A 33-year-old male consulting due to behavioural disorders, aphasia, severe occipital headache, unstable gait, and hearing loss. He denied substance abuse.
The following were highlighted on examination: absence of meningeal signs, sparse language with bradylalia, bradypsychia, amnesia and temporary disorientation.
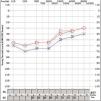
Complementary studies: haemogram, general biochemistry, C reactive protein and coagulation, normal. Lumbar puncture showed hyperproteinorrhoea, with Gram, panbacterial and myobacterial negative PCR. Lues serologies, HIV and neurotropic virus, as well as ANA, ANCA and HLA-B5 were negative. A video-EEG showed signs of mild diffuse encephalopathy and cranial CT was normal. Cranial MRI showed multiple supra-and intratentorial punctiform lesions in leptomeninges and “snowball” corpus callosum lesions (Fig. 1).
Brain MRI: 1: Axial. Diffusion with hyperintense punctiform lesions in relation to microinfarcts. 2: Sagittal, T2 Flair and T1 sagittal. Characteristic involvement of the corpus callosum. 3: Axial T2 Flair with contrast. hypersignal and leptomeningeal enhancement (additive signal T1 contrast + T2). 4: Axial T1 contrast with “military” uptake pattern.
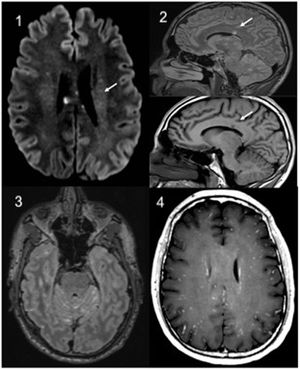
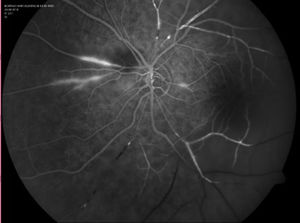
Treatment with steroids was initiated (initial dose: methylprednisolone 1 g/24 h/iv/for 7 days, later continued with 60 mg/24 h oral prednisone in a decreasing regimen) despite which he developed loss of visual acuity in both eyes, and ischaemic vascular occlusions were found on fluorescein angiography (FAG) (Fig. 2). In addition, audiometry showed bilateral sensory hearing loss (Fig. 3).
Susac syndrome (SS) was diagnosed given the clinical triad of encephalopathy, sensorineural hearing loss and retinal vasculitis with arterial occlusions. SS is an immune-mediated, pauci-inflammatory occlusive microvascular endotheliopathy that affects the brain, the retina, and the inner ear, first described in 1979.1,2 Characteristic are snowball-shaped T2-FLAIR lesions on MRI at the level of the corpus callosum and occlusive retinal vasculitis on FAG.3
The patient was treated with steroid boluses, rituximab, and acetylsalicylic acid and later, as there was no improvement, with immunoglobulins and mycophenolate,4 resulting in stabilisation of symptoms and then progressive reduction of steroid dose to 7.5 mg/24 h of prednisone after 9 months.
FundingThere was no source of funding.
Conflict of interestsThe authors declare that they have no conflict of interests.
AcknowledgmentIn gratitude to Dra. Miriam García Fernández from the Service of Ophthalmology of the Hospital Universitario Central of Asturias for the AFG images.
Please cite this article as: Suárez-Pérez L, Herrero Suárez SE, Peña Suárez J, Caminal-Montero L. Síndrome confusional y vasculitis retiniana. Reumatol Clin. 2021;17:52–54.