The use of technological environments with virtual reality (VR) techniques for the practice of arthrocentesis offers an effective and safe way to learn and improve the necessary skills to carry out a medical procedure and patient care. This article presents an interactive simulator using immersive VR, in which the participant experiences practicing clinical management and decision-making in the face of a person presenting with monoarthritis in a medical consultation. The objective with this development is for the user to acquire the competence to perform, correctly and safely, a knee arthrocentesis and to differentiate the types of synovial fluids that can be found in a joint. In turn, it provides clinical guidance and assists with the user's medical decision-making. Therefore, the aim is to improve the quality of care and patient safety when practicing this technique previously through clinical simulation.
El uso de entornos tecnológicos con técnicas de realidad virtual (RV) para la práctica de la artrocentesis ofrece una forma efectiva y segura de aprender y mejorar las habilidades necesarias para llevar a cabo un procedimiento médico y la atención a los pacientes. En este artículo se presenta un simulador interactivo mediante RV inmersiva, en la que el participante vive la experiencia de practicar el manejo clínico y la toma de decisiones ante una persona que presenta una monoartritis en una consulta médica. Nuestro objetivo con este desarrollo es que el usuario adquiera la competencia para realizar, de forma correcta y segura, una artrocentesis de rodilla y diferenciar los tipos de líquidos sinoviales que podemos encontrar en una articulación, proporcionar una orientación clínica y la toma de decisiones médicas. Con todo ello, se busca mejorar la calidad de la atención y la seguridad del paciente al practicar esta técnica previamente mediante simulación clínica con realidad virtual.
High quality medical education and training has to respond to society’s needs, which have an impact on all educational environments. Teaching systems in both universities and in health education are beginning to introduce changes, forcing teaching professionals to adopt new responsibilities based on the management and use of emerging technologies.
Clinical simulation has emerged as a powerful tool in the field of health sciences, revolutionising the way in which future professionals prepare to face real world challenges. In both medical teaching and training virtual environments enable participants to interact with simulated patients through technological procedures that emulate different clinical situations. In these environments students can practice, among others procedures, such as drug administration, wound dressing, catheter insertion, surgical procedures, ultrasound examination, and cardiac auscultation.1–8 The main advantage is to develop skills in different contexts and prepare for unusual or emergency situations. Everything takes place in a safe environment where practice can be repeated as many times as necessary to improve skill and confidence.9–11 We can therefore say that these methods offer a risk-free hands-on experience and promote an active, practical approach to learning rather than simply acquiring theoretical knowledge.12–14 The use of clinical simulation environments has been the subject of numerous evaluations and research studies which have sought to analyse the effectiveness and impact of simulation on learning, clinical skills and patient safety. Participants can apply concepts and skills in real-life situations, facilitating deep understanding and long-term retention. Students frequently experience anxiety during their first clinical practice sessions. Simulation gives them the opportunity to gradually approach these situations, reducing anxiety and increasing their confidence before working with real patients.15–22
Simulation systems often provide immediate and detailed feedback to participants on their performance. As a result, they can identify areas for improvement and hone their skills in real time, speeding up the learning process.23,24 Some of the problems that users may have when handling these VR technological procedures are: tripping, eye fatigue, dizziness, and headaches.25 However, these discomforts are gradually disappearing with the improvement in the quality of the VR glasses currently on the market.
Clinical management simulation of a patient with monoarthritisThis study presents an interactive simulator using immersive virtual reality in which the participant will experience practicing clinical management and decision-making for a person with monoarthritis of the knee during a medical consultation. The initial approach to the patient with monoarthritis constitutes a diagnostic challenge, even for the most experienced clinician. Any joint disease can begin as monoarthritis. Differential diagnosis is one of the most important in this case. The clinician’s priority is to identify patients with infectious arthritis since this may cause joint destruction in just a few hours.
To achieve this goal, it is essential to perform a good clinical history, a thorough physical examination and immediate analysis of the synovial fluid, completed with blood analysis and radiographic studies.
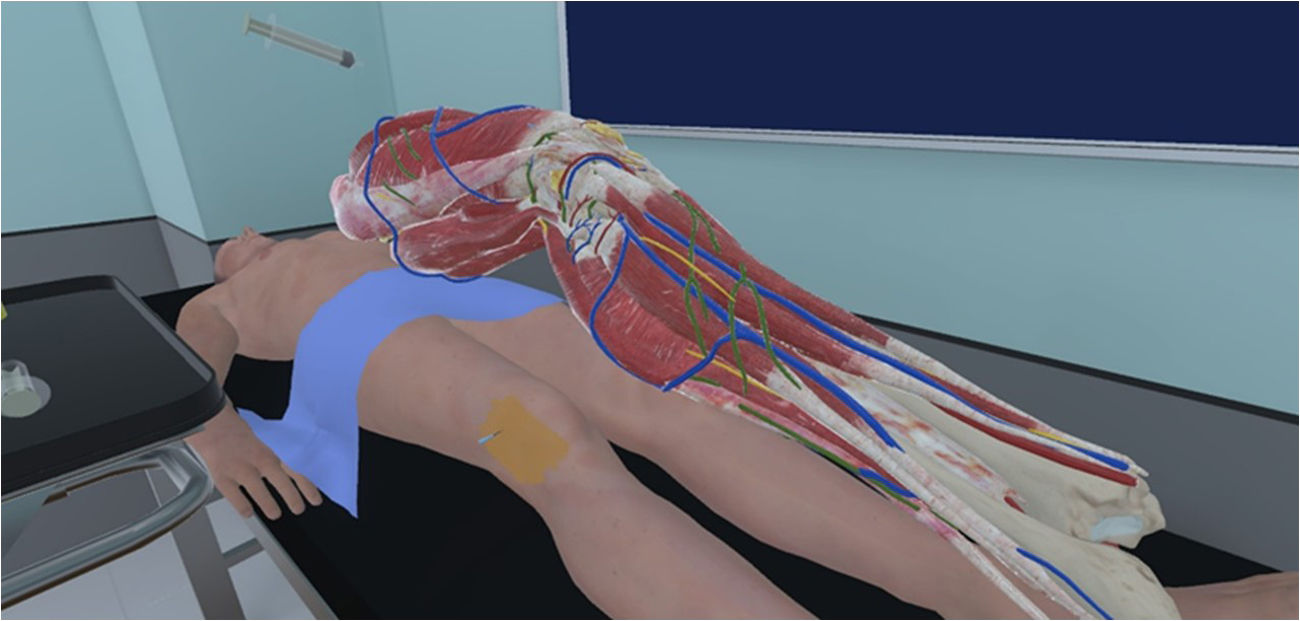
Our technological development has led us to aim at having participants learn to handle and experience the clinical approach to a person with monoarthritis, acquiring the skills to correctly perform a knee arthrocentesis, highlighting correct asepsis and the importance of recording the patient’s informed consent in the clinical history. To do this, we review the anatomical bases of the knee joint with a clinical focus, to serve as support for subsequent arthrocentesis and infiltration. In addition, we design various clinical scenarios to differentiate the different types of synovial fluids that can be found in a joint and provide clinical guidance, to properly use the storage and transport tubes for synovial fluid for its correct processing, to identify the most frequent crystals that cause arthritis due to their crystallographic characteristics and to clinically manage any suspicion of infectious arthritis.
Design of the technological developmentAny stimulation activity requires first determining the needs of the professionals to be trained, the skills required of that training and the teaching objectives. We designed various protocols for action with virtual reality techniques using stereoscopic vision glasses.
Technical applications usedWe used Unity 3D as a development engine. This has a series of programming routines that are operable in an interactive environment. Unity 3D is a multiplatform computer development engine that enables the creation of interactive 2D and 3D applications. It is known for its versatility and ability to develop content for a wide range of devices, including PCs, consoles, mobile devices and, especially, virtual reality experiences. Unity provides a visual development environment with an intuitive user interface that facilitates the creation and editing of content.
The programming language used with Unity was C++, through the Application Programming Interface (API) of scripting plugins (Unity Native Plugin) to improve performance. It is a small programming language whose code is inserted into HTML pages. These enable prototyping programmes, automating repetitive tasks, and interacting with the operating system and the user.
One of the main reasons for using the C++ language in Unity 3D was to improve performance, because it offers more precise control over memory management and application performance.
The Oculus Meta Quest 2 virtual reality (VR) headset (Fig. 1) was used, weighing 530 g and using a colour LCD screen with a resolution of 1,920 × 1,832. These headsets are equipped with the Snapdragon XR2 processor, which is considered to have a fast processing speed by today’s standards.
Development of the virtual learning environmentThe development of the virtual learning environment begins with the definition of the learning objectives to be achieved with the virtual environment. In other words, what specific concepts do we want to teach? What skills or procedures should participants practice: students, resident physicians or practicing physicians? In this way, specific goals are established to guide the outline of the virtual environment.
Our computer application starts from a visual environment of a waiting room (Fig. 2), before entering the clinician’s surgery (Fig. 3).
Once inside the surgery, the graphical interface for interaction with the user presents different types of screens that are located on the walls of the room and which we can access using the joystick controls. We began by choosing a clinical situation from 4 different scenarios, all based on a case of a patient with knee arthritis, which requires performing a diagnostic arthrocentesis.
We designed the protocol for the arthrocentesis procedure to be performed after medical indication. The procedure begins by obtaining the patient’s informed consent (the virtual room monitors indicate the need to provide information on the technique with its advantages and adverse effects, which the patient must accept and which must be reflected in the clinical history). This is achieved by bringing the portfolio closer to the virtual patient and subsequently validating the information by clicking on the mouse on the monitor on the table in the doctor's office. The patient is placed in a comfortable position on a bed to perform the puncture. We begin by washing our hands, preparing all the necessary material to perform the arthrocentesis and infiltration on a tray, putting on the gloves and proceeding to sterilise the joint area where the puncture will be performed. The arthrocentesis is then performed and the joint fluid is analysed. We finish the test by placing a sterile dressing on the puncture area. The sample is analysed visually on the syringe used to extract the synovial fluid and in the virtual laboratory with a microscope. The information panels in the virtual room are a guide to the steps to be followed during the procedure, showing educational material such as images or videos explaining basic concepts important for correctly carrying out the entire arthrocentesis or infiltration procedure (Figs. 4 and 5).
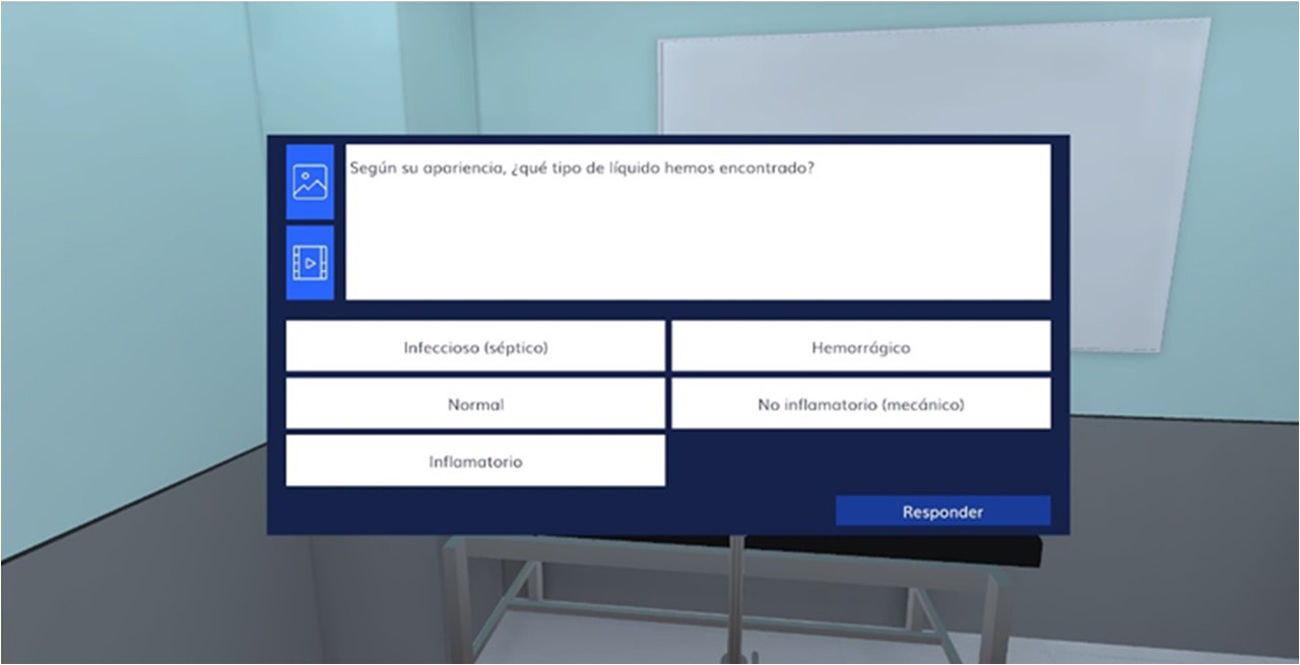
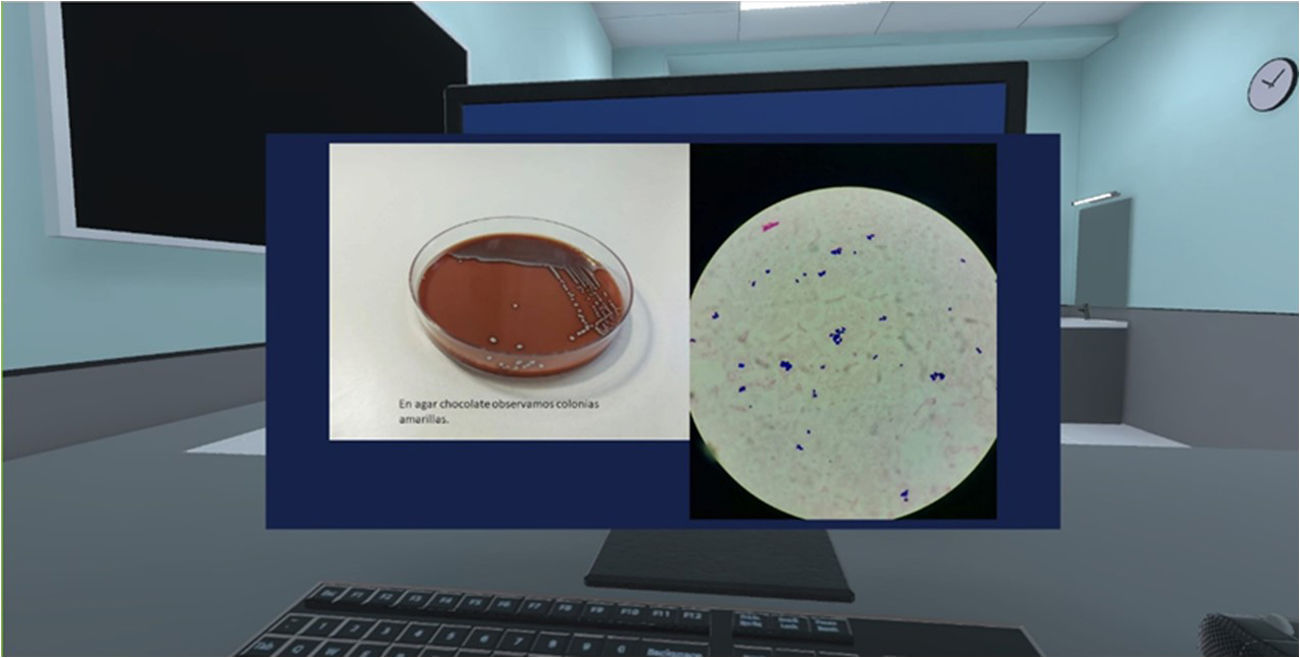
Throughout the procedure, the participant must resolve the questions that are posed to them, some of which are related to knowledge and others to decision-making (Fig. 6). We use images of synovial fluid in syringes, ultrasound images, as well as various preparations on slides to identify crystals using an optical microscope and cell cultures for microbiological analysis (Fig. 7).
We developed 4 training settings where the patient presented with arthritis of the knee.
In the first setting, the participant faces the situation of a patient with monoarthritis with mechanical characteristics, and must follow certain steps, answer questions and make decisions based on the information provided, and where they must perform an infiltration after arthrocentesis.
In the second setting, the participant has a patient with inflammatory monoarthritis where crystals are observed and, due to its crystallographic characteristics, they must diagnose the patient correctly and propose an appropriate treatment.
In the third setting, the situation is complicated by an infection, where correct action must be taken on a suspected diagnosis and early treatment with antibiotics must be applied.
The fourth setting consists of random steps with situations from any of the previous settings.
At the end of each setting, the score obtained is shown, differentiating the errors made and whether the diagnostic procedure and decision-making have been carried out correctly (Fig. 8) (Appendix B Additional material: explanatory video of the user's vision with VR glasses).
Results of the technological developmentWe tested the application on a group of 8 6th year medical students, 16 family medicine resident physicians and 4 rheumatology resident physicians, with a satisfaction level of 5 out of 5 points in 100% of the users. The students considered that this type of technological learning resources should be included in the medical subjects studied right from the beginning of medical school, in order to improve their learning. The resident physicians stated that the experience was relevant to their clinical practice, indicating that the virtual scenarios generated were of sufficient fidelity to develop a clinical experience such as the one proposed and that they had considerably improved their clinical skills in the management of a patient with monoarthritis. The resident physicians also felt more secure and confident to face real clinical situations after the virtual simulation. Two participants (7.1% of the users) suffered from “dizziness” with the use of virtual reality glasses, and this was resolved by performing the activity sitting on a chair.
Final considerationsVR techniques offer numerous applications in our field that lead to optimisation of medical training.1–8 This technological development allows the user to experience clinical management in a realistic setting within the doctor’s surgery. These technological teaching applications improve the training of the students who practice them and allow doctors in training to acquire experience in the execution of arthrocentesis, which results in a better performance when it has to be performed on a real patient. The simulator offers major advantages, the most notable being training in a safe environment to learn and perfect the arthrocentesis technique; the possibility of repeating the procedure as many times as necessary to acquire the necessary skill; allowing the participant to advance at their own pace in their learning process, and reducing the costs associated with the use of materials.
To conclude, the use of technological simulators with VR techniques demonstrates an innovative and updated approach in medical training. Further steps are required in the research and incorporation of these new technologies in healthcare training. With this project, the participant experiences a dynamic learning process on the clinical management of a patient with monoarthritis of the knee and the arthrocentesis technique, integrating theoretical and practical concepts simultaneously within a virtual visual environment.
FundingThis study was funded by the Prof. Novoa Santos and the Universidade da Coruña foundations.
The authors have no conflict of interests to declare.
We would like to thank Santiago González Izard, director of the ARSoft company, from the scientific park of the University of Salamanca, for his collaboration in the technological development of our teaching computer application.