Up to 30% of patients with psoriasis develop joint disease, the course of which can be improved by early diagnosis and treatment. The aim of this study was to describe our experience with a new multidisciplinary psoriasis and psoriatic arthritis unit over a period of 4 years (2009–2012).
Material and methodsImplementation of a PSOriasis Rheumatology and Dermatology unit (PSORD) to provide patient care and physician training. In the first phase of the project, referral criteria for the unit were defined and several meetings were organized to train and prepare the specialists involved in the program. In the second phase, a schedule was drawn up for monthly patient visits with the PSORD team. Starting in 2011, training was offered to dermatologists and rheumatologists from other hospitals interested in implementing a similar model.
ResultsA total of 259 visits (71% first visits, 8% no-shows) were scheduled during the period analyzed, with a median of 8 visits (range, 2–14 visits) per session. Sixty-three percent of the patients were referred from the rheumatology department. Diagnosis and treatment were modified in 32% and 47% of cases, respectively. Three training courses were held with 15 physicians from 6 hospitals, 3 of which created similar units.
ConclusionsThe PSORD model improved the management of difficult-to-diagnose and/or uncontrolled disease, the early diagnosis and treatment of psoriatic arthritis, and collaboration between dermatologists and rheumatologists. Finally, the model lends itself to being exported to other settings.
La afectación articular en los pacientes con psoriasis puede llegar hasta el 30%. El diagnóstico y tratamiento precoz de la artropatía puede influenciar su evolución. El objetivo de nuestro trabajo es describir la experiencia de la unidad multidisciplinar de psoriasis y artritis psoriásica de nuestro hospital en el periodo 2009–2012.
Material y métodosElaboración de un programa asistencial y docente. En una primera fase se consensuaron los criterios de derivación a la futura unidad y se realizaron varias reuniones conjuntas para formar y concienciar a los especialistas. En una segunda fase se estableció una agenda de visitas conjunta psoriasis-reumato-dermato (PSORD) con periodicidad mensual. A partir de 2011 se desarrolló un programa formativo abierto a dermatólogos y reumatólogos interesados en crear un modelo de colaboración similar.
ResultadosDurante el periodo revisado se han efectuado 259 visitas (71% primeras, 8% no presentados) con una media de 8 (2–14) visitas por sesión. El 63% de visitas eran derivaciones de reumatología. En un 32% de casos hubo algún cambio en el diagnóstico y en un 47% cambios en el tratamiento. También se han hecho 3 cursos con participación de 15 médicos de 6 hospitales, y en 3 de ellos se han creado unidades parecidas.
ConclusionesEste modelo ha comportado una mejora en el manejo de los pacientes que presentan problemas diagnósticos y/o de control de la enfermedad. También ha aumentado el diagnóstico precoz de la artritis y ha permitido indicar un tratamiento precoz. Además ha aumentado la colaboración entre ambas especialidades y el modelo creado se ha podido exportar a otros hospitales.
The current concept of psoriasis is a systemic disease with multiorgan involvement, including the skin and musculoskeletal system, and often is associated with various comorbidities.1–6 In most cases (70%–80%) skin lesions precede articular involvement by years, and therefore dermatologists play a key role in early detection.7 Psoriatic arthritis (PsA) is a chronic, progressive disease that can be debilitating and affect, according to the series, 30% of patients with psoriasis.8 In the initial stages of PsA, it can be difficult to diagnose, even for rheumatologists, but particularly if there is no suspicion or the characteristics of the entity are not known. Early diagnosis and treatment are essential to prevent future joint damage and disability. Early diagnosis prevents unnecessary tests, avoids treatment associated risk, lowers cost, reduces pain and thereby improves the quality of life of patients.8,9 It is estimated that between 10% and 29% of patients with psoriasis visited dermatology clinics could suffer PsA, and this is not suspected by the dermatologist, which can lead to a delay in diagnosis.10,11 Moreover, it is common in rheumatology to find little or no attention paid to the patient's skin involvement, although this may have an impact on the physical and mental health of the patient, especially if establishing a treatment.
This broader and more complex view of the disease has progressively pushed to increase collaboration among leading specialists involved in the diagnosis and treatment of these patients. The recommendations of the European League Against Rheumatism (EULAR) 201212 suggest a multidisciplinary approach and, in this line, since mid-2009 rheumatology (RMT) and dermatology (DRM) specialists of Parc Taulí University Hospital at Sabadell decided to create a model of multidisciplinary collaboration, as a unit, to improve the management of patients with psoriasis and PsA.
Material and MethodsIn 2009 the Parc de Sabadell Taulí University Hospital created a multidisciplinary unit called Derma Psoriasis Rheumatism (PSORD) for the overall management of patients with psoriatic disease.
Its specific objectives were: (1) to facilitate the early diagnosis of PsA in patients with psoriasis, (2) improve the management of problem patients with psoriasis and PsA, and 3) foster collaboration between the two specialties in our hospital.
Prior to the creation of this unit, the requirement was to have both services with specialists, expertise and interest in psoriatic disease, and to stimulate the diagnostic suspicion and referral to rheumatology by dermatologists.
For data collection a database was designed which collected data of the disease and treatment of patients, and the name of the doctor who derived them and why. The partial analysis of this database is the results presented in this paper.
Assistance ProgramThe assistance program was developed in two stages. The aim of the first stage was to train rheumatologists and dermatologists in the global vision of psoriatic disease, encouraging the need for collaborative work between the two specialties. Project managers, a rheumatologist and a dermatologist, were designated to this end, and conducted, over 3 months, 2 joint training sessions attended by all members of both services. In these training sessions, the disease was described from the point of view of both groups, with particular emphasis on those signs or symptoms suggestive of psoriasis and PsA. As a result of these training sessions, referral criteria were agreed upon by the dermatology and rheumatology multidisciplinary unit (Table 1). The referral criteria were established to visit and control, not all patients with psoriasis and/or PsA, but only those with a diagnostic or therapeutic problem that was the main objective of this project. In a second phase, a joint agenda of 3h visits on a monthly basis was developed. All patients referred to the multidisciplinary unit were visited jointly by a rheumatologist and a dermatologist, making diagnostic and/or therapeutic decisions. The diagnosis of PsA was established at the discretion of the rheumatologist following CASPAR diagnostic criteria.13 The diagnosis of psoriasis was established according to the characteristic signs and, in all cases, at the discretion of the dermatologist proceeding, when in doubt, to request additional diagnostic examinations (biopsy, culture, etc.). The visits were conducted in the rheumatology department using its infrastructure (clinics and specialized nursing staff). Once the patient had been seen in the multidisciplinary unit and the problem reported had been solved, the patient was returned to the reference specialist for routine monitoring.
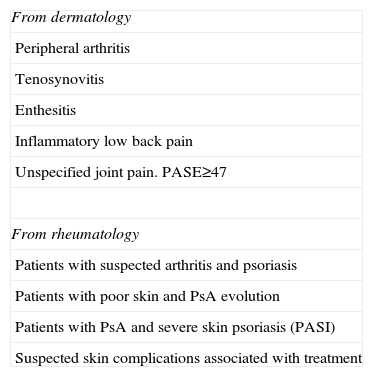
Criteria for Referral of Patients to the Derma Psoriasis Rheumatism (PSORD) Multidisciplinary Unit as per Service of Origin.
| From dermatology |
| Peripheral arthritis |
| Tenosynovitis |
| Enthesitis |
| Inflammatory low back pain |
| Unspecified joint pain. PASE≥47 |
| From rheumatology |
| Patients with suspected arthritis and psoriasis |
| Patients with poor skin and PsA evolution |
| Patients with PsA and severe skin psoriasis (PASI) |
| Suspected skin complications associated with treatment |
The result of the experience gained was used, as of 2011, to develop an accredited training program, and the unit was opened to other peers interested in creating such a unit at their hospitals in a similar collaborative model between rheumatologists and dermatologists. The program consists of a theoretical part, lasting 6h, on the main aspects of psoriasis and PsA reviewed from the perspective of dermatologist and rheumatologist, and development of referral criteria and logistics structure necessary for the creation of a multidisciplinary unit. The program is completed with a practical part the next morning during a routine clinic visit to the PSORD multidisciplinary unit.
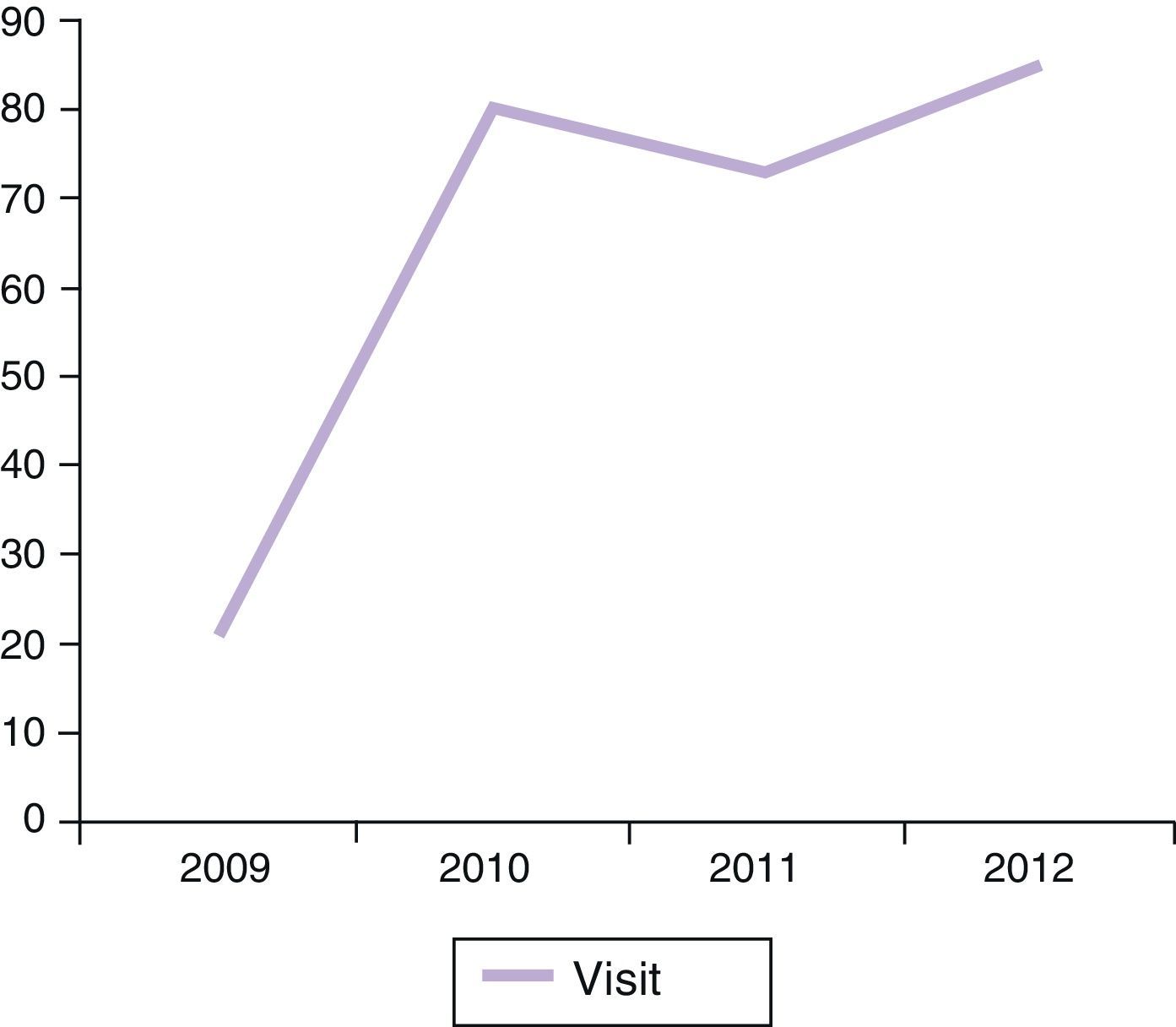
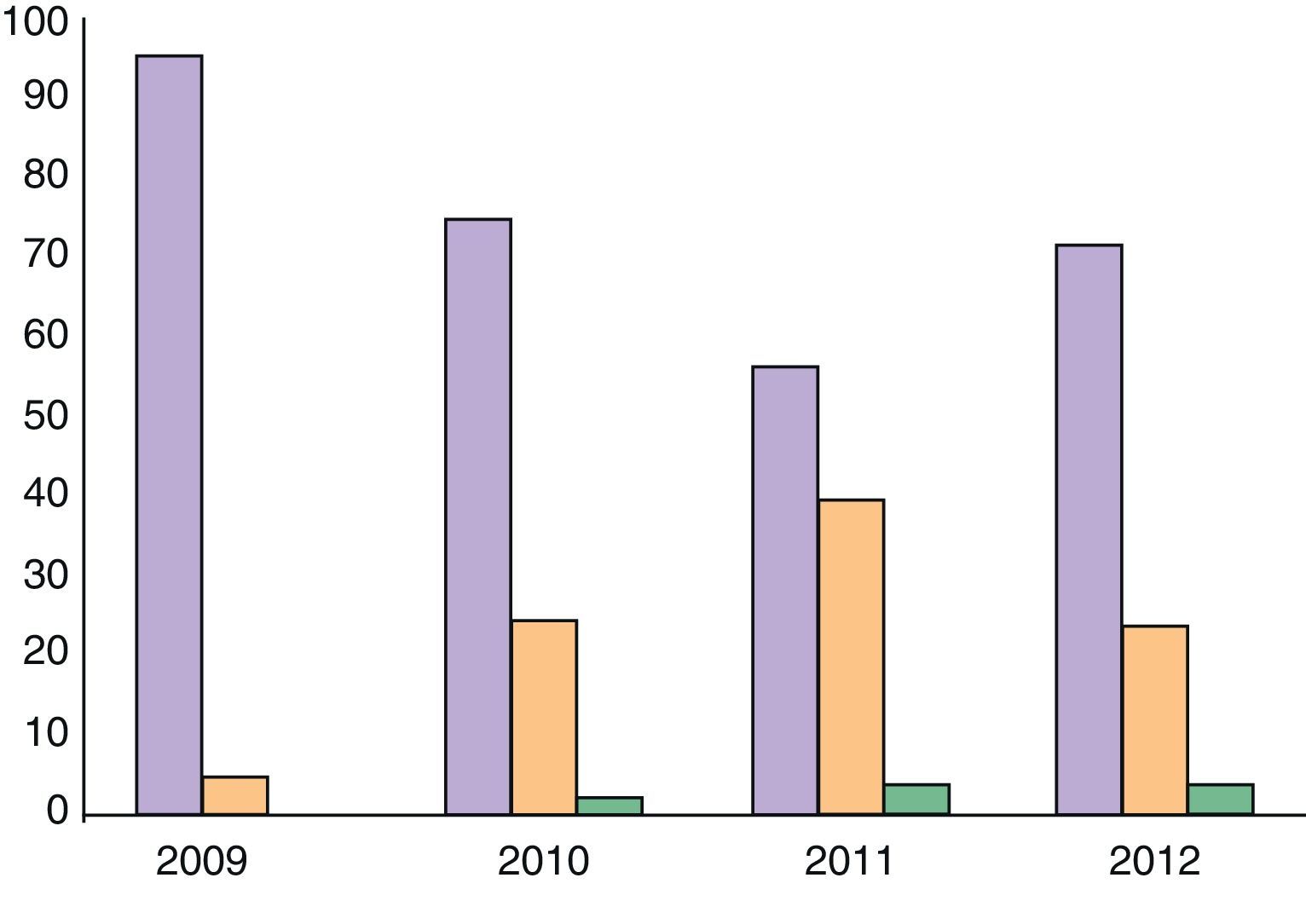
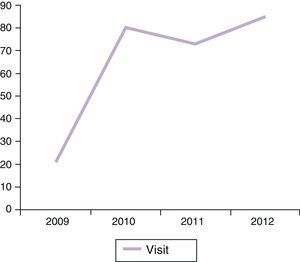
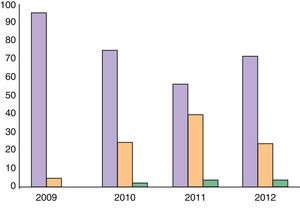
ResultsOver a period of 4 years (2009–2012) 184 patients (89 men and 95 women) have been seen, and have generated 259 visits. All patients seen as per protocol were from rheumatology or dermatology. The number of visits per session had a mean of 8 (2–14). 71% of all visits were first visits, 21% consecutive (of which less than 5% were a third visit). The rate of patients who did not attend the appointment was 8%. Visits increased very significantly between 2009 and 2010 and then stabilized at around 80 visits per year (Fig. 1). Although obviously sequential visits increased over time, first/sequential visit ratio stabilized around 7:3 (Fig. 2).
Patients referred from RMT were 114 cases (63%) versus 68 (37%) from DRM, a proportion of referrals that remained stable throughout the study period.
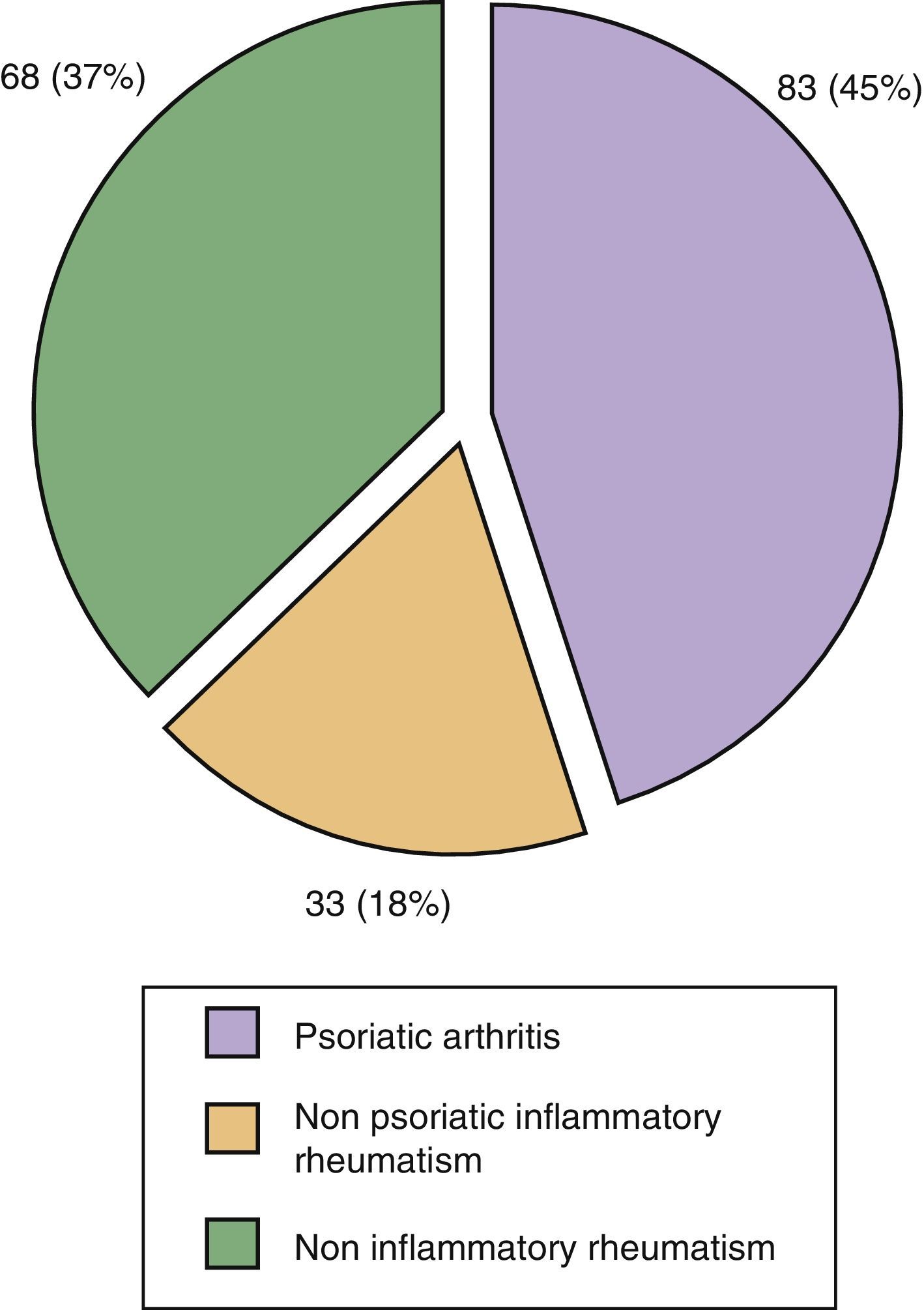
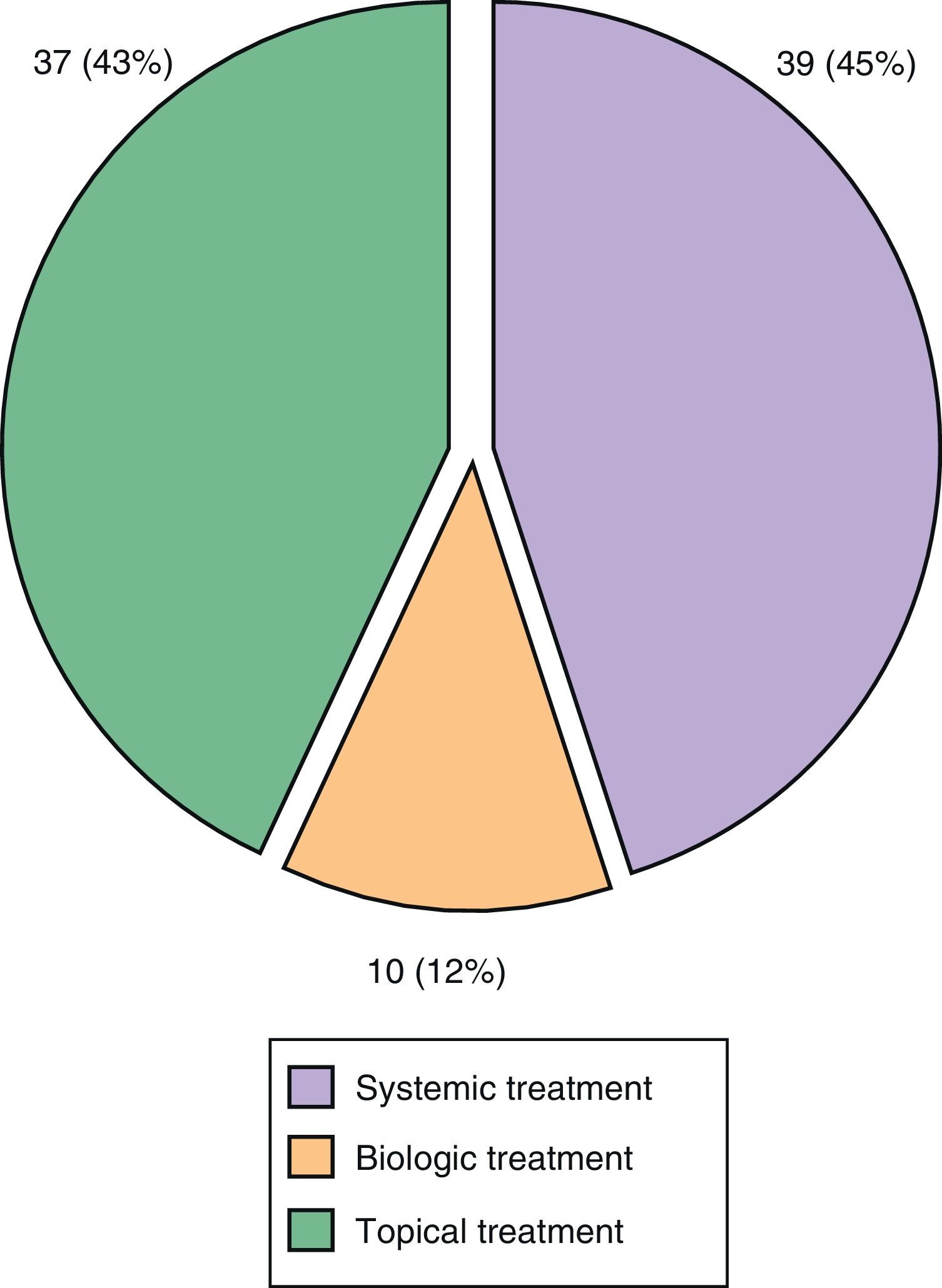
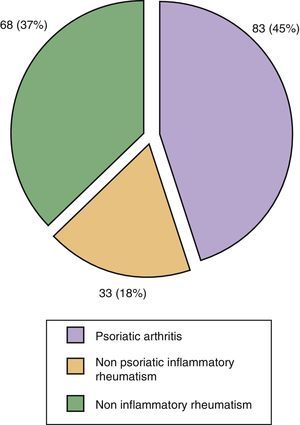
72% (132/184) of all patients referred to the unit had some sort of skin-nail psoriasis. The definitive diagnosis of PsA was established in 45% of referred patients (83/184); of these, 83 patients with PsA in 44 cases (24% of all patients seen) had a de novo diagnosis of PsA. In 18% of cases patients were diagnosed with non-psoriatic inflammatory rheumatism (gout, rheumatoid arthritis and connective tissue disease), and 37% had non-inflammatory musculoskeletal disease (osteoarthritis and nonspecific musculoskeletal pain) (Fig. 3).
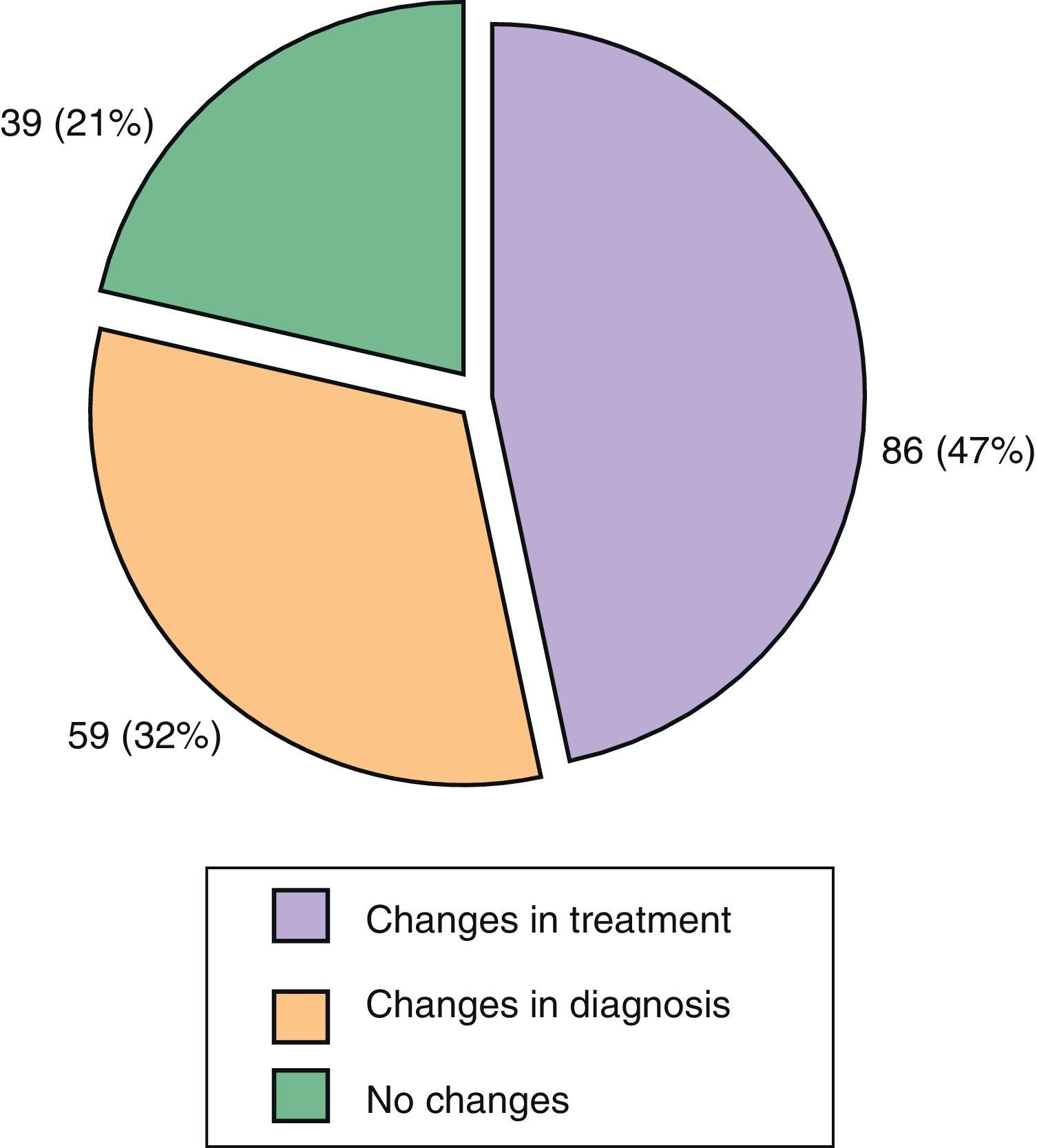
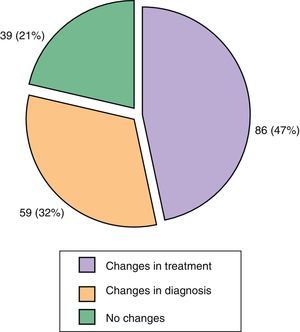
The reason for referral was, on 106 occasions (59%), suspected PsA, which was confirmed in 66% of cases. Moreover, 41% of referrals were due to a therapeutic problem. Diagnosis change occurred in 32% of cases, in 47% of occasions this led somehow to a modified treatment and in 39 cases (21%) no changes were made (Fig. 4). The diagnostic agreement was 40% both for suspected PsA by dermatology as for skin psoriasis and/or nail changes seen by rheumatology. It is important to note the low agreement when suspicion of psoriasis was based by rheumatology on nail lesions (<20%) and when the PsA suspicion was based, by dermatology, on joint and musculoskeletal pain (25%). In these cases the percentage of patients in which the referral was based on the result of the PASE was less than 5%.
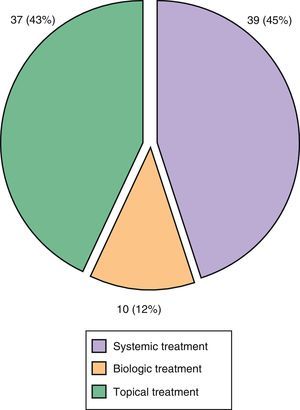
Of the 86 lesions that led to a therapeutic change, 45% of cases entailed changes in systemic therapy and in 30% of cases involved the addition of a new disease-modifying antirheumatic drug (DMARD), methotrexate being by far the most commonly used DMARD. Finally, in 12% of cases a new biologic drug was changed or added (Fig. 5).
Results of the Learning-Teaching ProgramDuring 2011 and 2012 there have been two courses involving 10 rheumatologists from 5 hospitals in our country. So far in 2 of these centers, the Ibiza Can Mises Hospital and Hospital de Basurto in Bilbao, multidisciplinary units similar to ours have been created.
DiscussionWe present the experience of multidisciplinary unit psoriasis at Taulí Parc de Sabadell (PSORD) during the period 2009–2012, a care model in which the patient is visited jointly by a rheumatologist and a dermatologist. This model has an important role in the management of patients with psoriasis who have diagnostic or therapeutic problems whose improvement may be facilitated by early diagnosis of PsA, with the advantages that this may involve the control of the disease and also has allowed a teacher-training program that has resulted in the creation of 2 similar units in other hospitals, and improved collaboration by dermatology–rheumatology, which is expected to generate future collaborative research projects.
It is a pioneering experience in our country that follows the current EULAR guidelines.14 There is only one prior joint communication between rheumatologists and dermatologists by the Center for Skin and Related Musculoskeletal Disease (SARM) at Harvard.15 These authors reported a preliminary study in 2007, with 94 patients seen at the unit during the period of one year,16 although it was not until 2012 when a retrospective review of 510 patients evaluated over a period of 6 years was performed.17 In addition, other formally structured initiatives similar to ours, such as the group of Drs. Frank Behrens Diamant Thaçi at the Goethe University of Frankfurt (Thaçi D, Behrens F. Psoriatic arthritis: Multidisciplinary units experience. Shedding light on psoriatic arthritis and psoriasis. Rheumathologists and dermatologists: two perspectives. Madrid 1–2 February 2013) exist, although we are not aware if they have published their experience. Structured joint dermatologist-rheumatologist visits, such as SARM and our models, provide unregulated personal contact between rheumatologists and dermatologists and the opportunity to systematize, collect and analyze the activity and, in a special way, to strengthen collaboration between the two specialties with the creation of referral criteria and patient management protocols. In this sense both PSORD and SARM are examples of structured collaboration. However, our model is significantly different from SARM, because while SARM is a comprehensive service with its own management unit, the PSORD model is a joint visit program using the existing resources. We decided to create this model since we saw the creation of a separate service as non-feasible in our public health system.
Unlike SARM, in which patients can be referred from multiple sources (not only dermatology and rheumatology, but also trauma, GPs, etc.) our model does not entail a separate service, and referrals are limited to RMT and DRM. This might seem a priori a weakness of our model but it has the advantage of promoting the implementation of joint training programs and awareness by both services in the early detection of complications, including the suspected diagnosis of PsA by dermatologists, something of particular interest, because in 75% of cases, psoriasis precedes the appearance of arthritis. Furthermore, and since there is no correlation between the severity of psoriasis and the presence of arthritis or any PsA specific diagnostic test, diagnostic suspicion by dermatology is difficult.18,19 For this reason we believe it is very important that dermatologists with expertise and special dedication to psoriatic disease participate in joint training programs designed to encourage recognition of the symptoms and signs and a greater suspicion of the diagnosis of PsA. However, the percentage of patients in our series derived from DRM (37%) was lower than expected and reported in other series15 and unfortunately has not increased with the operation time of the unit. Although there is no clear explanation for this fact, it is well known that it is far easier to refer a patient with arthritis (RMT) and skin lesions and suspected PsA in a patient with cutaneous PSO, which explain in part the result. This finding supports the need to periodically sensitize dermatologists on the suspicion and periodic search of PsA in patients with psoriasis at educational meetings.
It is also important in these joint meetings to establish agreed criteria for referral, both from DRM and RMT, to improve the performance of the unit, although we realize, based on our experience, that the diagnostic agreement in our model was only moderate (40%), with an excess of referrals from dermatology for nonspecific musculoskeletal pain and the diagnostic concordance was low (25%). Several validated screening surveys (PASE, PEST, TOPAS) improve performance in these referral situations20,21 although recently its use in clinical practice has proved to be less effective than that assumed in previous studies.22 In our model, and although PASE was advised for use as a screening test in one of the criteria for referral (joint pain), this was not mandatory, which led it to be used in less than 5% of cases depending on the interest of each clinician. In view of the results, compulsory implementation may in certain circumstances (suspected PsA based on joint pain) be of interest. Concerning referrals made from rheumatology, one of the main problems is the suspected diagnosis of PsA based on nail lesions; this segment had less than a quarter of diagnoses successes. This finding is not surprising, because nail disease is one of the biggest challenges for the dermatologist and, because although there is a precise description of the nail lesions that should allow the diagnosis of psoriatic onychopathy, the lack of specificity of these becomes a real diagnostic challenge and one of the most interesting fields of study developed jointly by both specialties.23,24
The number of first visits to our model, which also remained stable throughout the study period, is much higher than that published by the Harvard group. Moreover, unlike this group, all patients referred to our unit, once the problem was solved, returned to their specialist to continue with their usual medical monitoring. This joint assistance model is proposed as a support unit to improve problem patient management and not meant to be a parallel service for routine monitoring of patients or monopolize their treatment, which could lead to duplication of visits and conflicts of interest among specialists and result in a lower referral rate, which will undoubtedly entail a lower quality of care for the patient.
The impact of our unity in the management of patients with psoriasis has been very significant, as evidenced by the fact that only 21% of cases referred to our unit did not entail any changes in diagnosis and/or therapeutics. During the monitoring period, the most frequent diagnosis was that of cutaneous psoriasis in 71% of cases, and in 45% of cases a concomitant diagnosis of PsA was also established and, most importantly, over half of PsA diagnosis of these cases has been de novo. This finding is particularly relevant, because it shows that in 44 referred patients, a de novo diagnosis of PsA has been established due to the suspected diagnosis of dermatologist. Since early diagnosis7,18 and the possible influence of treatment in these phases on the progression of the disease25 is one of the main challenges of PsA, the data of newly diagnosed PsA itself justified, in our opinion, the existence of our unit. But it is also noteworthy that 47% of cases referred to our unit implied a therapeutic change. This change in nearly half the cases led to changes in systemic therapy and particularly, in 30% of cases, the addition of new DMARDs, methotrexate being by far the most commonly used one. The most common reason to change the dose and/or add a new drug was concomitant systemic detection of PsA. These data are in line with that previously published by the Harvard group,17 and support the usefulness of these units to improve the management of problem patients with psoriatic disease.
On the use of biological therapy in 12% of cases sent to our unit resulted in a change (addition or substitution) in this therapy. The most common cause of this change was to improve the management of skin and nail lesions, although in 2 cases the presence of a poorly controlled PsA led to the decision to change. Although the percentage seems non-relevant, the data are very significant when you consider that this is not a unit for indication of biological therapy, but a unit to supervise patients with a previous therapeutic indication by a specialist.
The rate of visits missed was 8%, very low figure in our experience and one that may be due to the fact that the waiting time for the visit was less than a month on average; this important data serve to assess the quality of the model especially if it is aimed at problem patients.
In this paper we present the experience of a single center; however, the fact that nearly half of rheumatologists from other centers participating in the teaching program have been able to create similar units in their hospitals, shows that the model may be applicable to different clinical situations. In previous courses only rheumatologists made the visits, and we believe that the experience gained in future editions would be interesting if joint participation by rheumatologists and dermatologists from centers with interest in implementing a similar model is seen. No doubt this will facilitate the development and increase the percentage of sites with potential for implementing this model of care.
Although the PSORD unit was designed as a high-resolution unit to support fellow specialists in the management of problem patients with psoriasis and PsA, the model has greatly improved the collaboration between the two specialties and has allowed the development of several joint projects, with this work being the first component of this collaboration.
A limitation of this study is that it is the experience of a single center, and should be confirmed and compared with other similar centers, although the absence of publications on similar projects has not allowed this.
The low-referral from dermatology could influence a probably less than desirable early diagnosis of PsA. Since one of the main benefits that can result from the creation of the unit was to facilitate the early diagnosis of PsA, we think that the model should be revised to focus more on the dermatologist, increasing training in this group.
Another weakness of our work is that in the activity log of our unit, nonclinical variables, comorbidities, monitoring, treatment and outcome of patients seen are not included. However, the main goal of our unit was to be a unit of high resolution in the management of problem patients for hospitals with high work load, not in a unit or parallel service to visit and follow up of patients with PsA. However, the project has greatly improved the collaboration between the two specialties, created a teaching program and cooperation and led to various scientific projects currently in development. It is not a closed model. On the contrary, this basic model, taking into account the particularities of each school, can develop collaborative models that incorporate varying degrees of monitoring of patients with PsA.
In conclusion, the creation of a multidisciplinary unit composed of expert rheumatologists and dermatologists in the management of psoriasis and PsA is in line with the main guidelines for the management of psoriasis. In our case it has been a support tool for specialists in the care of patients with psoriatic disease who have some kind of diagnosis and/or disease control problem. Finally, the project has involved improving dermatology–rheumatology collaboration and has resulted in the creation of an educational program and the development of joint projects, of which this work is the first example.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that no experiments have been performed on humans or animals.
Data privacy. The authors declare that they have followed the protocols of their workplace on the publication of data from patients and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors state that patient data does not appear in this article.
Conflict of InterestThe authors state that participants have received grants and research-related payments, counseling and training from the following companies: Abbvie, Janssen, Merck, Novartis and Pfizer.
Training courses derived from the project received the cooperation of Pfizer.
Please cite this article as: Luelmo J, Gratacós J, Moreno Martínez-Losa M, Ribera M, Romaní J, Calvet J, et al. Experiencia de 4 años de funcionamiento de una unidad multidisciplinar de psoriasis y artritis psoriásica. Reumatol Clin. 2014;10:141–146.
According to the authors and publishers, this article is published simultaneously and in full in the journal Actas Dermo-Sifiliográficas http://dx.doi.org/10.1016/j.ad.2013.10.009