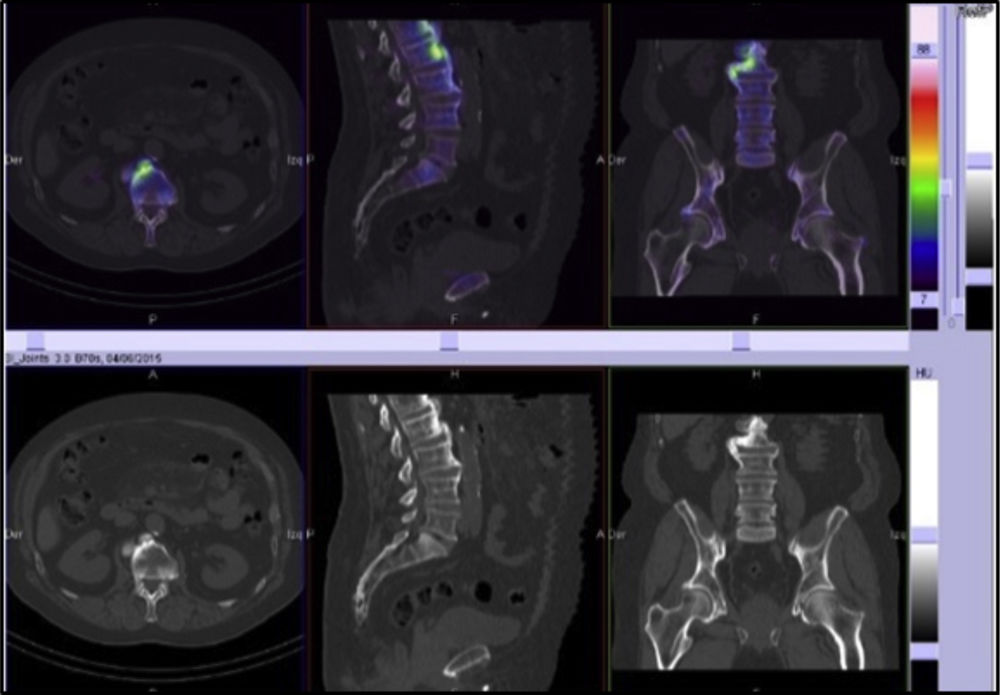
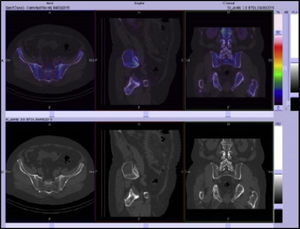
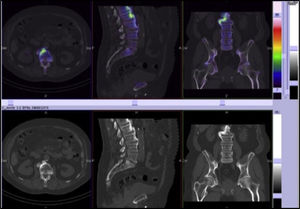
In the bone scan images there was no sign of articular pathological uptake (Fig. 3). Multimodality SPECT/CT tomographic images were then acquired (Figs. 4 and 5), which were used both for qualitative visual analysis of the sacroiliac joint, and for quantitative analysis which permitted the obtainment of indicators of the sacroiliac-promontory. In visual analysis calcification of the anterior common vertebral ligament was detected, together with absence of sacroiliac uptake. With this information and inferior promontory-sacroiliac indicators below the established cut-off level for diagnosis of sacroiliitis, diagnosis of ankylosing spondylitis was excluded, with support for the diagnosis of Forestier's disease.
SPECT/CT slice images in axial, sagittal and coronal planes with low uptake of the radiopharmaceutical in sacroiliac joints. Sacroiliac/promontory values below cut-off level established for diagnosis of sacroiliitis.7,8
The authors declare that this research has not been carried out experiments on humans or animals.
Data confidentialityThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Morales Lozano MI, Ornilla E, Sancho L, Guillén EF. Single-photon emission computed tomography en el diagnóstico de un caso de enfermedad de Forestier. Reumatol Clin. 2019;15:307–308.