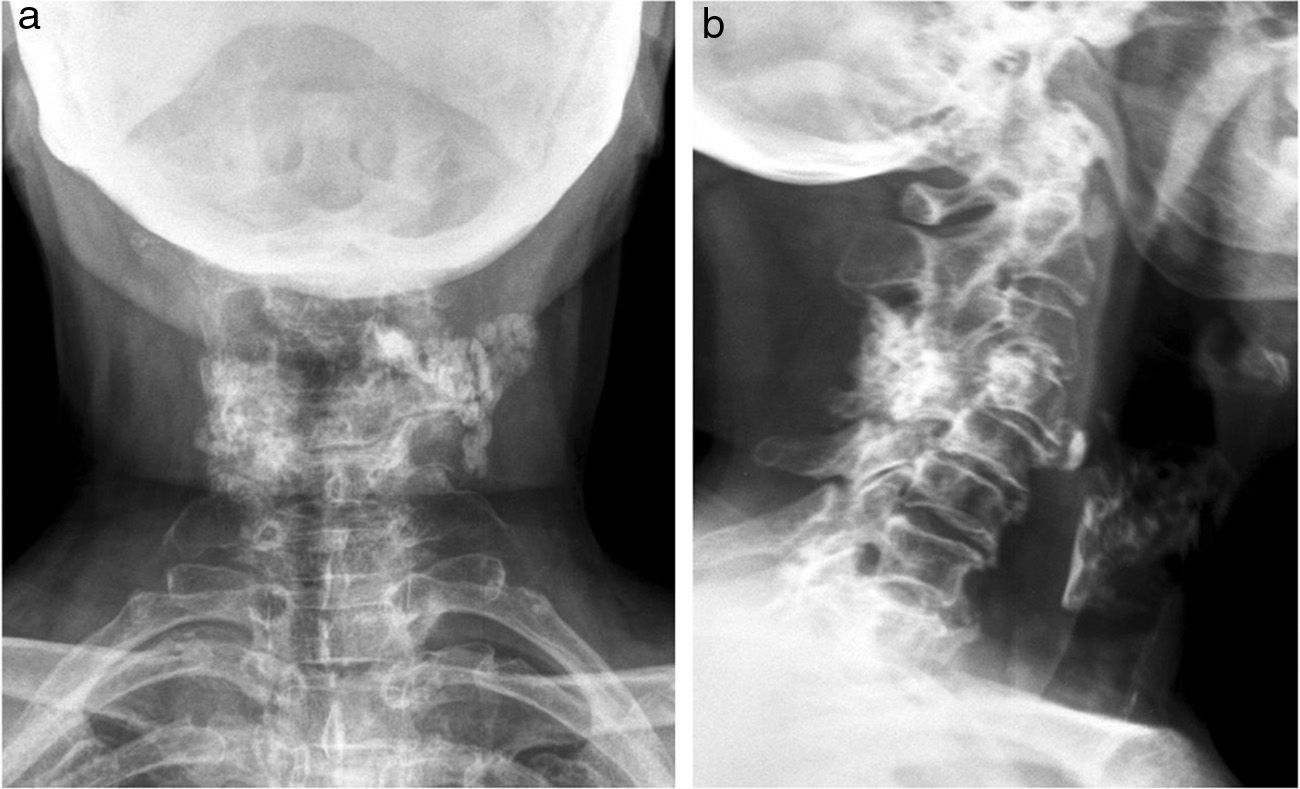
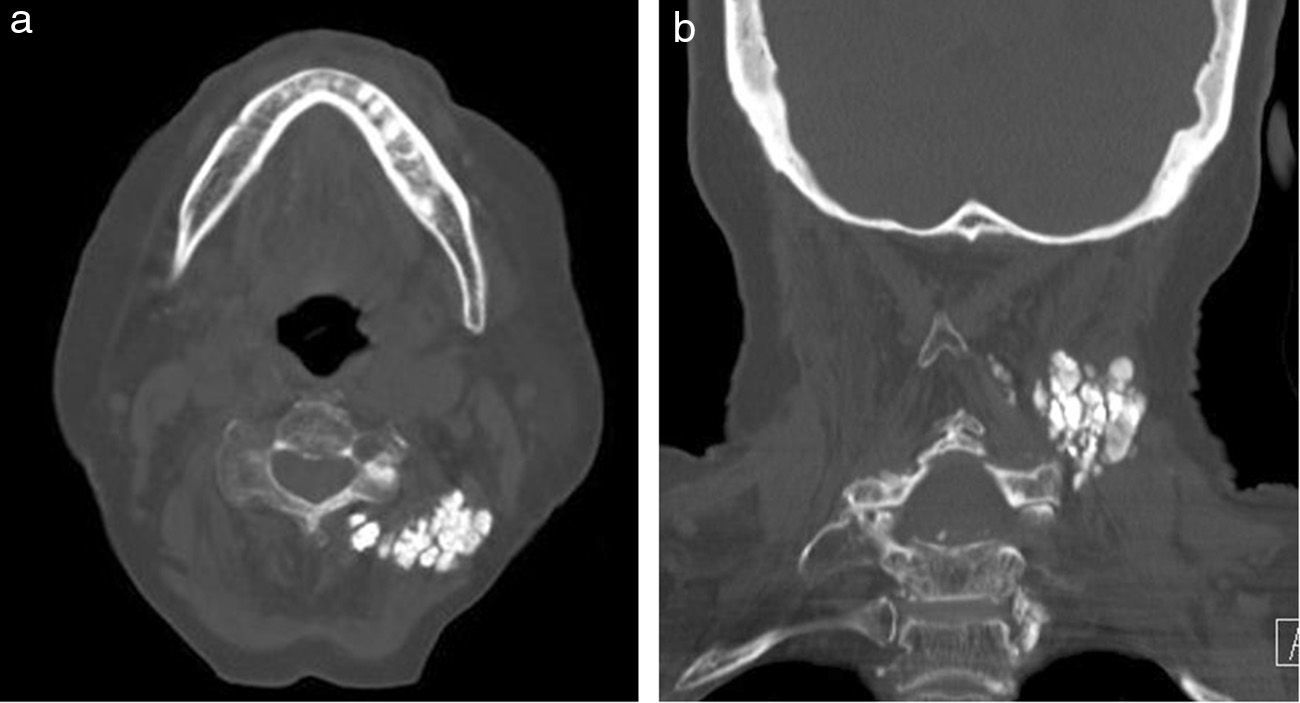
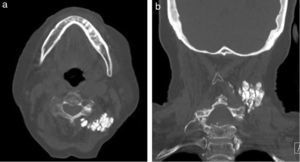
The patient was an 81-year-old woman who had hypertension, dyslipidemia, asthma and limited systemic sclerosis (LSS). Scleroderma was diagnosed 5 years prior due to finger calcinosis, sclerodactylia and positive anticentromere antibodies. She had no Raynaud's phenomenon or any other clinical data and was not followed by rheumatology. She came to the clinic due to inflammatory neck pain that did not irradiate, which had lasted for several months and a painful left cervical mass. The patient had resting dyspnea, no cough, dysphagia fever, weight loss or malaise. Under examination she had osteoarthritis on both hands, sclerodactylia, telangiectasias and calcifications on the fingers, some of them with ulcers. Spinal mobility was limited anteriorly, posteriorly and laterally, without signs of neurological affection. There was a solid and painful 4cm mass fixed to deep tissue on the left side of her neck. A simple X-ray of the spine was performed which revealed soft tissue calcification and osteoarthritis of the neck (Fig. 1). A cervical CT scan reveals a massive calcification of the paravertebral muscles at C3 (Fig. 2). Laboratory analysis showed no bone mineral or renal alterations.
DiscussionSoft tissue calcifications may be classified into: metastatic, tumoral, calciphilaxis-related, dystrophic and idiopathic. Calcinosis belongs to the dystrophic group and is found in hypoxia damaged tissues. Phosphocalcic metabolism is normal. It is associated to systemic lupus erythematosus, systemic sclerosis and dermatomyositis.1,2
Calcinosis is closely related to systemic sclerosis, especially in its limited form, and with positive anticentromere antibodies.1,3 It is usually characterized by small calcifications on sites of repeat microtrauma such as elbows, fingers and forearms.1,3 Paraspinal calcinosis is unusual and is possibly underdiagnosed. Cervical and lumbar localizations are easier to diagnose due to their clinical manifestation. A study by Ogawa et al. detected paraspinal thoracic calcinosis in 58.5% of patients with LSS who underwent a thorax CT while asymptomatic.4 In the case of our patient the calcification was large and extended through several spinal levels as described by Schweitzer et al. in their review.5 It is often associated to Raynaud's phenomenon, digital ulcers and skin calcinosis (as in this case).6 Some therapeutic options, such as diltiazem, steroids, colchicine, biphosphonates, probenecid, mynocyclin, kelating agents and warfarin, have been employed without a lot of benefit.1,6,7 Our patient was treated with nifedipine 10mg every 8h and non-steroidal anti-inflammatory drugs for pain, with improvement and is now clinically stable. Surgery is described as an option for neurological complications.6,7
Ethical ResponsibilitiesProtection of persons and animalsThe authors state that no experiments were performed on persons or animals for this study.
Data confidentialityThe authors state that they have followed their workplace protocols regarding the publication of patient data and all patients included in the study have received enough information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors state that they have obtained informed consent from patients and/or subjects referred to in this article. This document is in the possession of the corresponding author.
Please cite this article as: Contreras I, Sallés M, Mínguez S, Tuneu R, Gelman SM. Tumoración pétrea paracervical en paciente con esclerosis sistémica forma limitada. Reumatol Clin. 2013;10:336–337.