During the Covid-19 pandemic strategies to prevent transmission of the viral infection obliged our hospital to promote virtual consultations.
ObjetiveThe objective of this study is to describe the results obtained with the previous strategy of transferring activity to teleconsultation during the period of maximum impact of the pandemic.
Material and methodsBetween 16/03 and 10/05/2020 all successive consultations in our unit were performed in virtual rheumatology teleconference (RTC) format. The socio-demographic, geo-functional and clinical characteristics of all patients were collected; a numeric verbal scale (NVS) (where 0 = very dissatisfied to 10 = fully satisfied) was applied to assess the degree of satisfaction of the doctor/patient with the RTC.
Results469 TC were included. Most patients seen by RTC were women, mean age: 60,83 years. Only 16% had university education. The mean distance travelled for face-to face consultation is 33 Km with a mean total time of 2 h. Most individuals were diagnosed with osteoarthritis/soft tissue rheumatic diseases and/or osteoporosis; 21% had rheumatoid arthritis. The mean length of the TC was 9.64 min. We find more patient satisfaction with the TC when their level of education is higher (OR = 4.12); doctor satisfaction was higher when the individual was better able to manage the Internet (OR = 3.01).
ConclusionIt is possible to transfer rheumatological care activity to TC with a considerable degree of satisfaction for both the patient and the doctor.
Durante la pandemia por Covid 19 las necesidades de prevención de transmisión de la infección viral nos obligaron a potenciar las consultas virtuales.
ObjetivoEl objetivo de estudio es describir los resultados obtenidos con la anterior estrategia y definir el perfil de paciente más idóneo para aplicarla.
Material y métodosDurante el período comprendido entre el 16/3 y el 10/05/2020 todas las consultas sucesivas de nuestro servicio fueron realizadas en formato de teleconsulta reumatológica (TCR). Se recogieron las características sociodemográficas, geofuncionales y clínicas de los pacientes; se evalúo mediante escala numérica verbal (ENV) (0–10, donde 0 = muy insatisfecho hasta 10 = completamente satisfecho) el grado de satisfacción del paciente/médico con la TC.
ResultadosLa mayoría de los pacientes atendidos en las 469 TCR realizadas fueron mujeres, con una edad media de 60,83 años. Sólo el 16% habían realizado estudios universitarios. La distancia media recorrida para acudir a una consulta presencial era de 33 km, con una inversión de tiempo total promedio de 2 horas. La mayoría de los sujetos estaban diagnosticados de artrosis/reumatismos de partes blandas y/o osteoporosis; el 21% eran portadores de artritis reumatoide. La duración media de la TCR fue de 9,64 min. Encontramos una mayor satisfacción con la TCR por parte del paciente, cuando el nivel de estudios era más alto (OR = 4,33), y por parte del médico cuando el individuo manejaba mejor internet (OR = 3,22).
ConclusiónEs posible transferir actividad asistencial reumatológica hacia la TCR con un grado importante de satisfacción para el paciente y el médico.
Rheumatic diseases (33.6%) together with lower back pain (23.9%) are amongst the most common causes of consultation.1 However, access to medical care is not always easy for this type of patient. Physical disability in many of them, distance and difficulty in obtaining face-to-face access to specialists (especially for those living in rural areas), may delay diagnosis and treatment, causing irreversible joint damage.2,3
Teleconsultation (TC) is understood as the use of communication technologies to provide health services to the general population.4 Nowadays, the development of TC should allow for a reduction in the number of face-to-face consultations (without undermining the quality of care) to the benefit of the rheumatic patient, who often complains of difficulty in travelling.5–7 Synchronised TC methods mean that communication in real time may be effectively made between places which are spatially distant, without the need for the physical presence of the patient. These include telephone consultation and video conferencing systems. During the last 10 years, thanks to technological improvements and the increase in the speed of data transmission, a notable increase of TC has occurred, including tele-rheumatology (TR).8,9 However, very few studies have been published on the usefulness and effectiveness of the latter.10
During the initial wave of the COVID-19 pandemic, care needs and epidemiological strategies for prevention of viral infection transmission forced us to increase virtual consultations as part of successive consultations in our service. The aim of this study is to describe the results obtained from the previously described strategy of transferring face-to-face activity with rheumatology teleconsultation (RTC) during the period of maximum epidemic impact.
Material and methodsThe hypothesis of our study was that, faced with the situation of a health crisis triggered by the pandemic, and in order to maintain the attention and care of the patients, it was possible to establish an RTC procedure to guarantee care quality, identifying an especially appropriate patient profile to apply this medical care system to.
During the period between 16th March and 10th May 2020 (total period of lockdown and phase 0 of de-escalation of the state of emergency due to the COVID-19 pandemic in Spain), all successive consultations from our service were transferred to the teleconsultation format. Videoconsultations were not made. The population served was 257,762 inhabitants, 50.5% men and 49.5% women; 16% of them were over 65 years of age (INE 2019).
An observational, descriptive, longitudinal, retrospective study was conducted, covering the RTCs made during the before-mentioned period. The study protocol was approved by the CEIM of our health area (Ref. CEIm: 2020.25.PR). Eligible patients had to meet with the following inclusion criteria: a) individuals who had an appointment for consultation in the rheumatology department during the study period and b) patients attended during this period in RTC format. The following exclusion criteria were established: a) individuals who the doctor considered were not apt for the RTC procedure, due to the absence of necessary care information; b) subjects who could not be located and c) individuals with inadequate mental skills to reliably cope with RTC.
The sociodemographic characteristics of all patients were recorded, including their educational level and the level of skill they had in managing information and communication technologies. Within the geo-functional parameters we collected information on the following aspects: a) place and environment of residence (urban/rural); b) type of transport used to attend consultation (private/public); c) distance covered (km) and average time invested (h) to attend a regular face-to-face visit; d) presence or non presence of disability, and e) need or non need for a caregiver to accompany them for consultation.
All the RTC included were for successive visits. The care information obtained included: a) type of consultation: delivery of results after 1st face-to-face visit verified prior to the initiation of the study or the check-up visit (clinical/analytical/other complementary control/therapeutic sequence adjustment); b) follow-up time of the patient in rheumatology consultation (years); c) number of check-ups per year; d) time (months) passed from most recent consultation; e) time (min) of duration of the RTC. The clinical characteristics of each subject were also collected: a) main rheumatological diagnosis; b) other rheumatological diagnoses; c) tests requested in the RTC; d) therapeutic information: normal rheumatological treatments, changes to treatment (type of route, dose or change of drug), control of biological therapy and d) outstanding comorbidities: diabetes mellitus, arterial hypertension, dyslipidaemia, peptic ulcer, depression, anxiety, i stroke, ischaemic cardiopathy.
The level of patient/doctor satisfaction with RTC was evaluated using the verbal numerical scale (between 0–10, where 0 = highly dissatisfied up to 10 = fully satisfied). We also asked the patient about the usefulness of RTC compared with the regular consultation and the patient and doctor on whether they would repeat this format of non face-to-face medical attention.
Within the statistical analysis, a bivariate analysis of mean comparison was performed, with the Student’s t-test to contrast the measurement of the doctor and patient scores for the different variables. A comparison study of frequencies was also made using contingency tables with the Chi-squared test, to analyse the association of sociodemographic, geo-functional and clinical variables with the use of RTC and the repetition of this, according to doctor and patient opinions. This same focus was repeated with the scores of the doctor and patient dichotomizing these variables. Finally, the effect size measurement was calculated in the doctor and patient scores, evaluating the odds ratio (OR) using logistic regression multivariate analysis. The analyses were performed with the STATA 13.1 (College Station, TX, U.S.A.) programme.
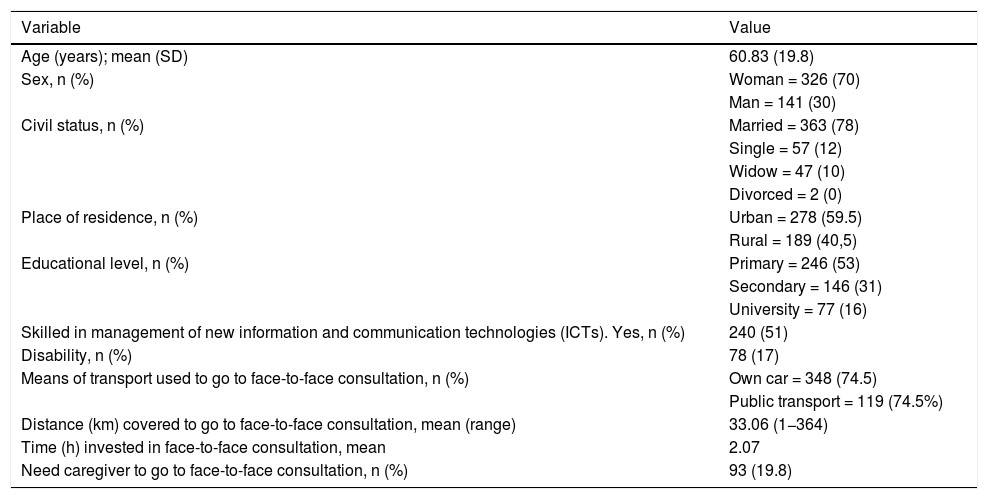
ResultsData was obtained from 469 RTC made in 28 sessions. Tables 1 and 2 show the main descriptive results obtained in this study. As may be observed, most patients are women, with a mean age of approximately 61 years and a low educational level (only 16% had a university level of education). 51% of the subjects felt comfortable managing the Internet. 59% resided in an urban area. The mean distance they travelled to a face-to-face consultation was 33 km, with a total average time investment of 2 h. Most of the patients (74.2%) usually go to the hospital in their own vehicle.
Sociodemograpic and geo-functional characteristics.
| Variable | Value |
|---|---|
| Age (years); mean (SD) | 60.83 (19.8) |
| Sex, n (%) | Woman = 326 (70) |
| Man = 141 (30) | |
| Civil status, n (%) | Married = 363 (78) |
| Single = 57 (12) | |
| Widow = 47 (10) | |
| Divorced = 2 (0) | |
| Place of residence, n (%) | Urban = 278 (59.5) |
| Rural = 189 (40,5) | |
| Educational level, n (%) | Primary = 246 (53) |
| Secondary = 146 (31) | |
| University = 77 (16) | |
| Skilled in management of new information and communication technologies (ICTs). Yes, n (%) | 240 (51) |
| Disability, n (%) | 78 (17) |
| Means of transport used to go to face-to-face consultation, n (%) | Own car = 348 (74.5) |
| Public transport = 119 (74.5%) | |
| Distance (km) covered to go to face-to-face consultation, mean (range) | 33.06 (1−364) |
| Time (h) invested in face-to-face consultation, mean | 2.07 |
| Need caregiver to go to face-to-face consultation, n (%) | 93 (19.8) |
Care and clinical characteristics.
| Variable | Value |
|---|---|
| Type of consultation, n (%) | Results of 1st visit = 49 (11) |
| Successive consultations = 418 (89) | |
| Type of review, na | Clinical assessment = 354 |
| Delivery of results = 338 | |
| Adjustment to treatment = 38 | |
| Years of follow-up in rheumatology, mean (SD) | 8.03 (2.5) |
| Number of visits per year, mean (SD) | 2 (3.5) |
| Time (months ) from last review, media (SD) | 6.19 (3.5) |
| Rheumatic disease attended, nb | OA/STR = 199 |
| OP = 141 | |
| RA = 99 | |
| PsA = 37 | |
| AS = 56 | |
| FM = 37 | |
| Gout = 20 | |
| SLE = 17 | |
| Col = 27 | |
| RPM = 15 | |
| ACPD = 5 | |
| Biologic therapy control, n (%) | 98 (21) |
| No changes in treatment in RTC, n (%) | 379 (81) |
| Duration of the RTC (minutes), mean (range) | 9.64 (3−30) |
| Satisfaction with RTC NVS patient: mean (SD) | 8.62 (4) |
| Satisfaction with RTC NVS doctor: mean (SD) | 8.84 (.5) |
| Would they repeat RTC? Patient, yes, n (%) | 391 (84) |
| Would they repeat RTC? Doctor, yes, n (%) | 431 (92) |
ACPD: Arthropathy from calcium pyrophosphate deposit; AS: Ankylosing Spondylitis, Col: Other colagenosis not SLE; FM: Fibromyalgia; OA/STR: Osteoarthritis/Soft tissue rheumatism; OP: Osteoporosis; PMR: Rheumatic Polymyalgia; PsA: Psoriatic Arthritis; RA: Rheumatoid Arthritis; RTC: Rheumatology Teleconference; SLE: Systemic Lupus Erythematosus.
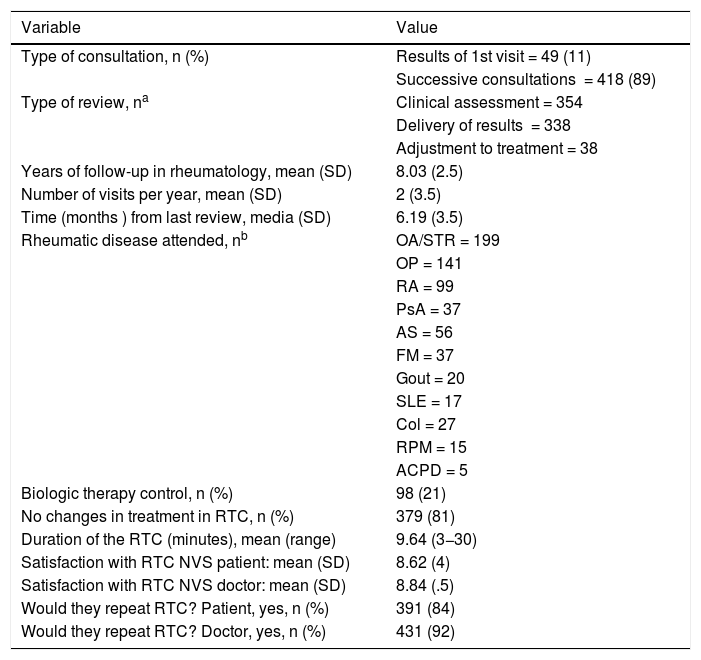
89% of the RTC were successive visits for clinical control or evaluation of analytical results. Mean time of follow-up of the subjects for whom the RTC was practised was 8 years, with a mean of 2 annual check-up consultations. Most of the individuals were diagnosed with osteoarthritis/soft tissue rheumatism or osteoporosis. 21% of the patients presented with rheumatoid arthritis. Revision of biological therapies previously indicated to the patient was performed in 21% of the RTC. In 81% of cases, there were modifications to the treatment of rheumatic patients. The mean duration of RTC was 9.64 min.
The mean levels of satisfaction with the RTC procedure were very high, both for the patient (8.62) and the doctor (8.84). Over 80% of patients attended would repeat the RTC and 79.3% considered them useful. The need for a face-to-face consultation after teleconsultation was not analysed.
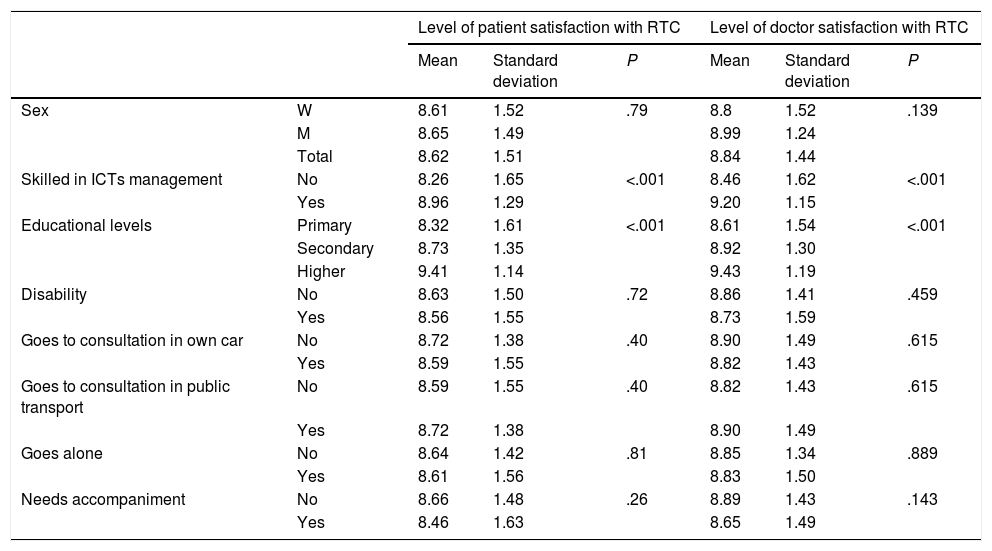
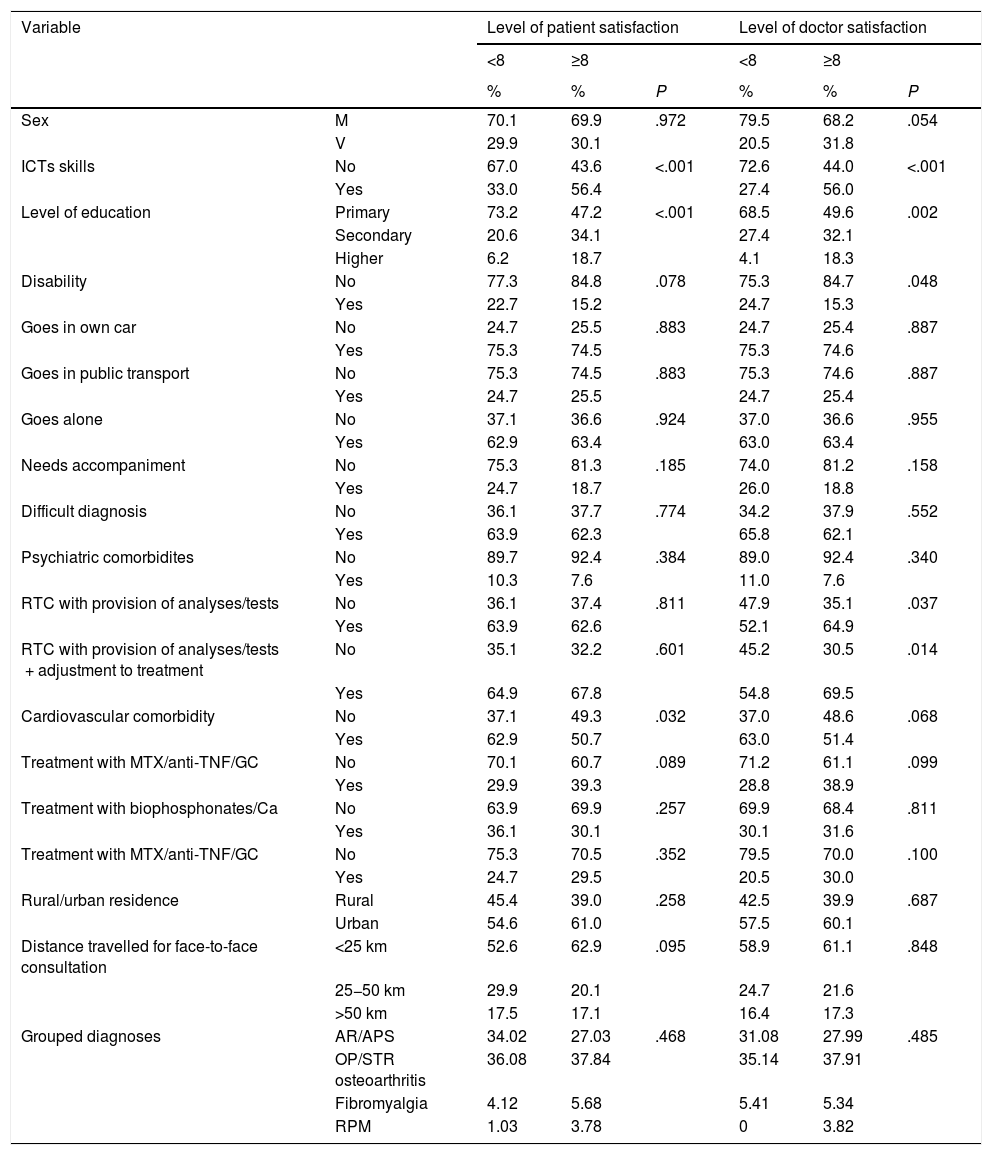
The association between the degree of patient and doctor satisfaction with different sociodemographic and geo-functional variables (Table 3) was analysed. No differences in conformity with the RTC were appreciated (in either patient or doctor estimation) according to sex, the existence of disability, the type of transport regularly used for the subject to go to hospital (private transport versus public transport) and the need or non need for a companion. However, we did detect greater satisfaction with RTC, both by the patient and the doctor, when the level of education was higher and the individual referred to better Internet management (P < .001).
Relationship between sociodemographic variables and level of patient and doctor satisfaction with the rheumatology teleconsultation.
| Level of patient satisfaction with RTC | Level of doctor satisfaction with RTC | ||||||
|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | P | Mean | Standard deviation | P | ||
| Sex | W | 8.61 | 1.52 | .79 | 8.8 | 1.52 | .139 |
| M | 8.65 | 1.49 | 8.99 | 1.24 | |||
| Total | 8.62 | 1.51 | 8.84 | 1.44 | |||
| Skilled in ICTs management | No | 8.26 | 1.65 | <.001 | 8.46 | 1.62 | <.001 |
| Yes | 8.96 | 1.29 | 9.20 | 1.15 | |||
| Educational levels | Primary | 8.32 | 1.61 | <.001 | 8.61 | 1.54 | <.001 |
| Secondary | 8.73 | 1.35 | 8.92 | 1.30 | |||
| Higher | 9.41 | 1.14 | 9.43 | 1.19 | |||
| Disability | No | 8.63 | 1.50 | .72 | 8.86 | 1.41 | .459 |
| Yes | 8.56 | 1.55 | 8.73 | 1.59 | |||
| Goes to consultation in own car | No | 8.72 | 1.38 | .40 | 8.90 | 1.49 | .615 |
| Yes | 8.59 | 1.55 | 8.82 | 1.43 | |||
| Goes to consultation in public transport | No | 8.59 | 1.55 | .40 | 8.82 | 1.43 | .615 |
| Yes | 8.72 | 1.38 | 8.90 | 1.49 | |||
| Goes alone | No | 8.64 | 1.42 | .81 | 8.85 | 1.34 | .889 |
| Yes | 8.61 | 1.56 | 8.83 | 1.50 | |||
| Needs accompaniment | No | 8.66 | 1.48 | .26 | 8.89 | 1.43 | .143 |
| Yes | 8.46 | 1.63 | 8.65 | 1.49 | |||
ICTs: Information and Communication Technologies; M: Men; RTC: Rheumatology Teleconsultation; W: Women.
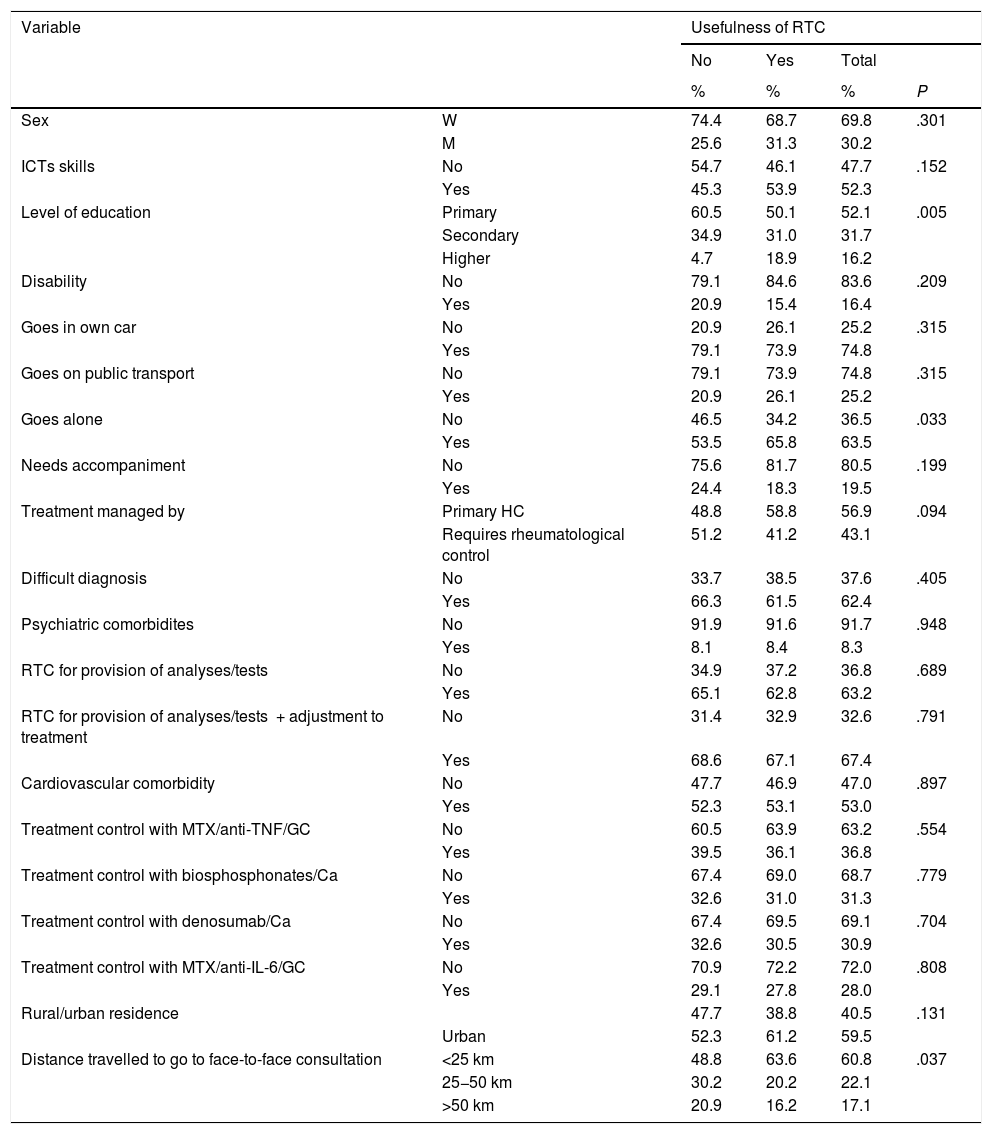
From the patient’s viewpoint, if we relate the use of non use of the RTC with sociodemographic variables we do not find any association with the patient’s sex, the ability in management of new information and communication technologies (ITCs), the existence or not of disability, type of transport used to attend face-to-face consultations or the need for a companion to go to the hospital. However, an association with the patient’s educational level was detected: subjects with a lower educational level found RTC less useful than those with medium or higher educational levels (P = .005). The subjects who had to go to face-to-face consultations with companions found RTC more useful than those who did not need accompanying (P = .033).When the doctor was asked about the ideal way of repeating RTC and they tried to relate it to sociodemographic and geo-functional variables of the patient they did not detect statistically significant associations with sex, type of transport to visit the hospital and the need or non need for accompaniment to attend their regular face-to-face consultation. We did detect that the rheumatologist believed repetition of RTC was less ideal if the patient lacked ICT skills (P = .013) and all the more so if the patient had a disability (P = .05).
Table 4 shows the relationship between the degree of patient/doctor satisfaction and the clinical variables. No association was found between the level of satisfaction of both with the complexity of the treatment, the difficulty in diagnosis, the existence of psychiatric comorbidity (depression/anxiety), treatments with calcium, anti-osseous reabsorption agents, glucocorticoids, methotrexate, anti-TNF or anti-IL-6. Only for the doctors was a statistically significant association detected between satisfaction with RTC and cardiovascular comorbidity and the type of successive visit. Specifically, the rheumatologist was less satisfied when the patient who they were applying RTC to presented with cardiovascular comorbidity (P = .005). In contrast, the satisfaction of the doctor was higher when the RTC involved provision of analytical outcomes or complementary tests (P = .009) or the former plus an adjustment to treatment (P = .001). This association was not detected when the RTC involved delivery of results from bone mineral density tests.
Usefulness of rheumatology teleconsultation for the patient: relationship with sociodemographic and clinical variables.
| Variable | Usefulness of RTC | ||||
|---|---|---|---|---|---|
| No | Yes | Total | |||
| % | % | % | P | ||
| Sex | W | 74.4 | 68.7 | 69.8 | .301 |
| M | 25.6 | 31.3 | 30.2 | ||
| ICTs skills | No | 54.7 | 46.1 | 47.7 | .152 |
| Yes | 45.3 | 53.9 | 52.3 | ||
| Level of education | Primary | 60.5 | 50.1 | 52.1 | .005 |
| Secondary | 34.9 | 31.0 | 31.7 | ||
| Higher | 4.7 | 18.9 | 16.2 | ||
| Disability | No | 79.1 | 84.6 | 83.6 | .209 |
| Yes | 20.9 | 15.4 | 16.4 | ||
| Goes in own car | No | 20.9 | 26.1 | 25.2 | .315 |
| Yes | 79.1 | 73.9 | 74.8 | ||
| Goes on public transport | No | 79.1 | 73.9 | 74.8 | .315 |
| Yes | 20.9 | 26.1 | 25.2 | ||
| Goes alone | No | 46.5 | 34.2 | 36.5 | .033 |
| Yes | 53.5 | 65.8 | 63.5 | ||
| Needs accompaniment | No | 75.6 | 81.7 | 80.5 | .199 |
| Yes | 24.4 | 18.3 | 19.5 | ||
| Treatment managed by | Primary HC | 48.8 | 58.8 | 56.9 | .094 |
| Requires rheumatological control | 51.2 | 41.2 | 43.1 | ||
| Difficult diagnosis | No | 33.7 | 38.5 | 37.6 | .405 |
| Yes | 66.3 | 61.5 | 62.4 | ||
| Psychiatric comorbidites | No | 91.9 | 91.6 | 91.7 | .948 |
| Yes | 8.1 | 8.4 | 8.3 | ||
| RTC for provision of analyses/tests | No | 34.9 | 37.2 | 36.8 | .689 |
| Yes | 65.1 | 62.8 | 63.2 | ||
| RTC for provision of analyses/tests + adjustment to treatment | No | 31.4 | 32.9 | 32.6 | .791 |
| Yes | 68.6 | 67.1 | 67.4 | ||
| Cardiovascular comorbidity | No | 47.7 | 46.9 | 47.0 | .897 |
| Yes | 52.3 | 53.1 | 53.0 | ||
| Treatment control with MTX/anti-TNF/GC | No | 60.5 | 63.9 | 63.2 | .554 |
| Yes | 39.5 | 36.1 | 36.8 | ||
| Treatment control with biosphosphonates/Ca | No | 67.4 | 69.0 | 68.7 | .779 |
| Yes | 32.6 | 31.0 | 31.3 | ||
| Treatment control with denosumab/Ca | No | 67.4 | 69.5 | 69.1 | .704 |
| Yes | 32.6 | 30.5 | 30.9 | ||
| Treatment control with MTX/anti-IL-6/GC | No | 70.9 | 72.2 | 72.0 | .808 |
| Yes | 29.1 | 27.8 | 28.0 | ||
| Rural/urban residence | 47.7 | 38.8 | 40.5 | .131 | |
| Urban | 52.3 | 61.2 | 59.5 | ||
| Distance travelled to go to face-to-face consultation | <25 km | 48.8 | 63.6 | 60.8 | .037 |
| 25−50 km | 30.2 | 20.2 | 22.1 | ||
| >50 km | 20.9 | 16.2 | 17.1 | ||
GC: Glucocorticoids; ICTs: Information and Communication Technologies; IL-6: Interleukin 6; M: Men; MTX: Methotrexate; RTC: Rheumatology Teleconsultation; TNF: Tumour Necrosis Factor; W: Women.
Due to the high scores in RTC evaluation the cut-off point was a score under or equal to 8, against one higher than this value. If we establish the threshold as highly favourable satisfaction to the intervention with RTC where the patient has a NVS equal to or higher than 8 (Table 5) we appreciate (both in the patient and doctor score) a statistically significant association of this level with a higher ability and training in ICTs (P < .001) and a higher level of education (P < .001). The degree of patient/doctor satisfaction with the RTC is not influenced by the rheumatic disease presented by the patient.
Relationship between level of satisfaction (patient and doctor) very favourable (≥8) or not (<8) and demographic and clinical variables.
| Variable | Level of patient satisfaction | Level of doctor satisfaction | |||||
|---|---|---|---|---|---|---|---|
| <8 | ≥8 | <8 | ≥8 | ||||
| % | % | P | % | % | P | ||
| Sex | M | 70.1 | 69.9 | .972 | 79.5 | 68.2 | .054 |
| V | 29.9 | 30.1 | 20.5 | 31.8 | |||
| ICTs skills | No | 67.0 | 43.6 | <.001 | 72.6 | 44.0 | <.001 |
| Yes | 33.0 | 56.4 | 27.4 | 56.0 | |||
| Level of education | Primary | 73.2 | 47.2 | <.001 | 68.5 | 49.6 | .002 |
| Secondary | 20.6 | 34.1 | 27.4 | 32.1 | |||
| Higher | 6.2 | 18.7 | 4.1 | 18.3 | |||
| Disability | No | 77.3 | 84.8 | .078 | 75.3 | 84.7 | .048 |
| Yes | 22.7 | 15.2 | 24.7 | 15.3 | |||
| Goes in own car | No | 24.7 | 25.5 | .883 | 24.7 | 25.4 | .887 |
| Yes | 75.3 | 74.5 | 75.3 | 74.6 | |||
| Goes in public transport | No | 75.3 | 74.5 | .883 | 75.3 | 74.6 | .887 |
| Yes | 24.7 | 25.5 | 24.7 | 25.4 | |||
| Goes alone | No | 37.1 | 36.6 | .924 | 37.0 | 36.6 | .955 |
| Yes | 62.9 | 63.4 | 63.0 | 63.4 | |||
| Needs accompaniment | No | 75.3 | 81.3 | .185 | 74.0 | 81.2 | .158 |
| Yes | 24.7 | 18.7 | 26.0 | 18.8 | |||
| Difficult diagnosis | No | 36.1 | 37.7 | .774 | 34.2 | 37.9 | .552 |
| Yes | 63.9 | 62.3 | 65.8 | 62.1 | |||
| Psychiatric comorbidites | No | 89.7 | 92.4 | .384 | 89.0 | 92.4 | .340 |
| Yes | 10.3 | 7.6 | 11.0 | 7.6 | |||
| RTC with provision of analyses/tests | No | 36.1 | 37.4 | .811 | 47.9 | 35.1 | .037 |
| Yes | 63.9 | 62.6 | 52.1 | 64.9 | |||
| RTC with provision of analyses/tests + adjustment to treatment | No | 35.1 | 32.2 | .601 | 45.2 | 30.5 | .014 |
| Yes | 64.9 | 67.8 | 54.8 | 69.5 | |||
| Cardiovascular comorbidity | No | 37.1 | 49.3 | .032 | 37.0 | 48.6 | .068 |
| Yes | 62.9 | 50.7 | 63.0 | 51.4 | |||
| Treatment with MTX/anti-TNF/GC | No | 70.1 | 60.7 | .089 | 71.2 | 61.1 | .099 |
| Yes | 29.9 | 39.3 | 28.8 | 38.9 | |||
| Treatment with biophosphonates/Ca | No | 63.9 | 69.9 | .257 | 69.9 | 68.4 | .811 |
| Yes | 36.1 | 30.1 | 30.1 | 31.6 | |||
| Treatment with MTX/anti-TNF/GC | No | 75.3 | 70.5 | .352 | 79.5 | 70.0 | .100 |
| Yes | 24.7 | 29.5 | 20.5 | 30.0 | |||
| Rural/urban residence | Rural | 45.4 | 39.0 | .258 | 42.5 | 39.9 | .687 |
| Urban | 54.6 | 61.0 | 57.5 | 60.1 | |||
| Distance travelled for face-to-face consultation | <25 km | 52.6 | 62.9 | .095 | 58.9 | 61.1 | .848 |
| 25−50 km | 29.9 | 20.1 | 24.7 | 21.6 | |||
| >50 km | 17.5 | 17.1 | 16.4 | 17.3 | |||
| Grouped diagnoses | AR/APS | 34.02 | 27.03 | .468 | 31.08 | 27.99 | .485 |
| OP/STR osteoarthritis | 36.08 | 37.84 | 35.14 | 37.91 | |||
| Fibromyalgia | 4.12 | 5.68 | 5.41 | 5.34 | |||
| RPM | 1.03 | 3.78 | 0 | 3.82 | |||
Ca: Calcium; GC: Glucocorticoids; ICTs: Information and Communication Technologies; M: Men; MTX: Methotrexate; OP: Osteoporosis; PsA: Psoriatic Arthritis; RA: Rheumatoid Arthritis; RPM: Rheumatic Polymyalgia; RTC: Rheumatology Teleconference; STR: Soft Tissue Rheumatism; TNF: Tumour Necrosis Factor W: Women;
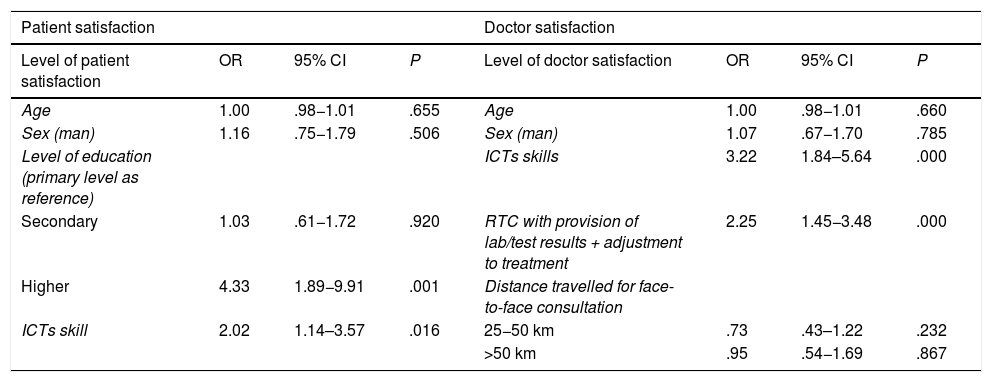
Finally, the most ideal patient profile to apply RTC to, according to the patient estimation (Table 6), after logistic regression, was that of a person with a higher education level (OR = 4.33) and skills in ICTs management (OR = 2,02). Rheumatologist were also more satisfied when the RTC included laboratory control or another diagnostic test or therapeutic adjustment (OR = 2.25) and also with the patient’s skill in ICTs management (OR = 3.22). Curiously, the distance covered to the face-to-face consultation had no impact on this model.
Logistic regression multivariate analysis. Measurement of effect in doctor and patient evaluation: main parameters which conditioned a profile of high satisfaction (equal to or above 8 in VNE 0-100).
| Patient satisfaction | Doctor satisfaction | ||||||
|---|---|---|---|---|---|---|---|
| Level of patient satisfaction | OR | 95% CI | P | Level of doctor satisfaction | OR | 95% CI | P |
| Age | 1.00 | .98−1.01 | .655 | Age | 1.00 | .98−1.01 | .660 |
| Sex (man) | 1.16 | .75−1.79 | .506 | Sex (man) | 1.07 | .67−1.70 | .785 |
| Level of education (primary level as reference) | ICTs skills | 3.22 | 1.84–5.64 | .000 | |||
| Secondary | 1.03 | .61−1.72 | .920 | RTC with provision of lab/test results + adjustment to treatment | 2.25 | 1.45−3.48 | .000 |
| Higher | 4.33 | 1.89−9.91 | .001 | Distance travelled for face-to-face consultation | |||
| ICTs skill | 2.02 | 1.14–3.57 | .016 | 25−50 km | .73 | .43–1.22 | .232 |
| >50 km | .95 | .54−1.69 | .867 | ||||
CI: Confidence Interval; ICTs: Information and Communication Technologies; OR: Odds Ratio; RTC: Rheumatology Teleconsultation; VNS: Verbal Numerical Scale.
The coronavirus pandemic and the strategies for preventing it spreading have forced us to make rapid changes to the standard healthcare model.11 One of the most relevant changes was the great advance in the establishment of TC. The emergence of TR and RTC is allowing us to develop innovative channels of communication between specialists and their patients, in circumstance like the present, where the physical presence of patients in health centres is not adviseable.12
Although there is broad and widespread favourable opinion towards TR,13,14 the body of scientific evidence which supports it is limited.15 McDougall et al.8 carried out a systematic review of published evidence (between 1946 and 2015) on TR in the diagnosis and treatment of autoimmune inflammatory rheumatic diseases, mainly rheumatoid arthritis. They confirmed that clinical trials are scarce and cost-effectiveness studies performed to assess the same. Also, the effectiveness of TC in rheumatology may vary depending on the disease, the phase of its evolution and the method of TC used. As a result there is interest in studies like ours, where we cover a broad patient sample, with a vast range of diseases, evolution times, years, therapies and healthcare follow-up.
It has been demonstrated that control of diseases such as RA is conditioned by distance between the patient’s place of residence and their health centre of reference, particularly in rural areas in the U.S.A., and within the MediCare system.16–18 The Veteran Department, in that country has regularly used TC strategies to care for ill patients who reside in rural areas and have difficulty attending face-to-face sessions in health centres. Wood et al.,10 prospectively analysed in this collective the usefulness of RTC in the activity metrics of inflammatory arthropathies, the level of patient satisfaction and the cost-saving involved in intervention (on avoiding the need to travel and movement of patients). The authors compared a group of patients with face-to-face consultations with another of RTC; they found there were no significant differences in clinical control or satisfaction but these did exist in distance and money spent on each visit, in favour of RTC.
In our patient sample, the mean distance saved regarding RTC was over 30 km; 17% of the patients attended via teleconsultation lived over 50 km away. The mean time save was also notable in our study; the mean duration of the TC was under 10 min, whilst the mean time invested in the face-to-face consultation was 2 h. This saving of a journey means that the patient has fewer expenses and also a lower risk of accidents whilst driving their vehicle. Society also benefits in the reduction in fossil fuel consumption and global warming.
The ideal patient profile for RTC, according to our study, is a person with a higher educational level and skill in managing ICTs. The rheumatologists agreed that RTC could be used for successive visits when handing out the results of analyses or complementary tests or analyses and treatment adjustment.
Out study encompassed a wide patient sample, higher than many of the published studies.8,19–21 Also, it did not only research patients with inflammatory arthropathies,18,19 but also included a wide range of rheumatic processes and, above all, patients with osteoarthritis/rheumatism of soft tissue and osteoporosis. Many of our patients resided in rural areas, with difficult access to care by rheumatology specialists. In all of these circumstances, the RTC initiative was satisfactory and useful, in the opinion of the patient and the doctor, as was also detected in many other published studies.22–24 However, further research is needed to establish under what circumstances, with what protocols, for which diseases and in what phase of evolution the RTC may replace traditional face-to-face consultation.8,15,25,26
The COVID-19 pandemic has driven TC as a technological and organisational alternative which must allow our patients to be cared for under certain conditions, facilitate their access to the healthcare system and enhance patient safety and that of the rest of the population.11,27 The Spanish Medical College Organisation has established28 that RTC can replace and at times complete the face-to-face medical act because this is not possible, or advisable or because the benefit/risk weighting for the patient recommends it and provided that both parties are satisfied with the decision taken, which must be consensual and not imposed by either of the parties involved.
The TR executed in times of crisis like the one presented in this study was very highly appreciated by the patient and their rheumatologist. Although our patient sample is broad and much higher than that of other recently published studies,8 the generalisation of the results obtained here is controversial because it is a retrospective study and above all, because of the situation of confinement and the emotional impact derived from it, which probably many of our patients presented with. A randomized prospective study would also be needed with 2 groups of individuals, with a wide range of rheumatic processes, monitored in parallel, assessing the activity of the processes by objective and standardised measurements, including the analysis of outcome variables calculated by the patient. A comparison of the traditional face-to-face care, with RTC follow-up would be required. It would also be advisable to explore the usefulness or non usefulness of TR in initial consultations and circumstances which differed from that of home confinement.
TC is increasingly gaining in popularity.11,29,30 We conclude that its use and that of RTC in the evaluation and management of rheumatic disease at a critical time for rheumatology healthcare has been of great use. Rheumatic patients may be followed up and assessed by this procedure in a wide variety of rheumatic disease, including the control and follow-up of biological therapies. It is therefore possible to transfer rheumatological care activity towards TC with a high level of satisfaction for the patient and doctor.
Ethical responsibilitiesApproved by the Ethics Committee of the General University Hospital of Guadalajara.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Tornero-Molina J, Sánchez-Alonso F, Fernández-Prada M, Bris-Ochaita M-L, Sifuentes-Giraldo A, Vidal-Fuentes J. Telerreumatología en tiempos de crisis durante la pandemia por COVID-19. Reumatol Clin. 2022;18:157–163.