Sarcoidosis is a chronic inflammatory disease with unknown cause characterized by non-caseating granuloma formations. It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and symptoms on the locomotor system. FMF (Familial Mediterranean Fever) is an autosomal recessive autoinflammatory disease, characterized by recurrent episodes of fever and polyserositis. Simultaneous occurrence of these diseases is rare. In this paper, we reported the coexistence of sarcoidosis with FMF.
La sarcoidosis es una enfermdad inflamatoria crónica de origen desconocido caracterizada por formaciones de granulomas no caseificantes. Puede manifestarse con linfadenopatía hiliar bilateral, lesiones cutáneas, afectación ocular y síntomas en el aparato locomotor. La FMF (fiebre mediterránea familiar) es una enfermedad inflamatoria autosómica recesiva que se caracteriza por episodios recurrentes de fiebre y poliserositis. La concurrencia simultánea de ambas patologías es poco frecuente. En este artículo se presenta la coexistencia de sarcoidosis con FMF.
Sarcoidosis is a chronic inflammatory disease with unknown cause characterized by non-caseating granuloma formations. It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and symptoms on the locomotor system.1 Familial Mediterranean Fever (FMF) is commonly seen autoinflammatory disease with an autosomal recessive pattern of inheritance.2 The disease is characterized by clinically recurrent fever and polyserositis attacks and pathogenically a mutation in the MEFV gene which is located on short arm of chromosome 16 causes the disease.3 FMF primarily affects Turkish, Armenian, Arab and Jewish populations.4 In this paper we mentioned about a patient with sarcoidosis who was monitored for 10 years was diagnosed with FMF in addition to sarcoidosis as a result of the examination of her recent increasing complaints.
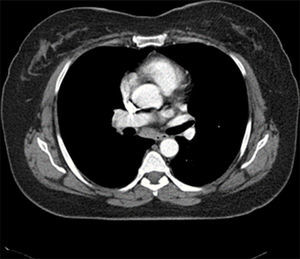
Case report50 years old female patient who was diagnosed with sarcoidosis 10 years ago was admitted to our rheumatology clinic with complaints of fatigue, recurrent fever, dry cough, and arthralgia. During her examination, she described recurrent abdominal pain and fever attacks which occur since her childhood. There is no known feature in her family history and she does not identify FMF in her family. Her medical history revealed that she was examined for a cough and she had a diagnosis of sarcoidosis supported with lymphatic gland biopsy 10 years ago. After 2 years of corticosteroid treatment, her disease restrained, she discontinued to treatment with medication and patient was not present for the subsequent control sessions. Patient's physical examination showed; 38.5°C fever, sensitivity in both ankles and hip joints and negative results for FABER(Flexion, ABduction, External Rotation) and FADIR(Flexion, ADduction, Internal Rotation) tests. In her systemic examination, rough lung sounds were determined during auscultation. There is palpable lymphadenopathy in her right axillar area. In laboratory tests; fasting blood glucose, liver, and renal functions were normal. CBC, thyroid function tests and routine urinalysis were normal. Acute phase reactants were investigated; C-reactive protein (CRP) was 4.03mg/dl (normal 0–0.5mg/dl), and sedimentation rate was 43mm/h (normal 0–20). In serological tests, negative results for RF, ANA, anti-CCP, ANCA, anti-dsDNA was determined. Hepatitis markers (HBV, HCV, HIV) was normal. Serum ACE level was high (87U/L; normal range: 8–52U/L) (Table 1). Her chest X-ray was normal, however, multiple mediastinal and hilar lymph nodes with the greatest dimension of 1cm was identified in her thoracic CT (Fig. 1). Results were consistent with stage 1 sarcoidosis. Regarding the patient's history, the FMF mutation tests were requested. In the FMF gene analysis all M694V, E148Q, R202Q mutations were found in the heterozygous state. After the clinical, radiological, and genetic observation and results of the laboratory test, diagnosis of sarcoidosis with FMF was considered. We made differential diagnosis; lymphoma, infection, other rheumatic diseases (such as connective tissue diseases) were exluded according to investigations. Three times daily oral treatment with NSAIDs and Colchicine 0.5mg tablets was initiated. In her follow-up examination after 3 months, a significant regression in her clinical symptoms was observed and she reported that there are no abdominal pain or fever attacks. Control acute phase reactants were investigated and the levels were determined as normal. Outpatient follow-up is still in progress for the patient with representing overall good condition.
Laboratory findings of the patient with sarcoidosis and FMF.
| Hemoglobin | 12.9g/dl | 10.8–14.9g/dl |
| WBC | 7300μL−1 | 3040–9640μL−1 |
| Platelet count | 269,000μL−1 | 150,000–400,000μL−1 |
| BUN: blood urea nitrogen | 13mg/dl | 7–20mg/dl |
| Creatinine | 0.67mg/dl | 0.5–0.9mg/dl |
| Uric acid | 6.8mg/dl | 3.4– 7mg/dl |
| ALT | 23U/L | 0–31U/L |
| AST | 27U/L | 0–32U/L |
| Calcium | 11.2mg/dl | 8.6–10.2mg/dl |
| Total protein | 7.8g/dl | 6.4–8.3g/dl |
| Albumin | 4.5g/dl | 3.4–4.8g/dl |
| TSH | 1.56ng/dl | 0.27–4.2ng/dl |
| CRP | 4.03mg/dl | 0–0.5mg/dl |
| ESR | 43mm/sa | 0–20mm/sa |
| RF | 7.9IU/ml | 0–14IU/ml |
| ACE | 83U/L | 8–52U/L |
In this paper, we reported the comorbidity of sarcoidosis and FMF. Until now, only a few cases reported comorbidity of sarcoidosis and FMF. As a result of their investigation, Erten et al. diagnosed acute sarcoidosis (Löfgren syndrome) and FMF together in 61 years old patient who admitted with the presence of erythema nodosum and recurrent fever and abdominal pain attacks.5 Corticosteroids, methotrexate, colchicine controlled the patient's complaints after the treatment. Aktimur et al. reported that a 53 years old patient who was monitored with FMF diagnosis and had appendectomy 34 years ago was diagnosed with sarcoidosis based on biopsy from scar tissue and pathological evaluations.6 Scar sarcoidosis was considered for this patient with no systemic symptoms and he was just monitored. In another report, 42 years old male patient using IFN-alpha due to the FMF was subjected to thorax CT due to the development of exertional dyspnea showed bilateral hilar lymphadenopathy.7 Depending on his histopathological evaluation, he was diagnosed with sarcoidosis and a causal relationship tried to be established between disease and medication. In literature, the development of sarcoidosis in patients treated with anti-TNF-alpha is also reported.8 In our case, without any drug relationship, we reported the coexistence of sarcoidosis and FMF. However, the presence of MEFV mutation may cause symptoms other than FMF and/or may determine the course and prognosis of some rheumatologic diseases. Sever et al. investigated mutation frequency of MEFV gene in patients with sarcoidosis.9 Low frequency of MEFV gene mutation was reported in patients with sarcoidosis compared the control group. This gene is thought to have a protective effect with respect to sarcoidosis because it less frequently occurs in patient with sarcoidosis than normal Turkish population. Sarcoidosis is a granulomatous disease with different clinical features. The etiology of sarcoidosis is unknown, however, it is suggested that genetic and immunologic factors might have an important role in the development of the disease.10 The low virulence due to the inadequate immune response causes the formation of permanent antigen. As a result of Th1 mediated immune response, development of accumulation of lymphocytes, macrophages and mononuclear phagocytes and non-caseating granulomas formation occurs in the affected organ. On the other hand, FMF is an autosomal recessive autoinflammatory disease, characterized by recurrent episodes of fever and polyserositis. The underlying cause of the disease is the mutation in MEFV gene which codes for proteins called pyrin or marenostrin. There is no common connection between sarcoidosis and FMF. Early-onset sarcoidosis (Blau syndrome) is also an autoinflammatory disease like FMF. The pathogenesis of Blau syndrome revealed that NOD2/CARD15 gene mutations cause the disease. Possibilities of different clinical presentations of the same disease in adults with sarcoidosis are discussed in the literature. In adult sarcoidosis, the presence of self-limited acute skin lesions, locomotor system symptoms and the regression of non-treatable disease suggest that this may be an autoinflammatory disease. Therefore, it may have common features and/or etiopathogenesis. In fact, while our patient already has sarcoidosis, she also diagnosed with FMF after gene analysis. In conclusion, the coexistence of sarcoidosis and FMF have been reported in few cases in the literature. The fact that both diseases are chronic and inflammatory suggesting the possibility of common etiopathogenesis and/or coincidence. New studies are necessary for investigation of this subject.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Right to privacy and informed consentThe authors declare and guarantee that they are in possession of a document signed by the patients whose personal data is included in the article.
Conflict of interestThe authors declare not any conflict of interest or financial support.