Schnitzler's syndrome is a disorder first described in 1972. It was published in 1974 by Liliane Schnitzler, a French dermatologist, as an autonomous entity.
It is characterized as a rare, acquired syndrome, which shares common characteristics with a group of inherited diseases known as the autoinflammatory syndromes. It has been described most often in men between the fourth and fifth decades of life. Its etiology is unknown, but has been associated with conditions such as impaired balance of interleukin-1. The presenting symptoms are fever, rash and joint pain; there may also be lymphadenopathy and an IgM monoclonal component. 15%–20% of patients with this entity develop a lymphoproliferative syndrome. Conventional treatments are ineffective, and they include antihistamines, anti-inflammatory drugs, corticosteroids and immunosuppressants.
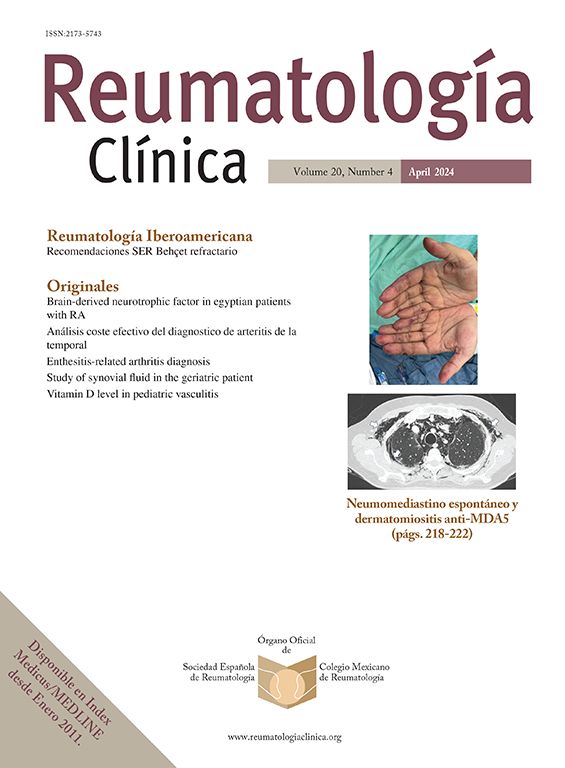
We report the case of a 65-year-old male patient with no medical history, with a 10-year history consisting of intermittent fever, joint pain of moderate intensity, scattered maculopapular pruritic skin lesions located on the thorax, abdomen and lower extremities. Three months before our evaluation he developed back pain radiating to the left lower extremity, non-continuous but intense that prevented walking. The general examination showed the presence of a maculopapular rash on the chest, abdomen and extremities, as well as a positive Lassegue sign on the left leg.
Lab tests, including complete blood count, biochemistry, coagulation, serology, tumor markers, serum protein and immunoelectrophoresis, were normal, except for the presence of monoclonal IgM kappa and increased erythrocyte sedimentation rate (ESR).
The skin lesion was biopsied. Histologic examination showed a superficial perivascular lymphocytic infiltration, interstitial dispersion and some neutrophils along collagen bundles.1 A cervical, thorax and abdomen computed tomography was performed, which showed no significant findings.
Given the different hematological findings, we performed aspiration/biopsy of bone marrow, which was consistent with Waldenstrom's disease. The patient is now in outpatient follow-up. No chemotherapy was started and has remained on symptomatic treatment only.
Schnitzler's syndrome is a rare entity which is difficult to diagnose given the absence of peripheral biomarkers and the need for confirmation of the diagnosis by a combination of clinical, laboratory and radiological tests as well as the exclusion of other diseases.
To date, on the basis of criteria proposed by Lipsker et al. no more than 60 cases have been described. These criteria include the presence of an urticarial skin rash and a monoclonal IgM component and at least two of the following signs or symptoms: fever, joint pain or arthritis, bone pain, palpable lymph nodes, spleen, hepatomegaly, accelerated ESR and leukocytosis.2,3
Our patient met criteria for Schnitzler syndrome, since some clinical (urticarial rash and fever) and laboratory findings (monoclonal IgM peak and increased ESR) present.
Among the various forms described above as part of the development of the disease, some authors include developing lymphoproliferative syndrome as lymphoplasmocytic lymphoma, Richter's syndrome, and4 marginal lymphoma.
The differential diagnosis of Schnitzler's syndrome should be performed with different entities, namely: cryoglobulinemia, hypocomplementemic urticarial vasculitis, acquired deficiency of C1 inhibitor, hyper IgD syndrome and adult Still's disease.
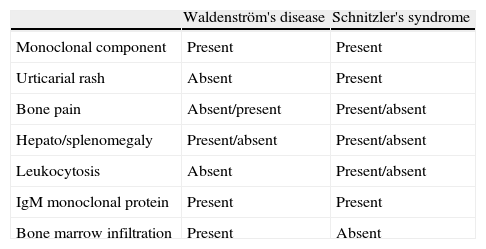
The interest of this article is that the presence of monoclonal IgM, and the histology of skin lesions were alterations leading to the diagnosis of Schnitzler's syndrome with progression to Waldenstrom's disease. It should be stressed that a good history is essential, as it allows to know the exact nature of its evolution. Finally, we emphasize the importance of a differential diagnosis between1 Schnitzler's syndrome and Waldeströn's disease (Table 1) as well as the importance of knowing this entity to prevent the diagnosis from going unnoticed.
Differences Between Schintzler's Syndrome and Waldeström's Disease.
| Waldenström's disease | Schnitzler's syndrome | |
| Monoclonal component | Present | Present |
| Urticarial rash | Absent | Present |
| Bone pain | Absent/present | Present/absent |
| Hepato/splenomegaly | Present/absent | Present/absent |
| Leukocytosis | Absent | Present/absent |
| IgM monoclonal protein | Present | Present |
| Bone marrow infiltration | Present | Absent |
Please cite this article as: Herráez Albendea MM, et al. Síndrome de Schnitzler. Reumatol Clin. 2013;9:384.