The causes of mortality among rheumatic diseases vary widely between geographic areas and cannot be generalized, however, they are frequently associated with the aggressiveness of the clinical presentation and the secondary effects of the therapy used. The main purpose of this study was to characterize the causes of death in a group of patients with autoimmune rheumatic disease. For this purpose, a retrospective study was carried out over a period of 10 years (2009–2019), deceased patients were included from a referral centre in Guatemala City, the records were reviewed in search of demographic and clinical variables. In total, 185 deceased patients were identified from 898 admissions during that period, 85.9% were women and the main disease reported was systemic lupus erythematosus in 49.7% of the cases. Among the causes of mortality, infections were reported in 53% and those attributed to disease activity in 15% of cases. The main conclusion is that that most of the deaths were of infectious origin.
Las causas de mortalidad entre las enfermedades reumáticas varían ampliamente entre áreas geográficas, y no puede generalizarse sobre las mismas, sin embargo, frecuentemente se asocian a la agresividad de la presentación clínica y a los efectos secundarios de la terapéutica utilizada. El propósito principal de este estudio fue caracterizar en un grupo de pacientes con enfermedad reumática autoinmune las causas de muerte. Para el efecto se realizó un estudio retrospectivo en un periodo de 10 años (2009 a 2019), se incluyeron pacientes fallecidos en un centro de referencia en la ciudad de Guatemala, y se revisaron los registros en busca de variables demográficas y clínicas. En total fueron identificados 185 pacientes muertos de 898 ingresos durante ese periodo, el 85,9% fueron mujeres y la principal enfermedad reportada fue lupus eritematoso sistémico con el 49,7% de los casos. Dentro de las causas de mortalidad, las infecciones se reportaron en el 53% y las atribuidas a la actividad de la enfermedad en el 15% de los casos. La principal conclusión es el origen infeccioso como la causa más frecuente de muerte.
Autoimmune rheumatic diseases (ARD) have a low prevalence of associated mortality from 0.3 to 2.1 and the associated mortality rates with these conditions have little impact on the general statistics at worldwide level, compared with other diseases of higher prevalence such as high blood pressure or diabetes mellitus.
In general terms, within the group of rheumatic diseases a standardised mortality ratio (SMR) risk of 2.03 (95% CI: 1.79–2.29) has been reported, particularly for those considered as inflammatory. The highest risk reported was 4.80 in systemic vasculitis, followed by 2.9 in systemic lupus erythematosus and 1.44 in rheumatoid arthritis.1
The causes of death are regularly associated with acute events, unrelated to the disease presentation. Frequent mention is made of infections, respiratory and cardiovascular diseases, such as those with the highest risk of this event.1
Other associated reported factors were: age and duration of the disease, the severity of presentation and the adverse effects relating to the treatment administered.2–4
The aim of the study was to describe the frequency and main causes of mortality in patients with autoimmune rheumatic diseases in a central benchmark hospital.
MethodologyA retrospective study was conducted, which included patients who had been referred to a tertiary level healthcare centre in the city of Guatemala, diagnosed with an autoimmune rheumatic disease. The period under review was between 2009 and 2019 and information from the medical files of patients who had died during this period was used. The variables studied contained demographic and clinical data, with emphasis on the cause of death. The following diseases were included using the diagnostic criteria of the American College of Rheumatology (ACR): systemic lupus erythematosus (SLE); rheumatoid arthritis (RA); inflammatory myopathies (IM); systemic vasculitis (SV); antiphospholipid syndrome (APS); systemic sclerosis (SS); mixed connective tissue disease (MCTD), and under the heading “others‿ were rheumatic diseases which had no defined diagnosis according to the ACR.
Statistical analysisStatistical Análisis was performed with the EPI info 7.2.0.1 programme, using one of its databases. The continuous variable results are indicated by means and standard deviations and percentages.
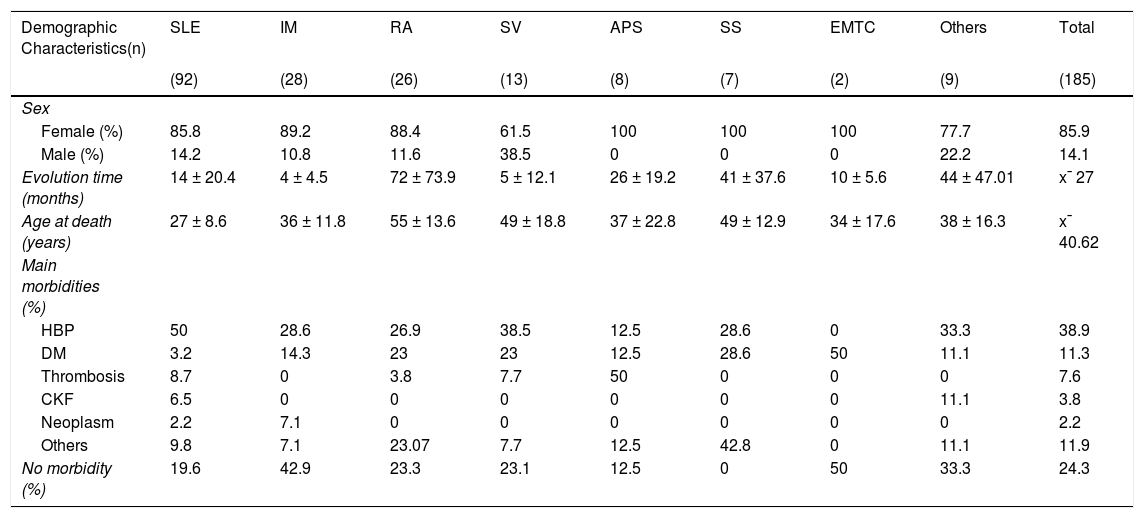
ResultsOf the 898 patients admitted to hospital, 185 deaths were reported. The necessary information and main demographic data obtained are presented in Table 1.
Demographic characteristics distributed by ARD.
| Demographic Characteristics(n) | SLE | IM | RA | SV | APS | SS | EMTC | Others | Total |
|---|---|---|---|---|---|---|---|---|---|
| (92) | (28) | (26) | (13) | (8) | (7) | (2) | (9) | (185) | |
| Sex | |||||||||
| Female (%) | 85.8 | 89.2 | 88.4 | 61.5 | 100 | 100 | 100 | 77.7 | 85.9 |
| Male (%) | 14.2 | 10.8 | 11.6 | 38.5 | 0 | 0 | 0 | 22.2 | 14.1 |
| Evolution time (months) | 14 ± 20.4 | 4 ± 4.5 | 72 ± 73.9 | 5 ± 12.1 | 26 ± 19.2 | 41 ± 37.6 | 10 ± 5.6 | 44 ± 47.01 | x¯ 27 |
| Age at death (years) | 27 ± 8.6 | 36 ± 11.8 | 55 ± 13.6 | 49 ± 18.8 | 37 ± 22.8 | 49 ± 12.9 | 34 ± 17.6 | 38 ± 16.3 | x¯ 40.62 |
| Main morbidities (%) | |||||||||
| HBP | 50 | 28.6 | 26.9 | 38.5 | 12.5 | 28.6 | 0 | 33.3 | 38.9 |
| DM | 3.2 | 14.3 | 23 | 23 | 12.5 | 28.6 | 50 | 11.1 | 11.3 |
| Thrombosis | 8.7 | 0 | 3.8 | 7.7 | 50 | 0 | 0 | 0 | 7.6 |
| CKF | 6.5 | 0 | 0 | 0 | 0 | 0 | 0 | 11.1 | 3.8 |
| Neoplasm | 2.2 | 7.1 | 0 | 0 | 0 | 0 | 0 | 0 | 2.2 |
| Others | 9.8 | 7.1 | 23.07 | 7.7 | 12.5 | 42.8 | 0 | 11.1 | 11.9 |
| No morbidity (%) | 19.6 | 42.9 | 23.3 | 23.1 | 12.5 | 0 | 50 | 33.3 | 24.3 |
APS: Antiphospholipid syndrome; ARD: Autoimmune Rheumatic Diseases; CKF: Chronic Kidney Failure; DM: Diabetes Mellitus; HBP: High Blood Pressure; IM: Inflammatory Myopathies; MCTD: Mixed Connective Tissue Disease; RA: Rheumatoid Arthritis; SLE: Systemic Lupus Erythematosus; SS: Scleroderma; SV: Systemic Vasculitis.
The disease with the highest number of cases was SLE with 49.7%, followed by the MI with 15.1%, RA with 14.0%, SV with 7.0%, APS with 4.3%, SS with 3.7%, MCRD with 1% and other rheumatic diseases with 4.8% of cases. According to the time of disease evolution (from the time of diagnosis), on average 27 months, with MI being the lowest at 4 months and RA at 72 months, the highest. Regarding age at the time of death, the average was 40.62 years, with SLE being the lowest at 27 years and RA at 55 years the highest. Within the causes of morbidity, the most common were high blood pressure (HBP) at 38.9% and diabetes mellitus (DM) at 11.3% of cases. No morbidity was reported in 24.3%.
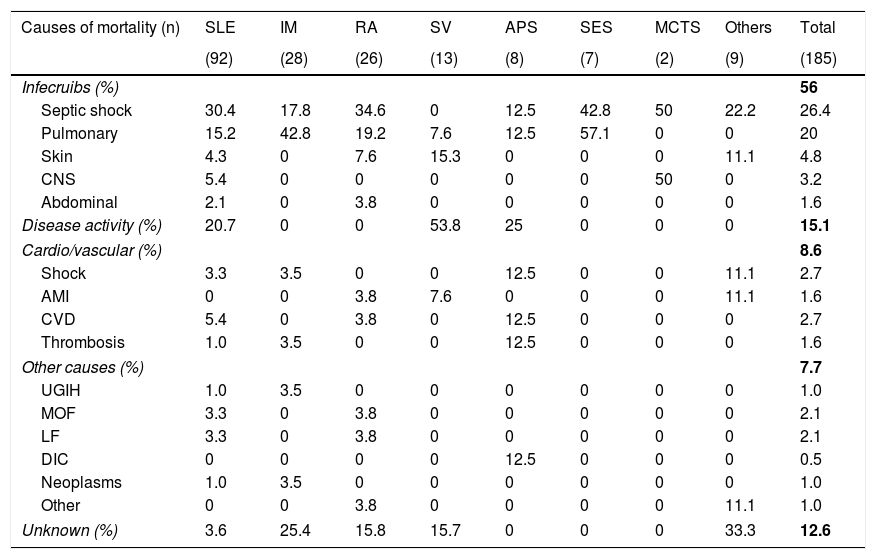
Table 2 contains the main causes of mortality, with infections being the most frequent at 56%, disease activity at 15.1%, and cardiovascular diseases at 8.6%.
Main causes of mortality distributed by ARD.
| Causes of mortality (n) | SLE | IM | RA | SV | APS | SES | MCTS | Others | Total |
|---|---|---|---|---|---|---|---|---|---|
| (92) | (28) | (26) | (13) | (8) | (7) | (2) | (9) | (185) | |
| Infecruibs (%) | 56 | ||||||||
| Septic shock | 30.4 | 17.8 | 34.6 | 0 | 12.5 | 42.8 | 50 | 22.2 | 26.4 |
| Pulmonary | 15.2 | 42.8 | 19.2 | 7.6 | 12.5 | 57.1 | 0 | 0 | 20 |
| Skin | 4.3 | 0 | 7.6 | 15.3 | 0 | 0 | 0 | 11.1 | 4.8 |
| CNS | 5.4 | 0 | 0 | 0 | 0 | 0 | 50 | 0 | 3.2 |
| Abdominal | 2.1 | 0 | 3.8 | 0 | 0 | 0 | 0 | 0 | 1.6 |
| Disease activity (%) | 20.7 | 0 | 0 | 53.8 | 25 | 0 | 0 | 0 | 15.1 |
| Cardio/vascular (%) | 8.6 | ||||||||
| Shock | 3.3 | 3.5 | 0 | 0 | 12.5 | 0 | 0 | 11.1 | 2.7 |
| AMI | 0 | 0 | 3.8 | 7.6 | 0 | 0 | 0 | 11.1 | 1.6 |
| CVD | 5.4 | 0 | 3.8 | 0 | 12.5 | 0 | 0 | 0 | 2.7 |
| Thrombosis | 1.0 | 3.5 | 0 | 0 | 12.5 | 0 | 0 | 0 | 1.6 |
| Other causes (%) | 7.7 | ||||||||
| UGIH | 1.0 | 3.5 | 0 | 0 | 0 | 0 | 0 | 0 | 1.0 |
| MOF | 3.3 | 0 | 3.8 | 0 | 0 | 0 | 0 | 0 | 2.1 |
| LF | 3.3 | 0 | 3.8 | 0 | 0 | 0 | 0 | 0 | 2.1 |
| DIC | 0 | 0 | 0 | 0 | 12.5 | 0 | 0 | 0 | 0.5 |
| Neoplasms | 1.0 | 3.5 | 0 | 0 | 0 | 0 | 0 | 0 | 1.0 |
| Other | 0 | 0 | 3.8 | 0 | 0 | 0 | 0 | 11.1 | 1.0 |
| Unknown (%) | 3.6 | 25.4 | 15.8 | 15.7 | 0 | 0 | 0 | 33.3 | 12.6 |
AMI: Acute Myocardial Infarction; ARD: Autoimmune Rheumatic Diseases; CNS: Central Nervous System; CVD: Cerebrovascular Disease; DIC: Disseminated Intravascular Coagulation; LF: Liver failure; MOF: Multiorgan failure; UGIH: Upper Gastrointestinal Haemorrhage.
Infections were the most common causes of death in SLE. IM. RA. Septic shock was reported in 26.4% and pulmonary infection in 20% of these cases.
Disease activity as a cause of death in SV was found in 53.8%, in APS in 25% and in SLE in 20.6% of cases. No known cause was reported in 12.6%.
Cultures were taken in 70.3% of cases (n = 130) and their distribution was as follows: in 20% (n = 26) of cases no germs were reported and in 80% (n = 104) of cases the germs most commonly found were distributed according to the anatomical site: respiratory system (n = 39); A. baumannii in 9.1%. K. pneumoniae in 5.4%. P. aeruginosa in 2.1% and negative cultures in 23%. In the genital-urinary system (n = 33) E. coli in 8.1%, Candida albicans in 5.9% and S. aureus in 1.6%, and negative cultures in 26%. In skin and nails (n = 20) P. aeruginosa in 5.4%, S. aureus in 3.7%, Streptococcus in 1.6% and 2 cases were negative. In the central nervous system (n = 5) C. neoformans was reported in 3 patients, M. tuberculosis in one patient, N. meningitidis in one patient, and negative cultures were reported in 4 patients. In the gastrointestinal system (n = 7). S. typhi was isolated in 3 patients, E. coli in 2 patients and C. difficile in 2 patients. 7 cultures tested negative.
Regarding therapy associated with cause of death, in 83% of cases some kind of treatment was reported. whilst in 17% none was. Of these, oral glucocorticoids were the most used and were reported in keeping with the dose: under 5 mg/day in 1.2%, 5−10 mg/day in 43.5%, 10−30 mg/day in 18.6% and 30−50 mg/day in 26.6%, and they were not used in 8.9% of cases. 94% of deaths by infection used glucocorticoids, and in 88.7% of these the dose was higher than 5 mg/day. 100% of deaths by disease activity used doses higher than 10 mg of oral and parenteral glucocorticoids.
The use of parenteral glucocorticoids was reported in 6.5% of cases, and the main drug used was methylpredinisolone. On average the number of intravenous infusions of 1000 mg was between 1 and 3 drug pulses, and in 82% of those who used it, infection was reported.
The use of disease-modifying drugs was reported in 81.1% and not used in 18.9% of cases. Methotrexate (MTX) was used in 29.7% of patients, azathioprine (AZT) in 27.8% and hydroxychloroquine (HCQ) in 1.7%.
The use of cyclophosphamide (CPM) was reported in 37.5% of cases, and the following was reported according to the number of monthly infusions of 1000 mg: between 1–3 pulses in 15.6% of cases, between 3–6 pulses in 15%, between 6–9 pulses in 4%, between 9–12 pulses in 2.6% of cases and there was no reported use of over 12 pulses.
In 72% of cases glucocorticoids were used combined with one of these drugs, and in 17% glucocorticoids were used with 2 of them.
The use of biologic therapy was reported in 5% of cases: rituximab (RTX) in 2.6%, adalimumab (ADA) in 1.3%, etanercept (ETN) in 0.6% and tocilizumab (TCZ) in 0.6%. Only one case of death by lung infection was reported for S. aureus.
Other reported treatments such as platelet antiaggregant were: aspirin in 20.2% of cases and anticoagulants in 15% of cases.
Regarding non-pharmacological treatment, at the outset kidney disease replacement therapy was reported: in haemodialysis in 10.4% of cases (94% in SLE) and peritoneal dialysis in 0.6%.
DiscussionThe study reported on the causes of mortality between autoimmune rheumatic diseases in a national benchmark centre. In Guatemala during this period (2009–2019) 857,395 people died with a general mortality rate of 4.7 per thousand inhabitants. In keeping with unpublished data from the department of statistics of the centre during the same period 15,110 adult deaths were reported from common diseases, with the following main causes: respiratory infections, cardiovascular diseases, chronic kidney disease and gastrointestinal bleeding. Of these, 185 cases or 1.2% resulted from RAD.
Previously in this institution in a similar study Cárcamo et al. reported a mortality of 26.17%, which was higher than that reported in our study (20.6%), with no intervention having played a part in this reduction. It could be simply an under-reporting of data, analysis of causes and associated factors that coincide with these current findings.5
As in the majority of reports, in this study females predominated with 85.9% de cases. Data relating to disease evolution are variable: in the case of IM it was short, at 4.5 months, and in SLE, 14 months, whilst in RA it was 72 months. Most studies have long follow-up periods which in our study did not appear to impact mortality.
The lowest age at death in SLE was 27 years, and the oldest patients were those with RA aged 55 years. In this context the Tselios et al. group, in a cohort of Ontario, Canada studied between 1971 and 2013, reported that mortality in SLE was later, at 53.2 years and the mean duration of the disease was 15.2 years, a difference which can be explained by the different nature of the health systems.2
Coinciding with the data of this study, the Mok et al. group, in a cohort in Hong Kong, China between 1999 and 2008 reported in SLE an average of 44.3 years and in RA 56.4 years.3 The group of Toledano et al. reported in their meta-analysis an average age for RA of 54 years and for SLE 34 years.1 Martínez et al., in a cohort in Mexico between 2001 and 2012 found that the average age in SLE was 29.7 years.4 The differences found could be explained by different factors between them: the differences in access to the health systems and policies, delay in diagnosis, adherence to treatment and the socioeconomic status which requires designing studies for these purposes.1–3
Of mortality-associated comorbidities in ARD, those of the highest prevalence were HBP at 38.9% and DM at 11.3%. Specifically, in SLE 50% reported HBP, 8.7% APS-associated thrombosis and 6.5% IRC. In RA the main association was HBP in 26.9% and DM in 23% of cases. In 24.3% no comorbidity was reported.
These data are similar to those reported by Panoulas et al., in a study on comorbidity in autoimmune systemic diseases which reported double the prevalence of HBP in comparison with the general population.6 In the Petri et al. group they also found there was an association, particularly in women with SLE under 40 years of age.7 Sabio et al. reported HBP in 40% of patients with SLE under 40, compared with the 11% of controls of the same age.8 The suggested relationship for this phenomenon could be explained by the constant inflammatory state which affects the blood vessels in the kidney and the central nervous system.
Relating to the causes of mortality in this study, we found that infections explain 56% of deaths and disease activity 15.1%. compared with that reported by Toledano et al., where cardiovascular disease and cancer were the most common causes of death and infections and respiratory complications were considered to be related to an increase in mortality;1 these data differ from those found in this study where cardiovascular comorbidities and neoplasms were not frequently reported, which could be explained by the differences in reported ages.
Mok and other researchers have reported similar data to those of our study regarding the causes of death: infections (28%) and disease activity (7%). which differ from that reported for cardiovascular/cerebrovascular complications (18%) and neoplasms (16%).3,9 Berlatsky et al. also calculated an SMR of 2.4 in SLE, especially in cardiovascular disease.10 and the Tselios et al. study differs from ours in cardiovascular comorbidity of 15.7% versus 8.6% and neoplasms of 9.6% versus 1%, whilst infections of 24.5% and disease activity of 13.3% were similar to our study.2
In this study septic shock represented 26.4% as the main cause of death and the associated germs reported were gram negative bacilli (A. baumannii. K. pneumoniae and P. aeruginosa). Gram positive cocci (S. aureus) and other opportunistic germs (C. albicans). These data coincide with that reported in the study by Juárez et al.11
For the last 5 decades patients’ survival with rheumatic diseases has significantly improved due to the use of drugs such as glucocorticoids, immunosuppressants, monoclonal antibodies and concomitant drugs (antihypertensive agents, antibiotics, etc.). However, there has also been an increase in the risk of developing infections, particularly from the extended use of glucocorticoids. In our study, 94% of patients reported at least one infection. This relationship was reported by Saag et al. who found an OR of 8 of developing infections.12 The Petri et al. study reported in patients hospitalised for SLE an average dose of prednisone higher than 10 mg/day increased the risk of infection compared with patients who were not hospitalised.7 Listing et al. in RA found that doses of glucocorticoids above 5 mg was associated with an increase in mortality.13 In our study 88.7% of cases of deaths used higher doses than 5 mg/day.
In this study the use of the majority of disease-modifying drugs such as MTX, AZA, HCQ, CFM and monoclonal antibodies were reported. Bultink et al.14 stratified the risk of mortality in patients with SLE with the use of glucocorticoids and immunosuppressants in accumulative doses, reporting an increase in the risk of OR: 3.60 (95% CI: 2.12–3.20) with an accumulation of glucocorticoid dosing. The accumulative HCQ dosing is associated with a lower risk of mortality and the risk of mortality was not statistically significant for any other immunosuppressant drug, whilst Moket al.15 did not report that the use of immunosuppressants was associated with higher survival in patients with SLE. However, the risk of infections did increase. Similarly, Listing et al. Reported that the use of MTX or MTX + TNF inhibitor demonstrated a poor association with mortality OR: 0.64 (95%CI: 0.50–0.81) and in the case of rituximab OR: 0.57 (95% CI: .39–.84).13
These data obtained from different studies could not be extrapolated to ours, since methodology and statistical analysis were different. Already in a previous study conducted in this centre, a high risk of death was reported with the use of MTX, CFM and high doses of glucocorticoids.5
ConclusionThis study provides information on the characteristics of mortality in patients with rheumatic disease in a specific population and shows the differences found compared with other centres.
The main conclusion was to identify infections as the most common cause of death, with disease activity also being a high percentage.
The major limitations to this study could be the under-recording of diagnoses and causes of death, and also that the population studied was not representative of the general population with rheumatic diseases, as this sample was obtained from a single centre. Findings may therefore not be extrapolated.
FinancingThis research did not receive any specific funding from public sector, commercial sector or not-for-profit agencies.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Leonardo H, Carrascosa M, Arreola R, Herrera-Méndez M. Causas de mortalidad asociadas a enfermedad reumática autoinmune en un hospital de referencia. Reumatol Clin. 2022;18:304–308.