The clinical anatomy of several pain syndromes of the knee is herein discussed. These include the iliotibial tract syndrome, the anserine syndrome, bursitis of the medial collateral ligament, Baker's cyst, popliteus tendon tenosynovitis and bursitis of the deep infrapatellar bursa. These syndromes are reviewed in terms of the structures involved and their role in knee physiology. All of the discussed structures can be identified in their normal state and more so when they are affected by disease. The wealth of information gained by cross examination of the medial, lateral, posterior and anterior aspects of the knee brings to life knowledge acquired at the dissection table, from anatomical drawings and from virtual images.
En este artículo se revisa la anatomía clínica de varios síndromes dolorosos de la rodilla. Estos incluyen el síndrome de la bandeleta iliotibial, el síndrome de la pata de ganso, la bursitis del ligamento colateral medial, el quiste de Baker, la tenosinovitis poplítea y la bursitis infrapatelar profunda. El análisis anatómico de estos síndromes revela una multiplicidad de estructuras identificables en su estado normal y más aún en las tendinosis o cuando hay un derrame sinovial. El examen cruzado de las estructuras mediales, laterales, posteriores y anteriores de la rodilla provee aspectos dinámicos que complementan su estudio por disección, láminas anatómicas e imágenes virtuales.
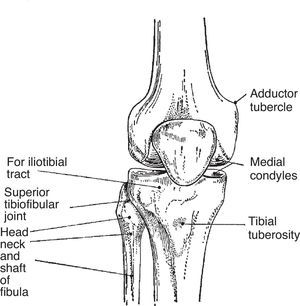
The knee is the largest synovial joint in the body and one of the most complex biomechanical systems known.1,2 This joint includes a condyloid joint between the condyles of the femur and the tibia and a saddle joint between the posterior surface of the patella and the patellar surface of the femur (Fig. 1). The upper tibiofibular joint, which is not involved in weight bearing, frequently communicates with the femorotibial joint.3
This simple diagram shows 2 most important attachment sites. One is “for iliotibial tract”. This site is unnamed in the Terminologia Anatomica but is widely known by clinicians as lateral tubercle of tibia or Gerdy's tubercle. The other site is the tibial tuberosity where the patellar tendon attaches.
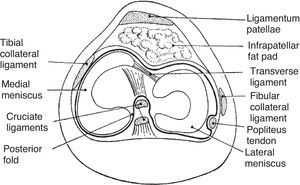
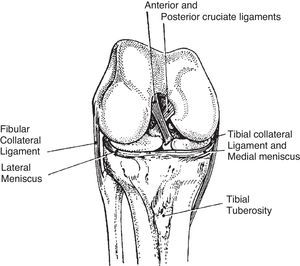
The main movements of the knee are flexion between 120° and 150° and extension between 5° and 10°.3 With maximal extension the knee “screws home” as the medial femoral condyle slides back on the medial meniscus and tibia while the lateral femoral condyle remains in place, locking the joint. This rotation movement initiates at 70° extension and becomes maximal in the last 10°.4 To unlock the knee, at the very beginning of flexion the popliteus muscle (P), taking hold on the tibia, pulls back from the lateral femoral condyle and causes a reciprocal forward movement of the medial femoral condyle on the medial meniscus and tibia (Fig. 2), reversing the locking of the joint.4,5 External and internal rotations of the tibia relative the femur are best shown with the subject sitting and the knee flexed 90°. External rotation is 30–40° and internal rotation is about 10°, the difference being explained by the twisting of the cruciate ligaments during internal rotation (Fig. 3).6 The efficacy of tests for the integrity of specific knee components has been reviewed.7
Sketch of a transverse section of the knee. The medial meniscus is like a C and the lateral meniscus almost like an o. The fibular collateral ligament is extracapsular. The tibial or medial collateral ligament is capsular. The cruciate ligaments and the initial portion of popliteus tendon are intracapsular but extrasynovial.
The knee joint is the most frequent source of musculoskeletal pain. Within the joint, there are structures that when irritated cause localized pain and others which are hard to pin point.8–10Table 1 lists conditions that cause knee pain according to its location. The six prototypical cases that follow will serve to review the clinical anatomy of the knee region.
Causes of knee pain according to location.
| Anterior |
| • Prepatellar or pretendinous bursitis |
| • Quadriceps tendon tendinitis |
| • Articularis genu muscle disorders? |
| • Chondromalacia patella |
| • Patellofemoral osteoarthritis |
| • Plica medio patellaris |
| • Tight lateral retinaculum |
| • Patellar tendon tendinitis |
| • Osgood-Schlatter disease |
| • Infrapatellar bursitis |
| • Hoffa's body inflammation |
| Lateral |
| • Iliotibial tract syndrome |
| • Bicipital tendon tendinitis |
| • Lateral meniscus tears and cysts |
| • Popliteus tendon bursitis (posterolateral) |
| Medial |
| • Anserine syndrome |
| • Medial meniscus tears |
| • Medial plica syndrome |
| • Medial (tibial) collateral ligament bursitis (“no-name, no-fame bursa”) |
| • Semimembranosus bursitis |
| Posterior |
| • Lymphadenopathy |
| • Thrombophlebitis |
| • Popliteal arterial aneurysms |
| • Mucoid degeneration of popliteal artery wall |
| • Baker cysts |
| • Ganglia |
| • Sarcomas |
Patient 1. Iliotibial tract syndrome. “A 30 year old woman recently undertook running and is seen because of a lateral left knee pain that appears about 10minutes into her running”.
Lateral knee pain that appears upon running may have several causes of which the most common is the iliotibial tract (ITT) syndrome.11 Pain in the ITT is maximal at 30° flexion and tenderness, usually with a burning quality, can be elicited by digital pressure on the lateral femoral epicondyle during flexion and extension movements of the knee.12 The cause of this syndrome is repetitive pressure of the ITT against the lateral femoral epicondyle. At this site swelling of the underlying soft tissues, rather than a distended bursa, can be shown by post-exercise ultrasound (US) and magnetic resonance imaging (MRI) studies.13
Relevant Anatomy Amenable to Self- and Cross-recognitionThe ITT is a lateral thickening of the deep investing fascia of the thigh, otherwise known as fascia lata. Proximally, the ITT attaches to the iliac crest. Once at the greater trochanter two muscles insert in the ITT, tensor fascia lata (TFL) anteriorly and most fibers of gluteus maximus (GM) posteriorly. The ITT descends along the thigh in parallel with the femoral shaft. Distally, the ITT inserts in the lateral tubercle of the tibia also known as Gerdy's tubercle. This tubercle is a large, readily palpable, often visible landmark which varies markedly in size and shape among people that can be found about 3cm lateral to the tibial tuberosity. The ITT itself can be seen as a vertical band that becomes distinct and prominent when the knee goes into extension and seems to fade in flexion, its course being roughly in parallel with biceps femoris (BF) tendon. The ITT appears to move forward in knee extension, covering the femoral epicondyle, and backward in flexion. This back-and-forth motion is apparent rather than real and is the result of selective fiber tension according to position, its posterior fibers tensing in flexion and its anterior fibers tensing extension, giving the illusion of motion. At any rate, true motion would have been prevented by strong connective tissue strands that anchor the ITT to the femoral epicondyle and the bone surface just proximal to it.12 Thus, the underlying tissue injury caused by running does not result from friction but from a repetitive, constantly changing pressure gradient onto the lateral condyle epicondyle.
Patient 2. Anserine syndrome. “An obese 50 year old woman complains of medial right knee pain”
Patient 3. No name-no fame bursitis. “A 50 year old man undertook running after many years of sedentary life (he is a hematologist). After exercising for two weeks he has developed medial knee pain. On PE there is a 2cm tender, fluctuant area medial to the upper tibia best shown in semiflexion”.
Medial knee pain can be caused by several conditions, the most frequent being the anserine syndrome.14,15 This designation shies away from implying a pathogenetic role of the bursa present in the region. Patients complain of knee pain that characteristically increases when ascending and descending stairs and while lying in bed with the knees in apposition. There is no pain in flexion and extension of the knee. The tenderness, that is diffuse, is located a few cm distal to the medial joint line. Predisposing factors for the anserine syndrome include osteoarthritis of the knee, valgus angulation and obesity. A proposed association with diabetes was not confirmed.16
Pes anserinus. In Latin and old Spanish “anser” means goose. Indeed, when the 3 tendons that make up the “pes” (foot) anserinus are cut, the insertion is said to resemble the footmark of a goose. This has not been confirmed in recent studies of the medial aspect of the knee.17 Pes anserinus is not an officially recognized designation in the Terminologia Anatomica; however, it is a widely used name for a very common condition. When a knee in extension is looked at from the front, particularly in women and especially in those who have genu valgum and are overweight, a broad convexity is seen that overlies the inner aspect of the joint. Have the subject flex the knee, even a few degrees, and the convexity disappears. What has happened? The muscles and tendons that make up pes anserinus, which stack up medial to the knee in extension, move back, along with the subcutaneous fat that overlies them, as the knee is flexed. This phenomenon emphasizes once again the differences between the anatomy that is learnt from pictures and the dynamic anatomy that lies every day before our eyes. The pes anserinus muscles are, from medial to lateral (or from surface down), sartorius (S), gracilis (Gra) and semitendinosus (ST). Their origins are far from each other: the anterosuperior iliac spine and a notch below it for S, the body and inferior ramus of pubis for Gra, and the superomedial part of the ischion for ST. A bursa between the pes and the tibia and adjacent medial collateral ligament, the anserine or sartorial bursa, enjoys an unwarranted fame as it only rarely displays pathology. Indeed, in the anserine syndrome which is widely known as “anserine bursitis”, US studies have failed to show bursits or clear-cut tendon pathology.18 Although it has been suggested that the pain results from medial collateral ligament stretching in people with a knee valgus deformity, it is fair to say that the pathogenesis of anserine syndrome remains unknown.16 Another interesting negative finding regarding these structures is that the complex pes anserinus/sartorial bursa is not involved in spondyloarthritis. This may be due to a lack of axial load which prevents sesamoid and periosteal fibrocartilague differentiation and thus excludes its participation in enthesitis.19
Anserine syndrome is usually improved, at least in the short term, by a steroid infiltration. The technique of injection we use (no priority claim here) is described because it is a good technique and, as the real reason, to reinvigorate the attendants’ interest in the seminar. The site for needle entry is determined, with the patient's knee in semi-flexion, by following the sharp ST tendon to the tibia. A mark is made at this site and the knee is extended. Then, with a syringe that contains a mixture of local anesthetic and a depo-steroid, a fan-like infiltration is made using a 21-gauge needle along the slightly diverging course of the tendons.20,21
No name-no fame bursitis is a rare bird. Bursitis affecting this bursa, that is placed between the medial collateral ligament and the upper medial tibia, can be diagnosed when a distended and tender sac can be felt between the skin and bone in knee flexion, as the bursa is exposed, and not in extension when the medial collateral ligament moves forward and covers the bursa.22 No description of this injection will be made beyond saying that is well in the reach of an insulin needle.
Patient 4. Baker cyst. “A 50 year old woman with knee OA has popliteal pain and describes perimalleolar swelling by the end of the day”
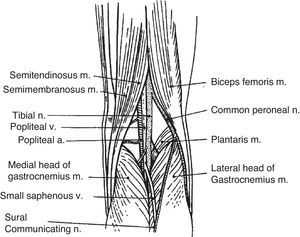
In a patient with swelling of the distal leg plus past or present knee pathology a Baker cyst must be placed highly in the differential diagnosis list. This case lends itself to discuss the anatomy of the popliteal fossa, the location and characteristics of the gastrocnemius–semimembranosus (GN-SM) bursa, the acquired communication between this bursa and the joint, the differences between a normal communicating bursa and a Baker cyst and the pathophysiologic bases for the treatment of this cyst (Fig. 4).
A simple drawing of the popliteal fossa. Baker cysts occur by distention of a communicating gastrocnemius–semimembranosus bursa. This bursa is placed in the junction of the middle third and the lateral 2/3 of the popliteal fossa.
Because in the evaluation of a patient with a possible Baker cyst the presence of a knee effusion is such an important finding it is pertinent to review how knee effusions are identified. All diarthrodial joints, among them the knee, normally contain a small amount of synovial fluid (SF). These small volumes cannot be identified by clinical maneuvers but their aspiration is possible by using a large bore needle and pulling hard and long from the syringe's embolus. Is the aspiration of these trace amounts of any practical importance? Yes, mainly for crystal identification in intercritical gout and the diagnosis of calcium dehydrate deposition disease in asymptomatic individuals with chondrocalcinosis, as crystals are almost regularly identified in these settings.23,24 Small effusions of around 5ml are best identified by the pop-up sign. In this maneuver the medial parapatellar recess is gently squeezed up toward the suprapatellar bursa. Then, a gentle pressure is applied on the pouch with the hand flat. In patients with a small effusion the medial parapatellar recess is seen to pop up. Larger effusions, such as 10ml or larger, are best palpated bimanually. The non-dominant hand is applied flat on the suprapatellar bursa while the thumb and index of the dominant hand are placed on the medial and lateral parapatellar recesses. Reciprocal, gentle pressures cause the fluid to enter the bursa or fill the recesses. Large effusions are seen as a bulge proximal to the patella (the suprapatellar bursa) and medial and lateral to the patella (the medial and lateral recesses). Doppman25 has shown in large effusions that by extending the knee the fluid collected in the back of the joint is shifted forward distending the suprapatellar bursa and lifting the patella. Conversely, in knee flexion, the pressure exerted on the effusion by the quadriceps and the patella pushes the fluid back, peels the capsule from the femora condyles and fills connecting G-SM bursae. Based on US, the detection of fluid in the suprapatellar bursa is improved by an isometric quadriceps contraction.26 This counterintuitive finding may be explained by the contraction of articularis genus muscle,27 a small, multiple-layered muscle that inserts in the femur and the proximal and/or the posterior walls of the suprapatellar bursa and shares innervation with quadriceps. Thus, the simultaneous contraction of quadriceps and articularis genus could act like a suction pump bringing back synovial fluid into the suprapatellar bursa. More difficult to explain, although unquestionable for the volume of the effusions studied, were the findings of an ultrasound study in which fluid in the suprapatellar bursa was best seen at 30° flexion.28
The popliteal fossa. The popliteal fossa (Fig. 4) has a rhombus shape that is more clearly figured out in anatomical plates than “in vivo”. With the volunteer lying on the examining table, face down, the popliteal fossa, rather than showing a depression, usually bulges out. This is caused by subcutaneous fat which varies in amount according to the person's make up and weight and should not be mistaken for a Baker cyst. Of the 4 sides of the rhombus the upper 2 are, medially, the ST tendon that lies on SM (this muscle remains fleshy almost to its insertion which makes it undetectable on palpation), and laterally, BF. Going up the thigh, particularly in strong people, SM appears to coalesce with BF without a dividing line. The distal 2 sides of the rhombus are, medially, the medial head of G and laterally, the lateral head of G. It should be recalled that the medial head of G has its origin above the medial femoral condyle and its lateral head, in the upper part of the lateral femoral condyle and adjacent supracondylar line. Plantaris (Pla) muscle shares insertion with the lateral head of G. Contained in the rhombus, from deep to superficial and from medial to lateral lie the popliteal artery, the popliteal vein and the tibial nerve. The area that concerns us at this time, however, is the contact area between SM in his way to the posterior upper tibia and the medial head of G in his way to its supracondylar origin. At this site, flexion movements of the knee separate these muscles and extension brings them together.29 In addition, at the beginning of flexion and at the end of extension an area of friction is created. A bursa at this site promotes gliding and allows harmless motion. This is the G-SM bursa, the anatomical substrate of the Baker cyst. Medial head of G and SM are placed behind the medial femoral condyle and so is this bursa. Lindgren, Willen and Rauschning,30,31 in a series of landmark anatomical studies determined the timing, the frequency and the nature of this acquired communication. The communication is absent in the first decade of life but reaches 10% in the 2nd decade, 20% in the 3rd decade 30% in the 4th decade, 40% in the 5th decade, reaching a top frequency of 50%–60% thereafter. Thus, once a communication is established, a knee effusion of any nature will fill the bursa which if large enough will result in a Baker cyst. Although the sequence of events leading to the acquired communication are still unknown, based on findings in the contralateral knee in unilateral cases, the posterior capsule becomes paper thin at the bursal site. The gap is an 18(4–24)mm wide transverse slit that separates the capsule from G.31 We have wondered whether this capsular wear results from the posterior displacement of the medial femoral condyle every time the knee is locked in extension.
There is quite a difference between a communicating bursa and a Baker cyst. When fluid enters a communicating bursa the filling occurs in flexion when the capsular gap opens and G and SM separate. As the knee is extended G and SM come together and the bursa, placed in between, empties its content into the knee and the capsular gap closes. Thus, normal communicating G-SM bursae should not be detectable in US studies performed in full knee extension. In a Baker cyst, a larger volume of distention causes part of the bursa to lie superficial to the muscles and in extension this portion of the sac, unable to empty, becomes compressed by the unyielding popliteal fascia. This makes popliteal cysts become soft and even undetectable in flexion and hard in extension.29 This finding on examination is known as the Foucher sign of the Baker cyst. Solid and true cystic lesions of the popliteal fossa do not soften in flexion, i.e., have a negative Foucher sign. The usefulness of this sign was evidenced by a recent referral to one of the authors. A 50-year-old male with B-cell lymphoma in remission was sent by his oncologist for evaluation of a popliteal mass with a presumed diagnosis of a Baker cyst. He was a strongly built, healthy looking male with a tennis ball size mass in the right popliteal fossa. There was no knee effusion. The mass was firm and its consistency was unchanged by knee flexion. Given his background and the negative Foucher sign he was sent back to his oncologist with a likely diagnosis of recurrent lymphoma in the superficial popliteal nodes, which was proven by a PET scan.
Popliteal vein compression causes swelling, pain, and rarely, venous thromboembolism. Swelling of the leg in Baker cysts may result from venous compression, synovial fluid leakage or cyst rupture. The role of lymphatic ectasia in the leg edema caused by an unruptured popliteal cyst remains to be determined.32 Baker cysts may compress the tibial nerve and cause gastrocnemius muscle atrophy, paresthesias, and pain. Very unusually, isolated arterial compression may result in intermittent claudication.33 A rare complication of a Baker cyst is an acute or chronic compartment syndrome.34 Baker cysts are best shown in US studies which are additionally useful to rule out concurrent or maskerading phlebitis.35
In children, since the capsular opening that allows the filling of the bursa has not yet formed, popliteal cysts have long been held to be the result of direct trauma that causes irritation of the bursa and a loculated effusion. While this concept is true in a normal school population it is not true in patients with inflammatory arthritis such as rheumatoid arthritis. In contrast to what should be expected, the rate of bursal communication in these children is 50% or more. This finding, initially shown by Szer in 1992 was confirmed in a recent series.36,37 It could be concluded that in RA the damage inflicted by inflammation adds to the normal wear of the capsule, causes an early communication and sets the conditions to develop a pediatric communicating Baker cyst.
Patient 5. Popliteal tenosynovitis. “A 61 year-old woman consulted with right posterior upper leg pain. Pain was absent while lying in bed, appeared upon raising and went away after taking a few steps. On examination there was a small knee joint effusion and tenderness at the posterolateral joint line as well as posteriorly on the upper tibia. An MRI showed a small joint effusion and fluid in the synovial sheath of popliteus tendon. Symptoms went away 24hours after a steroid injection in the joint cavity”.
Although we have no direct proof that the pain originated in the popliteus sheath in this patient, there are three lines of evidence pointing to this diagnosis. First, pain occurred concurrent with the posterior sliding of the medial femoral condyle upon full extension which is the position in which popliteus muscle, which spans the lateral femoral condyle and the upper posterior tibia, would be maximally stretched. Secondly, there was tenderness at the both the origin and the insertion of popliteus. Third, an MRI showed fluid accumulation at the popliteus synovial investment.
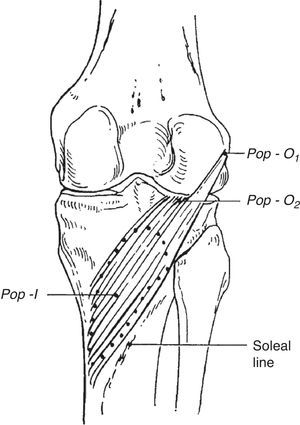
Popliteus has an intraarticular, tendinous origin in the lateral femoral condyle below the attachment of the fibular collateral ligament (Fig. 5). Additional attachments include the posterior horn of the lateral meniscus and the fibula. The tendon is invested for some distance by knee synovium (the popliteus bursa) as a superior and an inferior recess or as a complete investment by coalescence between the two leaving the tendon free in the lumen.1,38,39 The popliteus tendon has a downward and medial course, and emerges in the popliteal fossa from under the arquate ligament where it takes an additional fleshy insertion. Now muscle, it takes a broad fleshy insertion in the back of the tibia above the soleus.
Popliteus muscle. Two insertions are shown, in the lateral femoral condyle below the epicondyle and in the back of the lateral meniscus. Its insertion is in the posterior surface of tibia above soleal line.
Case 6. Infrapatelar entheseal organ inflammation. “A 14 year-old boy with spondyloarthritis diagnosed at age 12 is seen because of pain and swelling in both knees”
Deep infrapatellar bursa. This bursa, which is wedged between the patellar tendon and the tibia exhibits homology with the retrocalcaneal bursa.40 Although less well-defined than in the retrocalcaneal bursa, there is sesamoid fibrocartilage in the back of the patellar tendon, periosteal fibrocartilage in front of the tibia, and an apron or wedge of synovium-covered fat that hangs from Hoffa's infrapatellar fat pad on the top. The deep infrapatellar bursa, the adjacent patellar tendon enthesis, the fat pad and the subperiosteal bone are all components of the infrapatellar enthesis organ.19 In our patient there was a marked swelling of the knee predominantly in the infrapatellar region where bulging was seen (Figs. 6 and 7). An MRI study revealed fluid not only in the infrapatellar bursa but also in the synovial cavity of the knee and the soft tissues anterior to the patella.
- •
Patellar tendon
- •
Projection of the suprapatellar bursa
- •
Lateral and medial parapatellar recesses
- •
Lateral border of the femoral condyles
- •
Tibial plateaus
- •
Patellar tendon
- •
Hoffa's fat pad, changes in the insertional angle with knee flexion
- •
Hoffa's fat body apron or wedge that tops the deep infrapatellar bursa
- •
Tibial tuberosity
- •
Lateral tibial tubercle (Gerdy)
- •
Sartorius
- •
Gracilis
- •
Semitendinosus
- •
Pes anserinus
- •
Anserine bursae
- •
Medial collateral ligament
- •
No name, no fame bursa
- •
Medial meniscus and its relationships with the medial collateral ligament
- •
Medial plica
- •
Insertions of semimembranosus
- •
Lateral femoral epicondyle
- •
Iliotibial tract
- •
Biceps femoris
- •
Lateral collateral ligament
- •
Popliteal fossa
- •
Subcutaneous fat
- •
Semitendinosus and semimembranosus
- •
Biceps femoris
- •
Medial gastrocnemius
- •
Lateral gastrocnemius
- •
Plantaris
- •
Foucher sign of the Baker cyst
- •
Popliteus muscle origin and insertion
- •
Condylar attachment of the lateral collateral ligament as a marker of popliteus tendon insertion
- •
Role of popliteus muscle in knee unlocking
The authors have no conflict of interest to declare.