Sarcoidosis is a Th1-mediated chronic inflammatory disease characterized by non-caseating granulomas. Its pathogenesis is not yet clear, but the possible role of various proinflammatory cytokines is being discussed.
AimThis study aims to determine serum cytokine (IL-6, IL-12, IL-17, and IL-23) levels in patients with sarcoidosis, and to determine a possible correlation with clinical and laboratory findings of the disease.
Material and methodForty-four biopsy-proven sarcoidosis patients followed up at a single centre and 41 healthy volunteers were included in the study. Demographic, clinical, laboratory, and radiological data of all patients were recorded. Serum samples from the patients and the control group were taken and IL-6, IL-12, IL-17, IL-23 were measured by ELISA method.
ResultsOf the 44 sarcoidosis patients, 13(29.5%) were male and 31(70.5%) were female. Average patient age was 47.4 years, mean disease duration was 3.2 years. Twenty-one (47.7%) patients had erythema nodosum, three (6.8%) had uveitis, 40(90.9%) had arthralgia, 23(52.3%) had ankle arthritis, 15(34.1%) had enthesitis. Laboratory evaluation showed increased serum ACE levels in 24(54.5%) patients, increased serum calcium levels in 11 (25%) patients, increased serum D3 levels in 5(11.4%) patients, increased ESR and CRP levels in 22(50%) and 23(52.3%) patients, respectively. Compared with the control group higher serum IL-23 levels were found in the patients with sarcoidosis (p=.01). Serum IL-23 was associated with ankle arthritis (p=.02). Serum IL-6, IL-12, and IL-17 levels were similar in the sarcoidosis patients and the control group (p=.128, p=.212, p=.521 respectively).
ConclusionIn our study, we found increased serum IL-23 in patients with sarcoidosis, while serum IL-6, IL-12, and IL-17 were detected as normal. Although our results are somewhat contradictory to other studies in the literature, the question should still be whether sarcoidosis is a Th1/Th17 disease. Multicentre studies are needed in this regard.
La sarcoidosis es una enfermedad inflamatoria crónica mediada por Th1, caracterizada por granulomas no caseificantes. Su patogenia no está clara todavía, aunque se está debatiendo el posible rol de las diversas citocinas proinflamatorias.
ObjetivoEl objetivo de este estudio es determinar los niveles de citocinas séricas (IL-6, IL-12, IL-17 e IL-23) en los pacientes con sarcoidosis, así como establecer una posible correlación con los hallazgos clínicos y de laboratorio de la enfermedad.
Material y métodoSe incluyó en el estudio a 44 pacientes con sarcoidosis verificada mediante biopsia, cuyo seguimiento se realizó en un único centro, y 41 voluntarios sanos. Se registraron los datos demográficos, clínicos, de laboratorio y radiológicos de todos los pacientes. Se tomaron muestras séricas de los pacientes y el grupo control, midiéndose los niveles de IL-6, IL-12, IL-17 e IL-23 mediante el método ELISA.
ResultadosDe los 44 pacientes con sarcoidosis, 13 (29,5%) fueron varones y 31 (70,5%) fueron mujeres. La edad media de los pacientes fue de 47,4 años, y la duración media de la enfermedad fue de 3,2 años. Veintiún (47,7%) pacientes tenían eritema nudoso, 3 (6,8%) tenían uveítis, 40 (90,9%) tenían artralgia, 23 (52,3%) tenían artritis de tobillo y 15 (34,1%) tenían entesitis. La evaluación de las pruebas de laboratorio reflejó un incremento de los niveles séricos de ECA en 24 (54,5%) pacientes, de los niveles séricos de calcio en 11 (25%) pacientes, de los niveles séricos de D3 en 5 (11,4%) pacientes y de los niveles de ESR y PCR en 22 (50%) y 23 (52,3%) pacientes, respectivamente. En comparación con el grupo control, se encontraron niveles séricos de IL-23 más elevados en los pacientes con sarcoidosis (p=0,01). Los niveles séricos de IL-23 estuvieron asociados a artritis de tobillo (p=0,02). Los niveles séricos de IL-6, IL-12 e IL-17 fueron similares en los pacientes con sarcoidosis y en los sujetos del grupo control (p=0,128, p=0,212 y p=0,521, respectivamente).
ConclusiónEn nuestro estudio encontramos un incremento de los niveles séricos de IL-23 en los pacientes con sarcoidosis, mientras que se detectaron niveles normales de IL-6, IL-12 e IL-17. Aunque nuestros resultados son ligeramente contradictorios con respecto a otros estudios de la literatura, persistiría la cuestión de si la sarcoidosis es una enfermedad de Th1/Th17. Son necesarios estudios multicéntricos a este respecto.
Sarcoidosis is a chronic inflammatory disease of unknown aetiology characterized with non-caseified granuloma formation.1 It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and the locomotor system.2 The pathogenesis of the disease is not clearly yet. Sarcoidosis is usually accepted as Th1-related disease, developed as results of unknown antigen stimulation, immune system dysregulation and formation of the granuloma.3 Recently the higher amounts of Th17-related cytokines were found in bronchoalveolar lavage(BAL) fluid and the sera in patients with sarcoidosis.4 It may be suspected for the role of this pathway in disease development and progression. Various studies showed the important role of many cytokines in the disease pathogenesis.5,6 Sarcoidosis patients secrete pro-inflammatory cytokines, including interleukin (IL)-12, IL-23, and tumour necrosis factor (TNF)-a. Interleukin-23 is a protein encoded by the IL23A gene in humans and is produced by dendritic cells and macrophages. They share a common subunit p40 with IL-12 and are important proinflammatory cytokines.7 The IL-23 family of cytokines, (IL-12, IL-23, IL-27, and IL-35), have been implicated in other granulomatous inflammatory diseases such as tuberculosis and Crohn's disease, and a role for some of these cytokines has also been proposed in sarcoidosis.8
The aim of this study is to detect serum IL-6, IL-12, IL-17 and IL-23 levels in patients with sarcoidosis and to determine a possible relationship with clinical and laboratory findings of the disease.
Materials and methodsForty-four patients diagnosed with sarcoidosis were consecutively included in the study. Forty-one healthy volunteers compatible with age and gender were included as the control group. The sarcoidosis diagnosis was made with biopsy and histopathological examinations taken from different organs and tissues, and the demonstration of the non-caseified granuloma. Other reasons likely to cause granulomatous illnesses (bacterial, fungal infections) were excluded. The following laboratory tests were conducted on all patients with sarcoidosis: routine biochemistry, acute phase reactants (ESR, CRP), serum ACE, calcium and D3 levels. Lung X-ray and thorax CT imaging were conducted for staging the sarcoidosis. All events were questioned in detail and their systemic and rheumatologic examinations performed. Informed consent was taken from each of the individuals in both groups and entry forms were filled out. Demographic, clinical, serologic and radiological data of the patients group were registered. Blood samples from patients and healthy volunteers taken in tubes and procured by centrifuge for 10min at 4000rpm were preserved in a refrigerator at −80°C until the study. During the study, the serums were transferred into the +4°C part of the refrigerator a day before and kept there to defrost. Before pipetting, the homogenecity of the serums was ensured by vortexing. IL-6, IL-12, IL-17, IL-23 were examined in all patients and the control group by ELISA method.
Statistical analysisAll statistical analyses were made by using SPSS version 9.0 (Chicago, II, USA). Prevalence was calculated for each group and comparisons for categorical variables were made with a Chi-square test. Continuous variables were compared with Student's t-test. Descriptive statistics for continuous variables are presented either by the mean and standard deviation (SD) or median and interquartile range, where appropriate, categorical variables as frequency (and percentage). For all statistical tests, a p value of <0.05 was considered to be statistically significant.
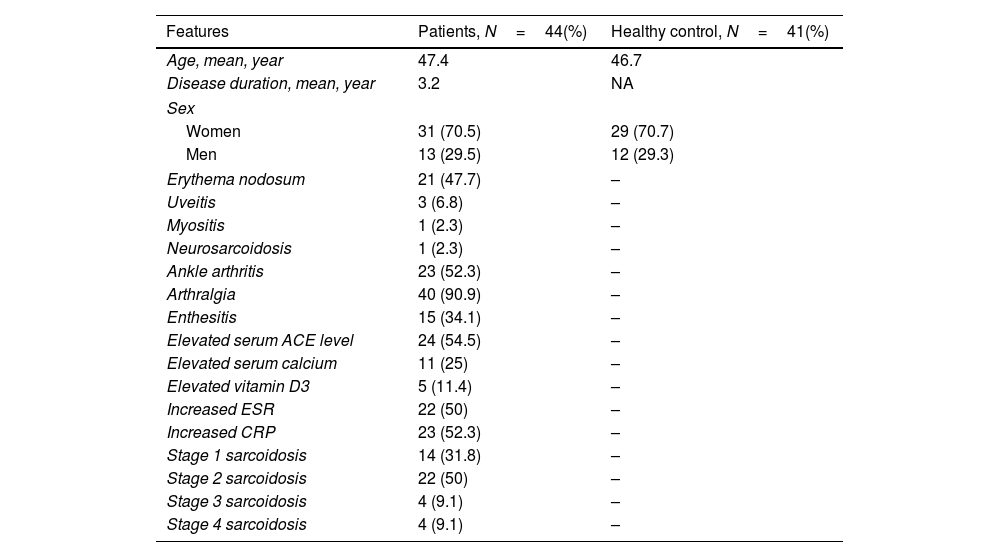
ResultsThirteen (29.5%) of the forty-four patients with sarcoidosis were male and 31 (70.5%) were female. The average patient's age were 47.4 years, the average disease duration were 3.2 years. Erythema nodosum was found in 21 (47.7%) of patients with 44 sarcoidosis, uveitis in 3 (6.8%), arthralgia in 40 (90.9%), arthritis in ankle in 23 (52.3%), and enthesitis in 15 (34.1%). In laboratory evaluation, serum ACE elevation was detected in 24 (54.5%) patients, serum calcium level in 11 (25%) patients, serum D3 elevation in 5 (11.4%) patients, elevated ESR in 22 (50%) patients, and CRP elevation in 23 (52.3%) patients (Table 1). Patients with sarcoidosis had higher serum IL-23 level compared to the control group (p=0.01)(Table 2). There was a relationship between serum IL-23 and ankle arthritis (p=0.02). There were no association between the serum IL-23 level and clinical symptoms such as enthesitis, sacroiliitis, and arthralgia (p=0.18, p=0.45, p=0.12 respectively) (Table 3). Serum IL-6, IL-12 and IL-17 levels were similar with sarcoidosis patients and the control group (p=0.128, p=0.212, p=0.521 respectively). There was no detected any correlation between serum cytokines level and stage of disease.
Demographic, clinical and laboratory features of patients with sarcoidosis and healthy control group.
| Features | Patients, N=44(%) | Healthy control, N=41(%) |
|---|---|---|
| Age, mean, year | 47.4 | 46.7 |
| Disease duration, mean, year | 3.2 | NA |
| Sex | ||
| Women | 31 (70.5) | 29 (70.7) |
| Men | 13 (29.5) | 12 (29.3) |
| Erythema nodosum | 21 (47.7) | – |
| Uveitis | 3 (6.8) | – |
| Myositis | 1 (2.3) | – |
| Neurosarcoidosis | 1 (2.3) | – |
| Ankle arthritis | 23 (52.3) | – |
| Arthralgia | 40 (90.9) | – |
| Enthesitis | 15 (34.1) | – |
| Elevated serum ACE level | 24 (54.5) | – |
| Elevated serum calcium | 11 (25) | – |
| Elevated vitamin D3 | 5 (11.4) | – |
| Increased ESR | 22 (50) | – |
| Increased CRP | 23 (52.3) | – |
| Stage 1 sarcoidosis | 14 (31.8) | – |
| Stage 2 sarcoidosis | 22 (50) | – |
| Stage 3 sarcoidosis | 4 (9.1) | – |
| Stage 4 sarcoidosis | 4 (9.1) | – |
Abbreviations: ACE: angiotensin converting enzyme; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein.
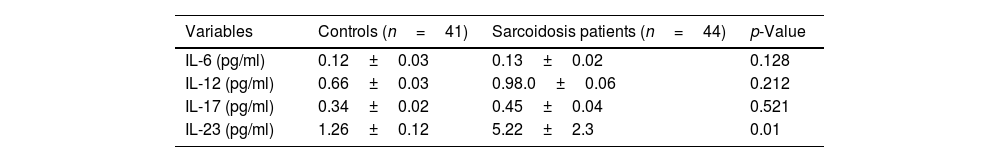
Mean serum IL-6, IL-12, IL-17 and IL-23 levels in patients with sarcoidosis and control group.
| Variables | Controls (n=41) | Sarcoidosis patients (n=44) | p-Value |
|---|---|---|---|
| IL-6 (pg/ml) | 0.12±0.03 | 0.13±0.02 | 0.128 |
| IL-12 (pg/ml) | 0.66±0.03 | 0.98.0±0.06 | 0.212 |
| IL-17 (pg/ml) | 0.34±0.02 | 0.45±0.04 | 0.521 |
| IL-23 (pg/ml) | 1.26±0.12 | 5.22±2.3 | 0.01 |
* p<0.05 statistically significant.
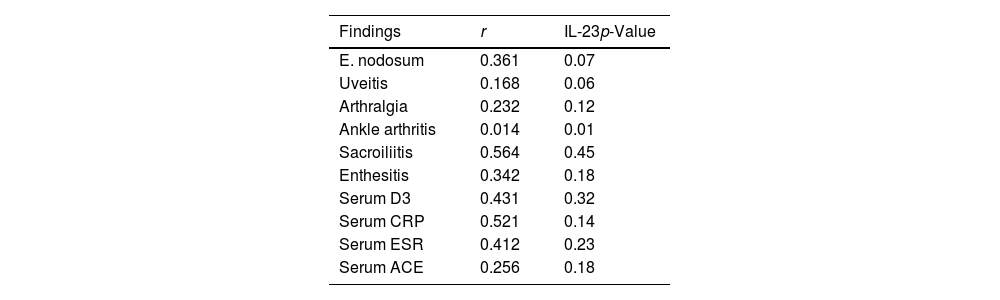
Correlation between serum IL-23 with clinical findings in patients with sarcoidosis.
| Findings | r | IL-23p-Value |
|---|---|---|
| E. nodosum | 0.361 | 0.07 |
| Uveitis | 0.168 | 0.06 |
| Arthralgia | 0.232 | 0.12 |
| Ankle arthritis | 0.014 | 0.01 |
| Sacroiliitis | 0.564 | 0.45 |
| Enthesitis | 0.342 | 0.18 |
| Serum D3 | 0.431 | 0.32 |
| Serum CRP | 0.521 | 0.14 |
| Serum ESR | 0.412 | 0.23 |
| Serum ACE | 0.256 | 0.18 |
* p<0.05 statistically significant.
Our study results showed that patients with sarcoidosis had higher serum IL-23 level compared to the control group whereas the serum IL-6, IL-12 and IL-17 levels were similar between both groups. The close relationship between serum IL-23 and ankle arthritis was found whereas no association between the serum IL-23 level and clinical symptoms such as enthesitis, sacroiliitis, and arthralgia were detected. Sarcoidosis is a multisystemic granulomatous disease of unknown cause. It is predominantly Th-1 disease, but also a broad spectrum of various cytokines have role in the pathogenesis of sarcoidosis.9 Th17 pathway in which IL-23 is a key cytokine were also investigated in disease development. While IL-12 is linked to sarcoidosis, the role of IL-23 and IL-17 has not been examined well yet. It is known that IL-23 and TGF-beta play an important role in the proliferation and differentiation of Th17 cells, which produce IL-17A, IL-17F, IL-21, and IL-22.10 Gene analyses showed close relationship between IL-23 receptor polymorphisms and clinical findings in patients with sarcoidosis. Kim et al. reported the association of IL23R polymorphism and sarcoid uveitis.11 IL23R may be a common susceptibility gene shared by various autoimmune disorders including inflammatory bowel disease, psoriasis, and sarcoid uveitis.12 The survival, expansion and activation of Th17 cells, which have recently been linked to sarcoid granuloma formation may be promoting by IL-23.13 However IL-23 receptor mRNA is found to be elevated in the sarcoid granulomatous skin lesions as resulting in up-regulation of IL-23 p19 in two-thirds of skin lesions.14 Peripheral mononuclear cells of sarcoidosis patients produce less IL-23 than control group, showing that IL-23 might play a role in the formation of granulomas but not in peripheral blood.15 IL-23 mostly acts as pro-inflammatory cytokine through the promotion of Th17 development, this fact may underline the possible role of Th17 cells in sarcoidosis.16 It have been reported that the Th17 cytokine IL-17A have important role in formation of granuloma following infection with mycobacteria.17 Contrary to our results, Th17 cells were detected both in the peripheral blood and in the BAL fluid of patients with active sarcoidosis.18 In our study, among the reasons we found IL-17 to be normal, it may be that there was no active disease or not using a more sensitive kit for detection of IL-17. Since to date there are no murine models of sarcoidosis it is difficult to verify whether Th17/IL-17A contribution is essential in sarcoidosis. The role of IL-12 in sarcoid granuloma formation is well discussed. Multiple studies confirm that IL-12p40 is elevated in blood, BAL fluid, and granulomatous tissue from sarcoidosis patients compared to healthy controls.13 The corresponding IL-12 receptor chain IL-12Rβ1 is equally over-expressed in peripheral blood and BAL of sarcoidosis patients.19 IL-12 is known to increase IFNγ production and this holds true in sarcoid patients compared to controls.20 Hata et al. showed that circulating IL-12 p40 was highly increased in sarcoidosis patients and this was correlated with the number of involved organs.21 The authors suggested that increased circulating IL-12 p40 is an important systemic marker for disease activity. Shigehara et al. found that the serum concentrations of IL-12 p40 and interferon gama(IFNg) in pulmonary sarcoidosis were significantly higher compared with the normal controls.22 The authors speculated that this may explain the Th1 response in sarcoidosis and may a useful clinical marker for disease activity. IL-12, in particular, may have a role in the dysregulation of IFN-gama which was demonstrated in sarcoidosis. Probably, these mediators including IL-12 are not indispensable in interferon synthesis and production or formation of sarcoid granuloma. This fact may explain to some extent why ustekinumab which blocks both IL-12 and IL-23 has not any efficacy in patients with sarcoidosis.23
Our study had some limitations. The small number of patients including in the study, the fact that the many of patients received immunosuppressive therapies at the time of cytokine measurement are two important limitations of our study. This, together with the significant inter-individual variation of cytokine levels may explain some findings that are contradictory to other reports.
ConclusionThe IL-23 family of cytokines have been implicated in the pathogenesis of various granulomatous inflammatory diseases such as tuberculosis and Crohn's disease. The role of these cytokines has also been proposed in sarcoidosis pathogenesis. Our study results showed increased serum IL-23, while serum IL-6, IL-12 and IL-17 were detected as normal. Despite our results are somewhat contradictory to other studies in literature, sarcoidosis should be discussed if is the Th1/Th17 disease or not. More studies are needed to shed light on this issue.
FundingThe authors declared not any financial support.
Conflicts of interestThe authors declared not any conflicts of interest.