To assess and improve the level of implementation of the recommendations for the psychological management of patients with spondyloarthritis (SpA) and associated inflammatory bowel disease (IBD).
MethodsQualitative study. We performed a narrative literature review to identify the recommendations for the psychological management of SpA and associated IBD and to explore their level of implementation. Based on the findings, we developed a national survey to assess: (1) current level of knowledge and implementation of the recommendations; (2) attitudes towards the recommendations; and (3) barriers and facilitators to their implementation. The results of the review and survey were discussed by a multidisciplinary group of 9 expert rheumatologists and gastroenterologists, who defined implementation strategies to increase the uptake of the recommendations.
ResultsThe review included 4 articles, 2 of them included direct recommendations on the identification and management of psychological problems in patients with SpA and IBD. None assessed the level of implementation of the recommendations in routine clinical practice. Our survey showed a great lack of awareness and implementation of the recommendations, even though psychological issues are very relevant for health professionals. Lack of time, resources, and knowledge are considered the main barriers to adherence to the recommendations. We propose several implementation strategies related to educational activities, clinical practice, and others to increase the uptake of reported recommendations.
ConclusionsFurther research and efforts are required to achieve behaviour changes in clinical practice to improve the identification and management of psychological problems and needs in patients with SpA and IBD.
Analizar y mejorar la implementación de las recomendaciones sobre la evaluación y el manejo psicológico de pacientes con espondiloartritis (EspA) y enfermedad inflamatoria intestinal (EII) asociada.
MétodosEstudio cualitativo. Se realizó una revisión narrativa de la literatura para identificar las recomendaciones sobre el manejo psicológico de pacientes con EspA y EII asociada y explorar su grado de implementación. En base a ello se diseñó una encuesta para analizar el nivel de conocimiento de las recomendaciones, las barreras y los facilitadores a su implementación. Todos los resultados fueron discutidos por un grupo multidisciplinar de expertos reumatólogos y gastroenterólogos que definieron estrategias para incrementar el seguimiento de las recomendaciones.
ResultadosLa revisión incluyó 4 artículos, de los que 2 aportan recomendaciones directas sobre la evaluación y el manejo psicológico de pacientes con EspA y EII. Ninguno ha evaluado el grado de implementación de las recomendaciones en la práctica diaria. La encuesta mostró que el conocimiento de las mismas y la implementación de estas recomendaciones son prácticamente nulos a pesar de ser un tema muy relevante para los profesionales que manejan estos pacientes. La falta de tiempo, la escasez de recursos y la falta de reconocimiento se consideran las principales barreras para la correcta identificación y manejo de los aspectos psicológicos en pacientes con EspA y EII. Se proponen una serie de actividades formativas y relacionadas con la práctica clínica para mejorar esta situación.
ConclusionesSe precisa seguir trabajando en la implementación para conseguir cambios en la práctica diaria para mejorar la evaluación y el manejo psicológico de los pacientes con EspA y EII.
It is estimated that 6% of patients with spondyloarthritis (SpA) have inflammatory bowel disease (IBD),1 and vice versa, between 2 and 45% of patients with IBD have SpA.2–4 Further, it is considered that these figures may be an underestimate.
Both SpA and IBD are diseases that have a major psychological prevalence and impact on patients.5–7 It is estimated that around of 15% of patients with SpA present depression,8 and poor sleep is reported in 35–90% of patients.9 Up to 66% of patients with IBD might present impaired sexual function.10 Around 70% of these patients have reported at least one work related issue.11,12 It has also been reported that patients with uncontrolled psychological conditions use healthcare services more often (unplanned visits, telephone consultations, emergency department attendance), have lower treatment adherence and poorer quality of life and work outcomes.11,13–18 All this indicates that these patients could benefit from psychological intervention. However, several studies have revealed differences between healthcare professionals and patients regarding to psychological issues, but also objectified a lack of specific training for identifying and managing the psychological sphere of these patients.19,20
In recent years, various initiatives have been carried out in the areas of rheumatology and gastroenterology to increase awareness about the psychological problems of patients with these diseases and also to provide a framework and tools for their identification and management. Specifically, in 2018, the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) and the Spanish Federation of Crohn's & Ulcerative Colitis Associations (ACCU) published a consensus document on psychological problems in IBD patients.21 In the same year, another expert report was published which, although in principle focused on patients with rheumatoid arthritis, the authors considered could also be useful for other conditions such as SpA.22 Since then, various other studies have been published on emotional/psychological factors in these patients.23,24 Recently, a study in RA and EspA patients found that psychological flexibility variables (valued activity, mindfulness, cognitive fusion, and fatigue avoidance) are directly associated with fatigue-related disability. This suggests that interventions that target psychological flexibility could be effective at reducing fatigue-related disability.25
As various years have passed since the aforementioned initiatives were reported, we considered that the management of these patients in routine practice might have changed, and this might have had a positive impact from a psychological point of view. Therefore, we designed this study to analyse current level of implementation of the recommendations for the psychological management these patients and to design strategies to improve the adherence to them. For these purposes, we performed a qualitative study based on a literature review, a survey and experts opinion.
MethodsA qualitative study was conducted. The study coordinator and the methodologists defined the study phases that included a narrative review, a survey and a meeting with a multidisciplinary group of experts in SpA and IBD.
Narrative review of the literatureThe objective of the review was to describe and to explore the level of implementation of recommendations related to the psychological management of patients with SpA and IBD in routine clinical practice. We designed various search strategies in PubMed using the Clinical Queries function that combines Medical Subject Headings (MeSH) and free-text terms. Terms used included “spondyloarthritis”, “inflammatory boweldisease”, “psychological” and “emotional”.
The following eligibility criteria were applied: (1) Regarding the population, we included studies of adult patients (>18 years old) with SpA and IBD (according to international criteria), regardless of disease duration, severity or pharmacological treatment; (2) The interventions were required to involve either previously published or new recommendations on the psychological management of these patients; (3) No restrictions were set concerning the comparator (not even requiring there to be one); (4) As outcome measures, any related to the development and/or level of implementation of recommendations were allowed, including the evaluation of the efficacy of the implementation (early detection of depression, patient satisfaction, etc.). Regarding the type of study, we included meta-analyses, systematic literature reviews, clinical trials, and observational and qualitative studies, but excluded animal studies and basic research.
All the records retrieved using the search strategy were entered into Endnote® reference Management software. First, duplicates were removed. After this, two reviewers (EL and TO) screened the references independently and in duplicate and subsequently analysed the articles included in detail. The search results were first screened by title and abstract or by full text reading, if there was no abstract, in sessions lasting no longer than 60min. After this process, the articles selected were analysed in detail (full text reading).
The two reviewers independently and in duplicate collected data from the studies included using forms developed for the purposes of this review. The 2011 Oxford Centre for Evidence-Based Medicine Levels of Evidence were used to assess the methodological quality of the studies included.26 A qualitative descriptive analysis was performed.
Design of the survey and variablesThe aim of the survey was to analyse current level of knowledge and implementation of the recommendations regarding the psychological management of patients with SpA or IBD and related documents that were found in the literature review.21–24 We followed general recommendations for the development of surveys,27 and used a web-based tool (SurveyMonkey©), that generated structured and closed questions (a total of 30). In a first step, based on the published documents,21–24 we identified the recommendations and developers comments suggesting further difficulties regarding their implementation. Therefore, we also evaluated barriers and facilitators to the implementation of the recommendations. Then, taking into account care decentralisation in our country, it was decided to collect data connected to participants regional and hospital characteristics background. Questions were direct and short. Depending on the objective, closed-ended questions included one choice, multiple choice, checkboxes, and ranking questions. The survey as organised in 4 sections that included several questions to collect the following variables: (1) sociodemographic data like age, sex, region of residence, type of hospital (primary, secondary or tertiary level, private clinic or other), years worked, and whether working in an SpA specialised clinic or as part of a multidisciplinary team; (2) assessment of patients’ emotional/psychological status including frequency, impact, person(s) responsible, methods, relationship with SpA, IBD or both, use of effective communication models, motivational interview, and the evaluation of patients’ environment; (3) variables concerning the management and prevention of emotional/psychological problems, such as whether achieving a euthymic state is a treatment goal, shared decision making, allowance of time in appointments for informing patients, people responsible for managing psychological disorders, other related recommendations, and the existence of protocols for referral to mental health professionals; and (4) barriers and facilitators to the implementation of recommendations.21,22 A pilot study was carried out. Two rheumatologists outside the study completed the survey and provided comments. There was no formal validation of the survey.
Given the characteristics of the survey and its objectives, we used a convenience sampling based on a list of members of the Spondylarthritis Research Group of the Spanish Society of Rheumatology (GRESSER), inviting each of them to complete the questionnaire by email. GRESSER includes an extensive group of health professionals with interest in SpA from all around the country. Some of the members are well-recognized experts on the disease (including rheumatologists but also other specialists like gastroenterologist and health professionals as nurses) but in GRESSER there are also many clinicians and health professionals that are not considered experts or researchers. The survey front page included information about the survey, describing the objectives of the project and asking for their voluntary participation. By reading and responding, the health professionals gave their consent. The survey was run between 30 October and 17 November 2021.
Data were downloaded from SurveyMonkey© in Excel format. Data analysis was performed using Stata 12© statistical package (Stata Corporation, College Station, TX, USA). A descriptive analysis of the data was carried out. Quantitative variables were described using means (standard deviations) and qualitative variables using frequencies (percentages).
Nominal group meetingWe stablished a multidisciplinary group of 9 expert rheumatologists and gastroenterologists. The criteria for the selection were: (1) clinical experience ≥8 years and/or ≥35 publications on SpA or IBD in the last 5 years; (2) work in a SpA/IBD unit or multidisciplinary team; and (3) members of National and International Societies and related working groups. First, the results of the narrative review were presented by the project methodologists in a nominal group meeting. Then the experts analysed and discussed all of this information. Afterwards, the methodologists opened a discussion about the characteristics of the provision of clinical care across the country. One of the methodologists assured participation of all of the experts during the meeting. If necessary direct questions were performed. Following the experts, guided by the methodologists, and based on the previous discussions formulated the strategies and actions to improve the psychological management of patients with SpA and IBD. There was no limit to the number or type of strategies. Each strategy was closed only once all of the experts verbally agreed with the message and wording. Thus, we did not performed a Delphi process.
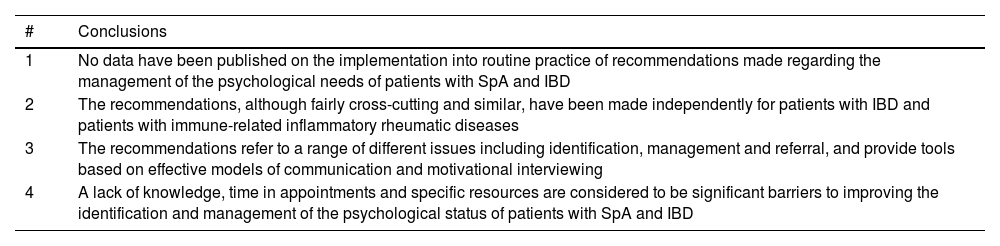
ResultsNarrative review of the literatureOur search identified 27 records. After removing 5 duplicates, the remaining articles were read in detail. Finally, we included 4, all of which were high quality consensus reports or similar types of document; 3 focused on IBD and the other on rheumatic diseases.21–24 Two of these documents contained recommendations focused on the psychological management of patients, while in the other two, the recommendations concerned patients’ preferences and improving treatment adherence. None of the documents analysed the level of implementation of the recommendations made. The main conclusions are summarised in Table 1 (see Tables 1 and 4 in the Supplementary Material for further information).
Main conclusions of the narrative review.
| # | Conclusions |
|---|---|
| 1 | No data have been published on the implementation into routine practice of recommendations made regarding the management of the psychological needs of patients with SpA and IBD |
| 2 | The recommendations, although fairly cross-cutting and similar, have been made independently for patients with IBD and patients with immune-related inflammatory rheumatic diseases |
| 3 | The recommendations refer to a range of different issues including identification, management and referral, and provide tools based on effective models of communication and motivational interviewing |
| 4 | A lack of knowledge, time in appointments and specific resources are considered to be significant barriers to improving the identification and management of the psychological status of patients with SpA and IBD |
Abbreviations: SpA=spondyloarthritis; IBD=inflammatory bowel disease.
In general, the recommendations address the detection/identification, management (including referral to mental health specialists) and prevention of psychological problems in this group of patients. They also indicate the need to take special care in certain circumstances such as the diagnosis, during disease flares, and when a patient is admitted to hospital.21–24
Regarding what is to be identified, considering prevalence rates, impact and tools to assess their presence, the authors of the documents recommend the screening for depression, anxiety, and specifically, sexual problems.21–24 If such psychological problems are identified, their impact on individual patients should also be evaluated.21−24 In order to analyse psychological needs, the recommended approach is to use a clinical interview and questionnaires such as the Hospital Anxiety and Depression Scale (HADS) for depression.21,22 In this context, it is also recommended to examine patients’ family, social and work environments.
The included documents place particular importance on the information given to patients,21–24 more specifically, the type of information that should be given at each moment and how. The more this information and communication is tailored to patients’ characteristics and preferences, the less psychological impact and the more improvement on treatment adherence.23,24
On the other hand, in general, all the documents mention the use of effective models of communication (active listening, use of open questions) and motivational interviews to contribute positively not only to identify and manage psychological problems but also to prevent them.21–24 It is also highlighted that all of this is responsibility of all health professionals involved in the management of patients with SpA and IBD,21–24 but also that the specific management of psychological and psychiatric problems should be undertaken by mental health professionals, and for this reason, various referral criteria have been proposed. Some of the authors recommend as well to analyse the needs and psychological well-being of patients’ relatives, given that family members’ problems might be a source of stress for the patient and they might also need psychological support.22
Some of the documents identify barriers and facilitators to the implementation of the recommendations. One of the included articles showed certain barriers to the incorporation of patients’ preferences into routine clinical practice.24 In relation to clinicians, the lack of empathy and/or knowledge of the psychological and affective needs of patients were considered major barriers, and concerning the health system, the limited human resources, short appointment times, especially in primary care, and the variability in the access to services between regions, and even among hospitals within the same region, were identified as barriers to the incorporation of patients’ preferences.24 In this document, the panel highlighted that both nurses and primary care physicians could play a key role as facilitators in this context, the same as training clinicians in motivational interviewing and the development of specific protocols that integrate patients’ preferences into the decision making.
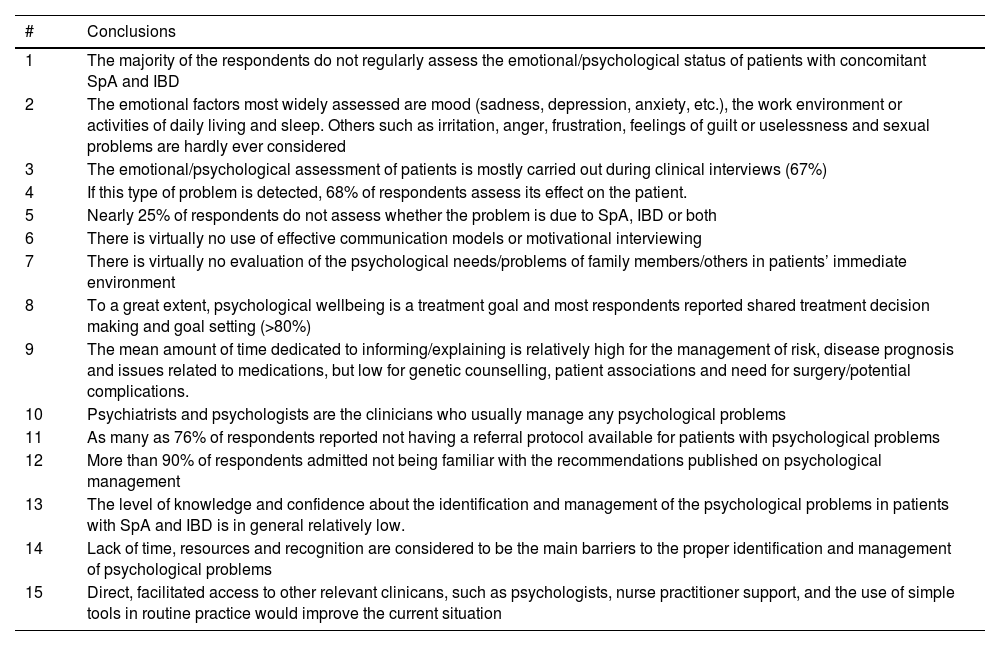
SurveyA total of 35 surveys were completed corresponding to health professionals from most of the country regions. The main results are summarised in Table 2 (see Tables 5 to 30 in the supplementary material for more information).
Main conclusions of the survey.
| # | Conclusions |
|---|---|
| 1 | The majority of the respondents do not regularly assess the emotional/psychological status of patients with concomitant SpA and IBD |
| 2 | The emotional factors most widely assessed are mood (sadness, depression, anxiety, etc.), the work environment or activities of daily living and sleep. Others such as irritation, anger, frustration, feelings of guilt or uselessness and sexual problems are hardly ever considered |
| 3 | The emotional/psychological assessment of patients is mostly carried out during clinical interviews (67%) |
| 4 | If this type of problem is detected, 68% of respondents assess its effect on the patient. |
| 5 | Nearly 25% of respondents do not assess whether the problem is due to SpA, IBD or both |
| 6 | There is virtually no use of effective communication models or motivational interviewing |
| 7 | There is virtually no evaluation of the psychological needs/problems of family members/others in patients’ immediate environment |
| 8 | To a great extent, psychological wellbeing is a treatment goal and most respondents reported shared treatment decision making and goal setting (>80%) |
| 9 | The mean amount of time dedicated to informing/explaining is relatively high for the management of risk, disease prognosis and issues related to medications, but low for genetic counselling, patient associations and need for surgery/potential complications. |
| 10 | Psychiatrists and psychologists are the clinicians who usually manage any psychological problems |
| 11 | As many as 76% of respondents reported not having a referral protocol available for patients with psychological problems |
| 12 | More than 90% of respondents admitted not being familiar with the recommendations published on psychological management |
| 13 | The level of knowledge and confidence about the identification and management of the psychological problems in patients with SpA and IBD is in general relatively low. |
| 14 | Lack of time, resources and recognition are considered to be the main barriers to the proper identification and management of psychological problems |
| 15 | Direct, facilitated access to other relevant clinicans, such as psychologists, nurse practitioner support, and the use of simple tools in routine practice would improve the current situation |
Abbreviations: SpA=spondyloartritis; IBD=inflammatory bowel disease.
More than 90% of participants were not aware of the published recommendations on the psychological management of SpA and IBD. Further, despite recognising the relevance of patients’ psychological wellbeing (considered as a treatment goal), the emotional/psychological status of patients with these conditions is not routinely assessed in clinical practice. The same regarding the psychological needs of patient's family and environment. In line with this, the level of knowledge and comfort connected to the identification and management of psychological factors in patients with SpA and IBD was generally low. Lack of time, resources and recognition of psychological problems are considered the main barriers to the proper identification and management of psychological problems in this population.
The aspects of emotional well-being/psychological health most commonly assessed in daily practice were patients’ mood, work environment, daily activities and sleep quality. Others such as anger, frustration and sexual problems were rarely evaluated. If an emotional/psychological is detected, nearly a third (30%) of participants did not evaluate its impact on patients, and around three-quarters (76%) lacked a protocol for referring patients with psychological problems to a mental health professional. We also found that most of participants do not use effective communication models, motivational interviews or related tools.
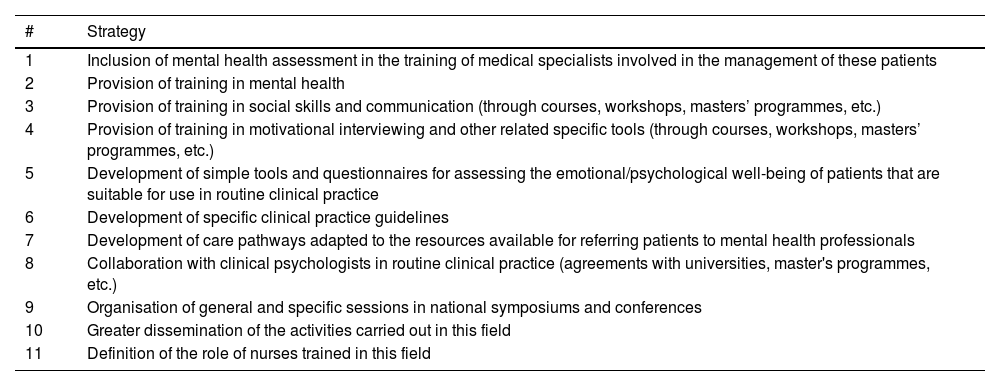
Strategies and actions for improving implementation of the recommendationsTable 3 summarises the strategies and other actions proposed to improve the recommendations on the identification and management of psychological problems in patients with SpA and IBD. The panel of experts recognises a lack of knowledge and implementation of the recommendations published on the psychological management of patients with SpA and IBD, even in highly specialised units, and despite emotional/psychological problems are considered very relevant by clinicians.
Main strategies and actions to improve the psychological management of patients with SpA and IBD.
| # | Strategy |
|---|---|
| 1 | Inclusion of mental health assessment in the training of medical specialists involved in the management of these patients |
| 2 | Provision of training in mental health |
| 3 | Provision of training in social skills and communication (through courses, workshops, masters’ programmes, etc.) |
| 4 | Provision of training in motivational interviewing and other related specific tools (through courses, workshops, masters’ programmes, etc.) |
| 5 | Development of simple tools and questionnaires for assessing the emotional/psychological well-being of patients that are suitable for use in routine clinical practice |
| 6 | Development of specific clinical practice guidelines |
| 7 | Development of care pathways adapted to the resources available for referring patients to mental health professionals |
| 8 | Collaboration with clinical psychologists in routine clinical practice (agreements with universities, master's programmes, etc.) |
| 9 | Organisation of general and specific sessions in national symposiums and conferences |
| 10 | Greater dissemination of the activities carried out in this field |
| 11 | Definition of the role of nurses trained in this field |
Abbreviations: SpA=spondyloarthritis; IBD=inflammatory bowel disease.
For this reason, and as a first step, the panel considered it essential to include mental health as part of the knowledge and skills of medical specialists involved in the management of these patients. They should acquire, since the medical training, relevant general knowledge; and more specifically, social and communication skills including how to conduct motivational interviews and their use in routine clinical practice. Although no studies have yet demonstrated their efficacy, the panel stated that their use might save time in the mid- to long term. All this could be accomplished through courses, workshops, masters’ programmes, etc.
For routine clinical practice, as well as what has been mentioned above, the panel proposed the generation and addition of specific questionnaires, questions or other resources related to the psychological status and needs of patients (simple, implementable). For example the HADS to suspect depression or the ASAS Health Index (ASAS-HI). On the other hand, the recruitment of clinical psychologists is currently very complicated due to lack of resources, but it might be possible to find ways to collaborate directly with psychologists through universities, masters’ courses, etc. Along with this, the panel consider it very important to establish clear referral pathways for patients in whom psychological problems are detected and who, according to established criteria, require specialised mental health care.
From a more institutional perspective, and in close collaboration with scientific societies, working groups and patients’ associations, a series of activities are proposed including the development of overall management guidelines for psychological problems, courses, and specific sessions in national scientific meetings and conferences.
DiscussionIn this project, we have shown that, despite a general awareness among clinicians of the prevalence, severity and impact of emotional/psychological problems of SpA and IBD patients,5–7 available recommendations for identifying and managing them are practically unknown and their level of implantation is really low.21–24
The dissemination of evidence-based recommendations is considered a key step for improving the quality of care. However, simple dissemination of information has rarely been effective in changing clinical practices and behaviour.28,29 More specifically, adherence to and uptake of recommendations is often sub-optimal.30,31 This is critical as it has been demonstrated the benefit of the adherence to clinical recommendations.32,33
Several high-quality multidisciplinary documents have been published in rheumatology and gastroenterology concerning the identification and management of patients’ psychological problems and needs.21–24 However, the results of our survey show a very low level of knowledge and implementation of these recommendations, which suggests the need of a careful analysis of our context and to design adapted implementation strategies to overcome this scenario. In this regard, the survey found several barriers at different levels of care. At the meso-level (health system level) it was clear the lack (but also variability) of resources for a proper identification and management of emotional/psychological problems and needs. Current work load in daily practice limits the time of clinical consultation. This probably have led health professionals to focus on other aspects of the disease like activity or structural damage and not on the psychological dimension. Other articles have showed similar results.34–36 But in this context it is vital to mention that the access to mental health professionals like psychologists and others is very limited. To overcome this barrier we have proposed to look for collaborations with psychologies through universities, research projects or masters, but also to increase collaboration in the hospital with mental health professionals generating referral programmes.
At the micro-level (health professionals level), we would like to highlight two main points. The first one is the lack of knowledge of the consensus documents that have been already published.21–24 It is important to mention that one of them was promoted by a national scientific society and a patients association.21 Besides, all of them were developed by national experts following the required methodology and were published in well-known journals. Numerous studies have also demonstrated a low level of implementation of recommendations generated in high-quality consensus documents in rheumatology and gastroenterology.30,31 This should encourage consensus developers to design implementation strategies beyond a simple publication to increase the visibility and adoption of the recommendations. For example by organising specific sessions in scientific meetings, through key opinion leaders, etc.
At the micro-level along with a lack of implementation we have reported a great variability in the recommendations that apparently are already implemented. And, as also detected in the survey this might reflect a lack of knowledge and training in how to identify and manage psychological problems and needs of our patients, not having enough staff to perform this task and lack of practical evaluation tools. This is in line with the data of other publications.30,31,34–36 Following the principles of the implementation science,37 the experts proposed a set of strategies to achieve changes in clinical practice, most of them were educational proposals. But the experts also the use of practical tools (questionnaires, questions or checklists) that have proven efficacy to identify/manage psychological issues. The HADS for depression has been extensively described and it is easily implemented in daily practice.21,22 The same way, the ASAS-HI,38 is disease specific and measures overall functioning and health. It is very suitable for busy clinics and provides valuable data regarding the psychological status of the patients. Recently it has been published that the implementation of a specific checklist (that includes psychological issues) in daily practice improves the evaluation of patients with SpA as well.
At this point we would like to comment on the management of patient's emotional/psychological status. The published recommendations propose several actions in daily to improve the negative impact of the disease, for example, with the use of the motivational interview, practising empathy, providing adapted information, positive and constructive messages, etc. This strategies reduce anxiety and improve patients well-being. Rheumatologists and gastroenterologists, but also other health professionals like nurses are already prepared to follow these actions or just require simple training to acquire these skills. However, the evaluation and management of mental diseases like depression should always be performed by a mental health professional (psychologist, psychiatrist). Rheumatologists and gastroenterologists are responsible of the screening of these group of diseases for example using the HADS questionnaire, and if one of them is suspected then the patients should be referred to a mental health professional.
Finally, the experts consider very relevant to point out that implementation also requires participation and interaction of multiple actors, organisations and care levels, scientific societies and/or working groups or patients associations.
On the other hand, our study is qualitative in nature, and not free of the limitations inherent to this type of design and these should be addressed. We include a narrative review of the literature, which was not systematic, and therefore cannot rule out it having missed some key studies. Regarding the survey, the sample size was quite small and might lack representativeness, but the results regarding the poor knowledge and implementation of the recommendations are very consistent. We also recognise a potential selection bias of respondents, given that it was sent to health professionals with a special interest in SpA, and as a result, they may have been more aware (than other colleagues) of the existence of recommendations on the psychological management of patients, more sensitive to the issue, and therefore, more likely to follow the recommendations made. Such bias may also have been present among the experts participating in the nominal group. It is possible that the expert's clinical practice differs from that of colleagues who are less experienced in this group of diseases. But taking into account our results we would expect even worse results if we have analysed a more representative sample.
Nonetheless, despite these limitations, we believe that this qualitative study may serve as a useful starting point for increasing the uptake of the recommendations in routine practice. More efforts are needed in the implementation field to achieve changes in clinical practice that would eventually improve the management of the psychological problems and needs of patients with SpA and IBD.
Authors’ contributionsEstíbaliz Loza and Ana Urruticoechea contributed in a similar and full way in the design of the study, analysis and interpretation of the data, critically reviewed the article and approved the version for publication. Jesús Sanz, Daniel Ginard, Yago González-Lama, Xavier Juanola, Miriam Almirall, Natalia Borruel, and Jordi Gratacós participated in the analysis and interpretation of the data, critically reviewed the article, and approved the version for publication.
FinancingThis work was independent.
Conflicts of interestThe authors report having no conflicts of interest.
We would like to thank the survey participants in the survey.