Granulomatosis with polyangiitis (Wegener) (GPA) was diagnosed in a 44 year-old-man who had a relapse 6 years after diagnosis with the “air crescent” sign on chest CT. Seven years after his diagnosis the patient presented a new relapse with cavitary lung disease, and high levels of anti-proteinase 3 antibodies, suggesting disease activity; however, a transbronchial biopsy showed histological findings of tuberculosis (TB). The association between TB and GPA is rarely informed; moreover TB and GPA have similar findings including both clinical and anti-proteinase 3 antibodies.
Paciente masculino de 44 años, con diagnóstico de granulomatosis con poliangeítis (Wegener) (GPA) y recaída 6 años después, con el signo de la media luna creciente en la tomografía. Siete años después del diagnóstico, el paciente presentó otro episodio con empeoramiento de la enfermedad cavitaria pulmonar y altos niveles de anticuerpos antiproteinasa 3, lo que sugirió actividad de la enfermedad; adicionalmente, la biopsia transbronquial informó tuberculosis pulmonar (Tb). La asociación entre Tb y GPA es rara, aunque estas 2 enfermedades tienen características clínicas similares y se acompañan de anticuerpos antiproteinasa 3 que se han asociado a tratamiento antifímico.
The association of pulmonary tuberculosis granulomas with polyangiitis (Wegener) (GPA) is rare. Both diseases have similar clinical features including cavitary lung disease. We describe the case of a patient with clinical features and laboratory and imaging findings common in both diseases, something which represents a challenge for diagnosis and treatment.
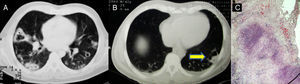
Case ReportMale patient, 44 years, with GPA diagnosed in April 2003 due to weight loss, cough, recurrent episodes of nodular scleritis, mononeuritis multiplex and cavitary nodules in a chest CT (Fig. 1A); he also presented proteinuria (50mg/dl), and dysmorphic microhematuria with positive neutrophil cytoplasmic antibodies (cANCA). He received glucocorticoids and 7 cycles of IV cyclophosphamide, with methotrexate as maintenance therapy.
In July 2009 he relapsed, presenting productive cough without hemoptysis, mononeuritis multiplex, proteinuria (50mg/dl), dysmorphic hematuria and elevated CRP (16.7mg/dl). Chest CT showed a suggestive image with a crescent sign (Fig. 1B), characteristic of aspergiloma.1 To exclude infection, we performed a biopsy of the lesion, which reported granulomas (disease activity). Cultures and stains for mycobacteria and fungal infections ruled them out (Fig. 1C). Again, he received cyclophosphamide (7 cycles), methylprednisolone, and azathioprine for maintenance.
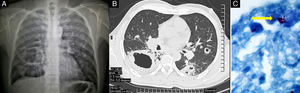
In October 2010, the patient required hospitalization due to weight loss and a 4 week history of cough and hemoptysis, presenting leukocytosis (11×103μl−1), anemia (11.8g/dl), thrombocytosis (603×103μl−1), high titers of antibodies to proteinase 3 (130.7U/ml) and elevated C-reactive protein (11.74mg/dl). The radiograph showed multiple bilateral nodules, some cavitated, and a large cavitation in the right lower lobe (Fig. 2A); a CT scan confirmed the findings, showing cavitations with thick walls (more than 5mm) and increased irregularity (Fig. 2B). PPD testing was negative. A bronchoscopy with biopsy was performed, showing the presence of acid-fast resistant bacilli (Fig. 2C); a polymerase chain reaction reported Mycobacterium tuberculosis complex.
DiscussionThe differential diagnosis of cavitary lung disease in this patient with immunosuppressive therapy included both disease activity and an infectious process as well as, ultimately, cancer. The high titers of anti-proteinase 3 antibodies and the presence of nodules are related to disease activity.2 Among the factors associated with severe infections is the use of cyclophosphamide and glucocorticoids, essential for the management of GPA.3 In developing countries, infectious disease due to cavitary pulmonary tuberculosis is very common and has clinical and radiological features similar to GPA.4,5 Additionally, there are reports that highlight the presence of cANCA in 40% of patients with tuberculosis,6–8 however, positive proteinase 3 antibodies may be due to treatment for tuberculosis, as pointed out by Esquivel-Valerio et al.9 Because our patient had not received TB treatment, the context suggested GPA activity. On the other hand, the biopsy diagnosed pulmonary tuberculosis.
ConclusionsGPA and pulmonary tuberculosis have similar clinical characteristics. On the one hand, pulmonary involvement with cavitation, hemoptysis, fever and weight loss, and on the other hand, patients on TB treatment may have antiproteinase 3 antibody positivity. There are a few reported cases of the association of GPA and tuberculosis.10 Our patient is of interest since the first biopsy ruled out the diagnosis of infectious disease and the second confirmed the presence of tuberculosis; in addition, the patient had high levels of antibodies to proteinase 3, which also suggest disease activity. We emphasize the obligation to look for infection in patients with rheumatic diseases receiving immunosuppressive therapy, even when clinical and paraclinical features are suggestive of disease activity.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Martínez-Martínez MU, et al. Paciente masculino de 44 años con enfermedad cavitaria pulmonar. Reumatol Clin. 2013;9:62–64.