To determine the reasons for hospitalisation in patients with systemic lupus erythematosus (SLE) admitted to the Hospital de Clínicas "José de San Martín" Buenos Aires, Argentina.
MethodsWe retrospectively analysed the clinical histories of SLE patients (SLICC 2012) during or prior to hospitalisation, from 1-2014 to 12-2017. Demographic data, reasons for hospitalisation, treatments, SLEDAI-2 K and comorbid conditions.
Results121 hospitalisations corresponding to 72 patients, 25 patients (34.7%) were hospitalised more than once. Females (83.3%), the median length of disease until admission was 5 years. There was more than one reason for hospitalisation in 32, a total of 164 reasons. The main reason was relapse of disease (52.4%). The most frequent manifestations were renal involvement, serositis and pulmonary involvement. Infections were the second reason for hospitalisation (26.8%); urinary tract, pneumonia and soft tissue. Cardiovascular involvement 4.9%. Hospitalisation in a closed unit 14.05%, mortality 2.48%.
ConclusionRelapse of disease and infections were the main reasons for hospitalisation; admission secondary to infection was higher than that reported in other series.
Determinar causas de hospitalización en pacientes con lupus eritematoso sistémico (LES) internados en Hospital de Clínicas “José de San Martín” Buenos Aires, Argentina.
MétodosSe analizaron retrospectivamente historias clínicas de pacientes LES (SLICC 2012) durante o previo a la internación, desde 1-2014 hasta 12-2017. Datos demográficos, motivos de hospitalización, tratamientos, SLEDAI 2 K y condiciones comórbidas.
Resultados121 hospitalizaciones correspondientes a 72 pacientes, 25 pacientes (34,7%) tuvieron más de una hospitalización. Mujeres (83,3%), mediana de duración de la enfermedad hasta la admisión 5 años. Más de una causa de internación en 32, total de 164 motivos. La principal causa fue recaída de la enfermedad (52,4%). La manifestación más frecuente fue compromiso renal, serositis y compromiso pulmonar. Las infecciones fueron la segunda causa de hospitalización (26,8%); tracto urinario, neumonía y partes blandas. Compromiso cardiovascular 4,9%. Hospitalización en unidad cerrada 14,05%, mortalidad 2,48%.
ConclusiónRecaída de la enfermedad e infecciones, fueron las principales causas de hospitalización; la admisión secundaria a infección fue superior a la reportada en otras series.
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease with a wide range of clinical and laboratory manifestations that has exacerbations and remissions.1,2
Hospitalization is common, with an estimated annual rate between 8.6% and 18.9%.1 The main reported reasons for admission are relapse of the disease and acute infection; distinguishing between the two is a real diagnostic and therapeutic challenge. While admissions due to SLE relapse vary between 15% and 80.8%, hospitalizations for infection range between 9.4% and 23.2% according to recent series.1–8
Other reported reasons are cardiovascular disease, deep vein thrombosis (DVT) or pulmonary thromboembolism (PTE), associated autoimmune diseases, pregnancy-related morbidity, complications due to cumulative damage and adverse drug reactions.
Data on inpatients with SLE differ significantly across geographical regions, probably due to ethnic, social, and economic factors, among others.9 Even among populations in Latin America, there are differences in the presentation of the disease.10
The aim of this study was to determine the reasons for the hospitalization of patients with SLE admitted to a university hospital in the city of Buenos Aires, Argentina.
Materials and methodsThe clinical records of patients diagnosed with SLE and admitted to the Hospital de Clínicas "José de San Martín", in the city of Buenos Aires, Argentina, over a four-year period from January 2014 to December 2017, were analysed retrospectively. The criteria for inclusion were patients over 16 years old who met the criteria for SLE (SLICC 2012) during or before hospitalization.11
The SLE Disease Activity Index 2000 (SLEDAI-2 K) was used to measure disease activity, considering a patient to have active disease with a score equal to or greater than four.12
Demographic data, comorbid conditions, reasons for hospitalization, SLEDAI-2 K and treatment on admission were collected. The reasons for hospitalization were not considered mutually exclusive, therefore if a patient had more than one reason, e.g. SLE relapse and infection, both were recorded.
Charlson's index was calculated to assess mortality at one year (score 0, 12%; 1–2, 26%; 3–4, 52% and ≥ 5, 85%).
Epi Info v. 7.2 was used for the statistical analysis. A descriptive analysis was conducted and percentages, means (SD) and medians (IQR) were calculated. Student and Mann-Whitney U tests were used to compare means and medians, respectively, in continuous variables. Dichotomous variables were compared by means of a two-tailed Fisher test, considering a p < .05 statistically significant.
ResultsData from 121 hospitalizations corresponding to 72 patients with SLE were reviewed. Nine patients (9/72 patients, 12.5%) were admitted for organic involvement that led to the diagnosis of SLE during hospitalization. Twenty-five of the 72 patients (34.7%) had more than one hospitalization.
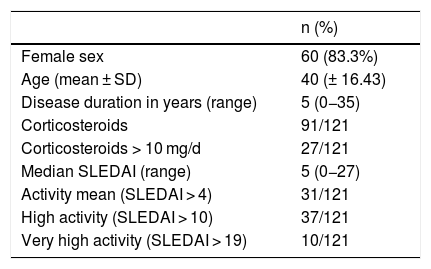
Table 1 shows the demographics, medication, and disease activity. The majority were females (60; 83.3%), with a female: male ratio of 5:1. The median age at diagnosis was 26 years (IQR 19–38) and the mean age at admission was 40 years (SD 16.43). The duration of disease between SLE diagnosis and admission was a median of five years (IQR 1–11; range 0−35 years).
Demographic data and activity measured by SLEDAI of the patients admitted.
| n (%) | |
|---|---|
| Female sex | 60 (83.3%) |
| Age (mean ± SD) | 40 (± 16.43) |
| Disease duration in years (range) | 5 (0−35) |
| Corticosteroids | 91/121 |
| Corticosteroids > 10 mg/d | 27/121 |
| Median SLEDAI (range) | 5 (0−27) |
| Activity mean (SLEDAI > 4) | 31/121 |
| High activity (SLEDAI > 10) | 37/121 |
| Very high activity (SLEDAI > 19) | 10/121 |
The most frequent comorbidities were arterial hypertension (ATH) in 42 patients (34.7%), deep vein thrombosis (DVT) in 21 (17.3%), hypothyroidism in 19 (5.7%) and dyslipidaemia in 16 patients (13.2%). Of the patients with DVT only six (28.6%) had associated antiphospholipid syndrome (APS). In the cases of hypothyroidism, eight (42.1%) were autoimmune. Overlap with other autoimmune diseases was observed in 19% of admissions, mainly APS followed by systemic scleroderma.
Of the total number of patients 10 (8.6%) were smokers, 35 (26%) ex-smokers, 32 (44.4%) had been vaccinated against pneumococcus and 28 (38.8%) against influenza. At the time of admission, the median SLEDAI was five (Range 0−27). A mean Charlson index of 1.42 (SD 0.84) was observed with a range of 1–4.
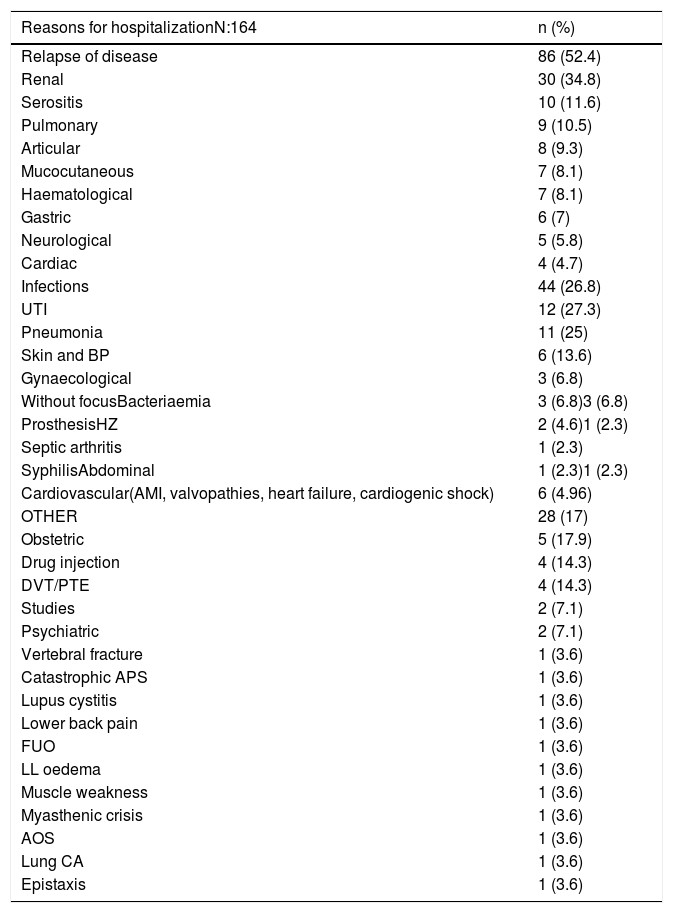
Of the 121 hospitalizations, more than one reason for hospitalization was recorded in 32, making a total of 164 reasons for admission.
Table 2 shows the reasons for hospitalization of patients with SLE. The main reason was relapse of disease 86/164 reasons (52.4%), the most common being renal involvement 30/86 (34.8%), serositis 10/86 (11.6%) and pulmonary involvement 9/86 (10.4%).
Reasons for hospitalization.
| Reasons for hospitalizationN:164 | n (%) |
|---|---|
| Relapse of disease | 86 (52.4) |
| Renal | 30 (34.8) |
| Serositis | 10 (11.6) |
| Pulmonary | 9 (10.5) |
| Articular | 8 (9.3) |
| Mucocutaneous | 7 (8.1) |
| Haematological | 7 (8.1) |
| Gastric | 6 (7) |
| Neurological | 5 (5.8) |
| Cardiac | 4 (4.7) |
| Infections | 44 (26.8) |
| UTI | 12 (27.3) |
| Pneumonia | 11 (25) |
| Skin and BP | 6 (13.6) |
| Gynaecological | 3 (6.8) |
| Without focusBacteriaemia | 3 (6.8)3 (6.8) |
| ProsthesisHZ | 2 (4.6)1 (2.3) |
| Septic arthritis | 1 (2.3) |
| SyphilisAbdominal | 1 (2.3)1 (2.3) |
| Cardiovascular(AMI, valvopathies, heart failure, cardiogenic shock) | 6 (4.96) |
| OTHER | 28 (17) |
| Obstetric | 5 (17.9) |
| Drug injection | 4 (14.3) |
| DVT/PTE | 4 (14.3) |
| Studies | 2 (7.1) |
| Psychiatric | 2 (7.1) |
| Vertebral fracture | 1 (3.6) |
| Catastrophic APS | 1 (3.6) |
| Lupus cystitis | 1 (3.6) |
| Lower back pain | 1 (3.6) |
| FUO | 1 (3.6) |
| LL oedema | 1 (3.6) |
| Muscle weakness | 1 (3.6) |
| Myasthenic crisis | 1 (3.6) |
| AOS | 1 (3.6) |
| Lung CA | 1 (3.6) |
| Epistaxis | 1 (3.6) |
AOS: Ascitic oedematous syndrome; CA: Cancer; DVT/PTE: Deep vein thrombosis/pulmonary thromboembolism; FUO: Fever of unknown origin; HZ: Herpes zoster; LL: Lower limb; UTI: Urinary tract infection.
Infections were the second most common reason for hospitalization, 44/164 (26.8%), the most frequent being urinary tract infections 12/44 (27.3%), pneumonia 11/44 (25%) and soft-tissue infections 6/44 (13.6%). In patients who developed pneumonia, no significant differences were found between patients vaccinated and unvaccinated for pneumococcus and influenza (p < .52 and p < 1, respectively).
Hospitalization for cardiovascular reasons was observed in 6/164 (4.96%).
Other reasons were found in 28/164 (17%), such as obstetric in 5/28 (17.9%), drug injection in 4/28 (14.3%), DVT/PET in 4/28 (14.3%), psychiatric in 2/28 (7.1%), vertebral fracture in 1/28 (3.6%), among others. Of the hospital admissions for DVT/PTE, three had associated PAS.
In the hospitalizations due to relapse of the disease the mean age was 35 (SD 13.9) years versus 44.12 (SD 17.9) in the rest (p < .0017) and the median disease duration was 3.5 (IQR 1-7) versus 7 years (IQR 1-14; p < .0017), respectively.
The SLEDAI-2 K score for relapse revealed a median of 10.4 (IQR 4–16) while the remaining causes were 0 (IQR 0–5) (p < .01).
In the hospitalizations due to relapse, the length of hospitalization was 16.52 days (SD 15) vs. 11.75 (SD 8.9) days for the remaining reasons (p < .03).
Seventeen out of 121 hospitalizations (14.05%) required a closed unit (coronary unit or intensive care). In these cases, the median length of hospitalization was 24 days (IQR 14–30) compared to 10 days (IQR 5–15.5) in the main ward (p < 0.008). There were no statistically significant differences in age, disease duration, causes of hospitalization, Charlson index, or SLEDAI among those who required a closed unit compared to those who did not.
Three patients (2.48%) died. Causes of death were sepsis without focus, obstetric complications, and cardiogenic shock. No significant differences in Charlson index values were observed between the patients who died compared to those who survived.
DiscussionIn this study we describe the reasons for hospitalization of SLE patients admitted to our hospital over a period of four years (2014–2017).
The main cause of hospitalization was relapse of the disease (52.4%), coinciding with that reported in the specialised literature.1,2,4,5,7,8 The admission rate for this reason varies widely, from 15% in the Danish cohort3 to 80.8% in the Malaysian cohort, 8 which could be due not only to ethnic and socioeconomic differences, but also to the medical criteria used for hospitalization. As in other series, patients admitted due to relapse were younger, had a higher SLEDAI-2 K score and shorter duration of SLE,1,4,6,7 which supports the data that suggest greater aggressiveness during the first five years of the disease.13
The second most frequent reason was infection (26.8%). The hospitalization rate for this reason was higher than previously reported (9.4%-23.2%).1–8 Compared with data from Latin America, the percentage was similar to the Honduran cohort (26.3%),14 although significantly lower than that of Peru (42.6%).15 This discrepancy could be partly attributed to the design of our study, where all reasons for hospitalization were recorded and not just the main reason as in other studies, which may have underestimated the actual percentage of admissions due to infections. On the other hand, patients with SLE are clearly vulnerable to infection both because of the nature of the disease and because of the immunosuppressive treatment prescribed for the management of clinical manifestations. In turn, infection may influence the activity of SLE,16 hence the importance of an adequate balance between disease control and infection prevention.
The most frequent infections were of the urinary tract (27.3%), followed by pneumonia (25%) and soft tissue infections (13.6%). Previous studies, however, identified pneumonia as the main infectious reason for hospitalization.1,2,4,7,14,15,17,18 Although in our study a high percentage of patients had been vaccinated against pneumococcus and influenza, no significant differences were observed between vaccinated and unvaccinated patients with respect to the development of pneumonia.
Cardiovascular involvement was responsible for 4.9% of hospitalizations. Although patients with SLE have an increased risk of coronary disease compared to the general population, resulting in high morbidity and mortality, this was an infrequent reason for hospitalization in our series, coinciding with previous studies.1,2,4,5 This could be due to the shorter disease duration at time of admission and the shorter cumulative time of corticosteroid use.
Thrombotic events were only observed in five cases (four DVT/PTE and one catastrophic APS), similar to that reported in other studies.3–5,7 It should be noted that most patients had a history of APS, being in an inadequate range of anticoagulation at the time of admission.
The percentage of patients with SLE requiring hospitalization in a closed unit (coronary unit or intensive care) was 14.05%, similar to that reported in Canadian series that ranged from 13% to 14.3%.1,6 However, this result was higher than that described in other studies, which present an average of 3.9% to 4.8%,7,8 which could be attributed to a more severe clinical picture in our patients at the time of admission or during hospitalization, observing significant differences in the median length of hospitalization among those requiring closed unit with respect to patients admitted to the main ward (24 vs 10 days).
A total of 34.7% patients required re-hospitalization during the study period. Previous reports showed variable results, from 28.7% to 54.7%.4–8 A recent study showed that 34% of patients with SLE required readmission within 30 days of initial hospitalization, observing a significant association with the presence of chronic damage, anaemia and hypoalbuminaemia.19 Moreover, an association with specific clinical manifestations such as nephritis, serositis, neurological involvement and thrombocytopenia was found, while age had a significant inverse relationship with the risk of early readmission, demonstrating once again the increased severity of SLE in young patients.20
Mortality in hospitalized SLE patients varies from 2.17% to 10.4% depending on the series.1,2,4,6–8,14,15,17 The main reasons reported are infection and relapse of the disease,2,4,7,8,17 relapse with concomitant infection and high rate of damage on admission being independent predictors of mortality.15 In our study, mortality was 2.48%, the causes being sepsis without focus, obstetric complication and cardiogenic shock.
Our work has some limitations: its retrospective nature, the number of patients included and a single hospital centre, which could cause bias in interpretation. On the other hand, it is the first paper that describes reasons for hospitalization in lupus patients in Argentina, contributing towards defining the characteristics of patients in our country and Latin America.
In conclusion, patients with SLE are frequently admitted to our hospital, the main reasons for hospitalization being relapse of the disease and infections. This confirms that reported in the specialist literature. However, as in other Latin American countries such as Honduras and Peru, the percentage of admissions due to infection was higher than that observed in other series, which could be attributed to a greater susceptibility of our patients to infections, either due to the treatment used to control SLE, their own demographic characteristics or due to the functioning of the health system and access to it.
FundingThis research has not received specific support from public sector agencies, the commercial sector, or non-profit organisations.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Perrotta N, López Meiller MJ, Malah V, Dubinsky D. Causas de internación en pacientes con lupus eritematoso sistémico en un hospital universitario de Buenos Aires. Reumatol Clin. 2021;17:471–474.