Osteoarthritis at the base of the thumb (CMC-1 OA) is a pathology that mainly affects postmenopausal women. The main symptoms including pain, decreased hand-thumb strength and fine motor capacity. Although a proprioceptive deficit has already been demonstrated in people with CMC-1 OA, there is insufficient evidence regarding the effects of proprioceptive training. The main objective of this study is to determine the effectiveness of proprioceptive training in functional recovery.
Materials and methodsA total of 57 patients were included in the study, 29 in the control group and 28 in the experimental group. Both groups underwent the same basic intervention programme, but the experimental group included a proprioceptive training protocol. Variables of the study were pain (VAS), perception of occupational performance (COMP), sense position (SP) and force sensation (FS).
ResultsStatistically significant improvement was observed in the experimental group in pain (p < .05) and occupational performance (p < .001) after 3 months of treatment. No statistical differences were found in sense position (SP) or sensation of force (FS).
Discussion and conclusionsThe results concord with previous studies focussing on proprioception training. The incorporation of a proprioceptive exercise protocol reduces pain and significantly improves occupational performance.
La osteoartritis de la base del primer metacarpiano (OA CMC-1) es una patología que afecta mayormente a mujeres postmenopáusicas. Los síntomas principales que acompañan esta patología son el dolor, la pérdida de fuerza y la disminución de capacidad motora fina. A pesar de que se ha demostrado un déficit propioceptivo en personas con OA CMC-1, no hay evidencia suficiente sobre los efectos del trabajo propioceptivo. El objetivo de este estudio es determinar la efectividad del entrenamiento propioceptivo en la recuperación funcional.
Materiales y métodosSe incluyeron un total de 57 pacientes, 29 del grupo control y 28 en el experimental. Ambos grupos llevaron a cabo el programa de intervención, y al grupo experimental se le incluyó además un protocolo de trabajo propioceptivo. Las variables de estudio fueron el dolor (EVA), percepción del desempeño ocupacional (COMP), sensación de posición (SP) y sensación de fuerza (SF).
ResultadosSe observó una mejora estadísticamente significativa en el grupo experimental en el dolor (p < 0.05) y el desempeño ocupacional (p < 0,001) a los 3 meses de tratamiento. No se encontraron diferencias estadísticas en la sensación de posición (SP) y la sensación de fuerza (FS).
Discusión y conclusionesLa correlación de nuestros resultados y los de estudios precedentes en cuanto a la efectividad del entrenamiento propioceptivo sobre las variables de estudio nos permite afirmar que la incorporación de un protocolo de ejercicios propioceptivos disminuye el dolor y mejora notablemente el desempeño ocupacional.
The anatomical complexity of the carpometacarpal joint of the thumb (CMC-1) makes it susceptible to instability and osteoarthritis.1 Osteoarthritis (OA) CMC-1 is more common in postmenopausal women.2,3 The main symptoms are pain and inflammation, which have a negative influence on the performance of everyday activities, leading to a loss of functionality.1–3 The factors which directly affect the execution of activities include the loss of grasping force,4,5 hand grasping6 and a reduction in fine motor capacity.3
Neuromuscular control and the mechanoreceptors in the ligaments and tendons play a highly important role in muscle action and thumb stability.7 Nevertheless, the role of proprioception of the thumb has yet to be fully explored.8 The term proprioception, which derives from the Latin “proprius” (belonging to oneself) and “-ception” (that which perceives), was first defined by Sherrington in 1906 as the bodily sensations which contribute to the perception of muscle activity, postural balance and joint stability.9 Previous studies7,10–12 have shown that individuals with CMC-1 OA are at higher risk of suffering proprioceptive deficits in this joint in comparison with healthy people. This proprioception disorder may be associated with pain, fatigue, soft tissue damage, changes in the cortical perception of the thumb and/or desensitization of the nervous system, as has been proven in studies of the shoulder.13 These factors may contribute to worsening of CMC-1 OA.
This study is based on the hypothesis that proprioceptive training in the conservative treatment of CMC-1 OA has positive effects on functionality and on the pain perceived by patients and, definitively, that it improves the occupational performance of individuals with arthrosis in the base of the thumb. The general objective of this study was to detect the effect of proprioceptive training of the thumb, based on the perception of movement (Joint Position Sense),10 the perception of force (Force Sense)14 and functional recovery.
Material and methodsStudy designA non-blind simply randomized multicentre clinical trial with the participation of the Clínica Universitaria Reina Fabiola, Cordoba (Argentina) and the Centro Tecan, in Malaga (Spain). All of the participants signed an informed consent document and the procedure followed the recommendations of the Helsinki Declaration.15 This study was approved by the Ethics Committee for Research in Human Beings (CIEIS).
ParticipantsAll of the participants were legally of age and diagnosed with grade I, II or III arthrosis in the base of the thumb according to the classification by Eaton and Littler.16 The participants were included in the study consecutively and did not know whether they were in the control group or the experimental group. Data confidentiality was ensured at all times.
Inclusion criteriaPatients legally of age with a previous diagnosis by a doctor of Eaton grade I, II or III arthrosis in the base of the thumb, who signed the informed consent document and accepted taking part in the study.
Exclusion criteria- -
Previous surgery in the hand or wrist.
- -
Neurological disorders.
- -
A previous diagnosis of OA at the level of the wrist and/or carpal joints.
- -
Rheumatoid arthritis or any other bone or joint pathology which may influence the function of the thumb studied.
- -
Having been treated conservatively for OA in the previous 6 months, including infiltrations (steroids and/or hyaluronic acid).
- -
Cognitive alterations that affect comprehension of the procedure and/or home exercises.
- -
Individuals with a visual disorder (blindness).
- -
Refusal to sign the informed consent document.
The sample size was determined using ENE3.0 software (GlaxoSmithKline©, Universidad Autónoma, Barcelona). Calculations were based on detecting an average difference of 2 cm in the minimum clinically important difference (MCID) in a Numerical Rating Scale (NRS) of 10 cm, with a standard deviation of 2 cm, a two-tailed test, an alpha level of 0.05 and a desired statistical power of 80 %. The size of the estimated desired sample is 15 individuals per group. A total of 28 participants were included in the control group and 29 were included in the experimental group.
InterventionThe patients were assigned at random according to their order of arrival in the experimental or control groups. The evaluation criteria and data gathering methods were stipulated and agreed previously by the participating centres. The variables were recorded by a hand therapist in each centre. The demographic and study variables were recorded and the data were entered in SPSS Statistics for subsequent analysis, assigning a number to each participant to ensure their anonymity at all times.
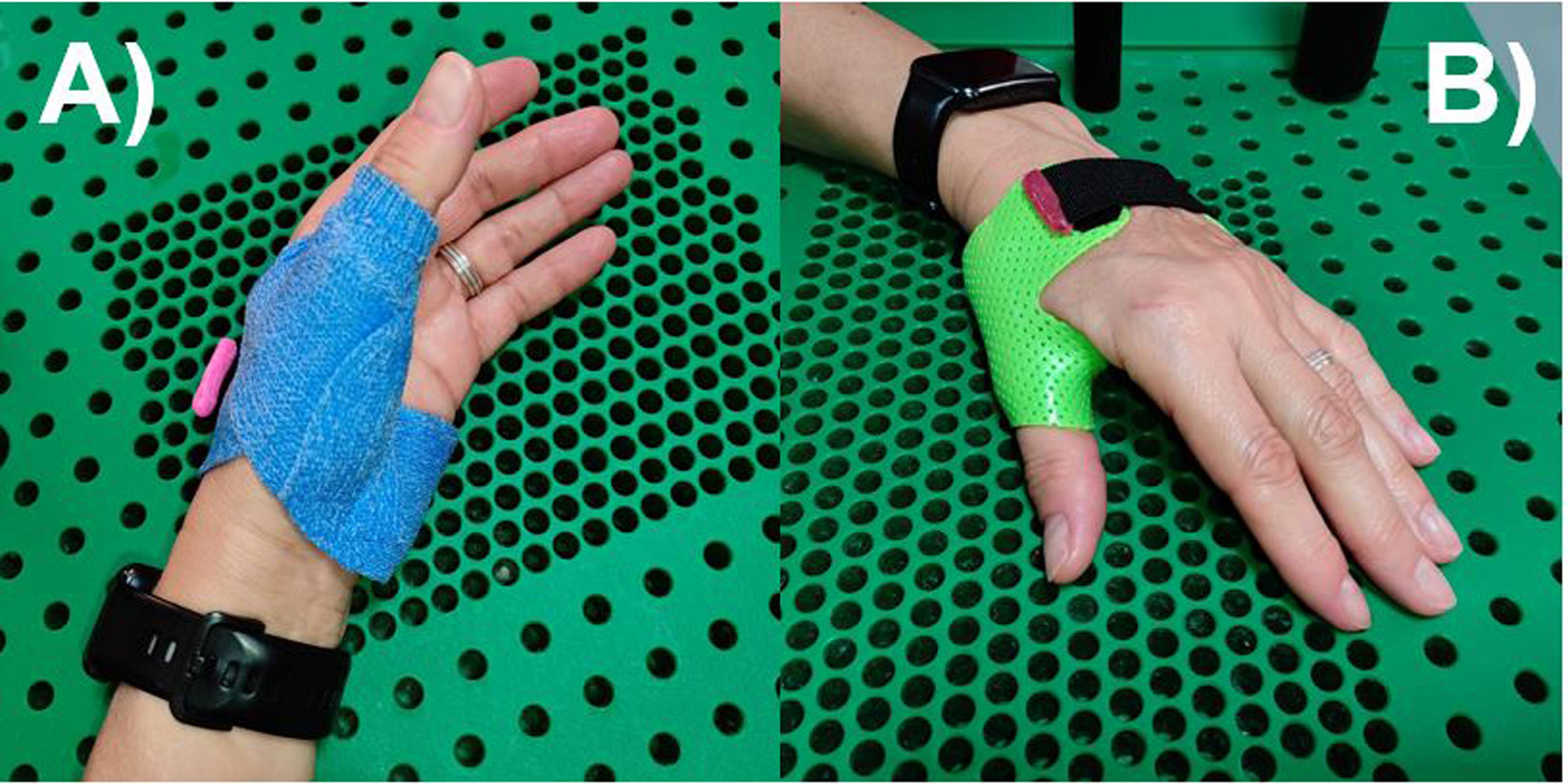
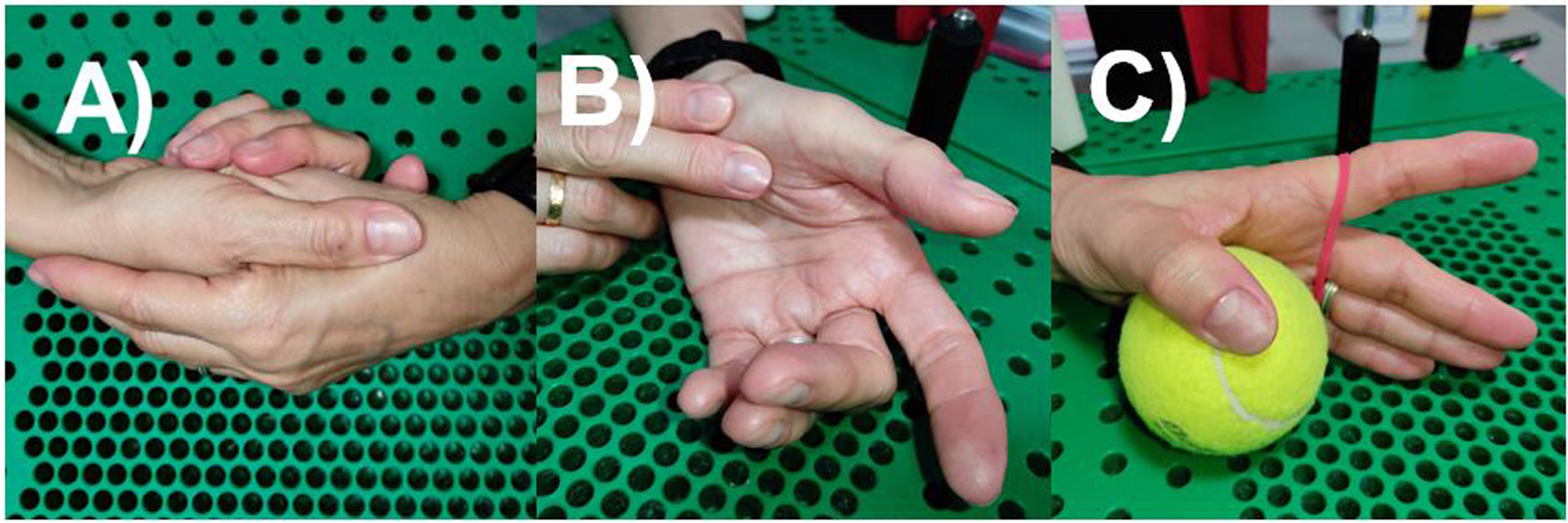
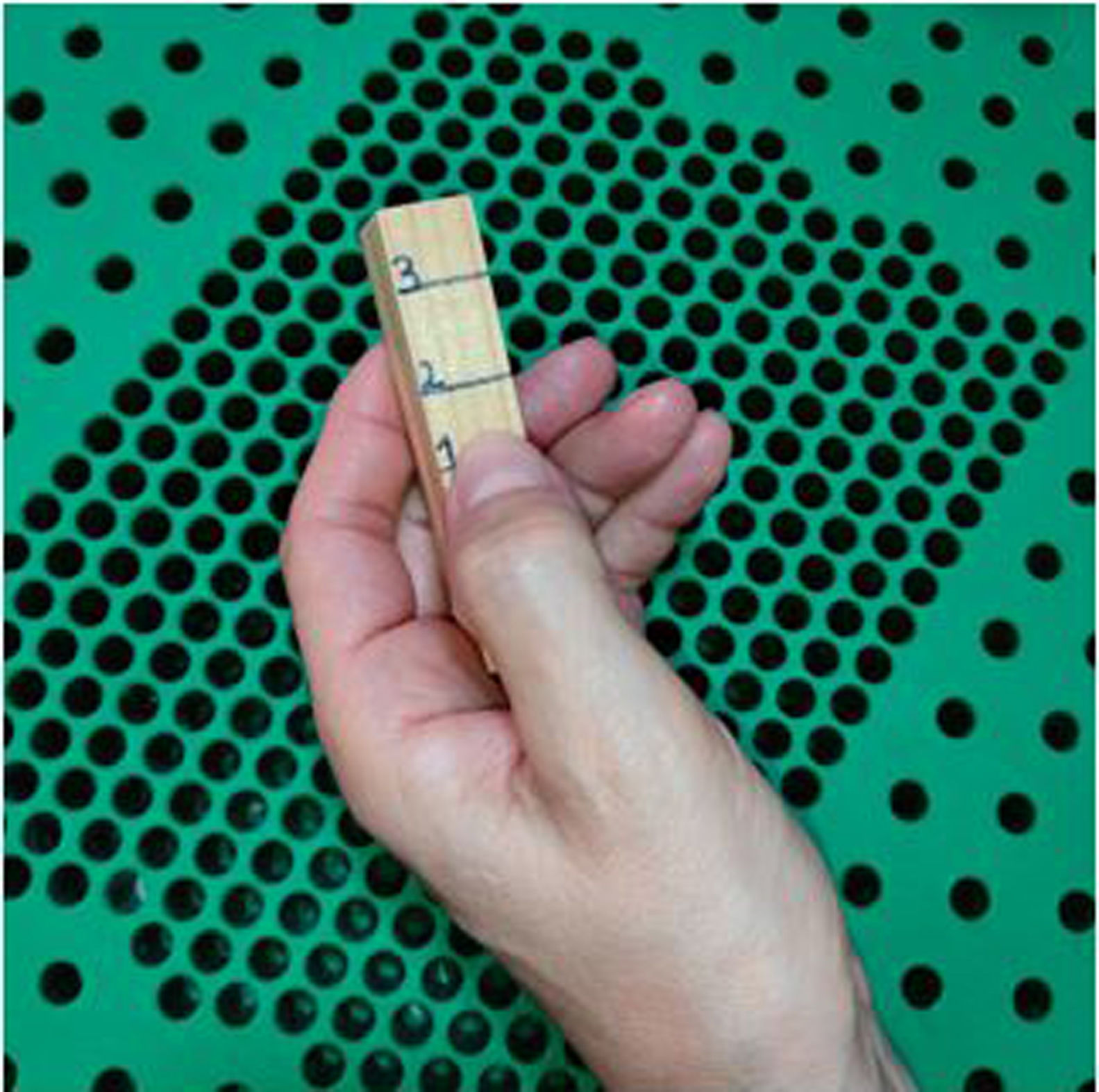
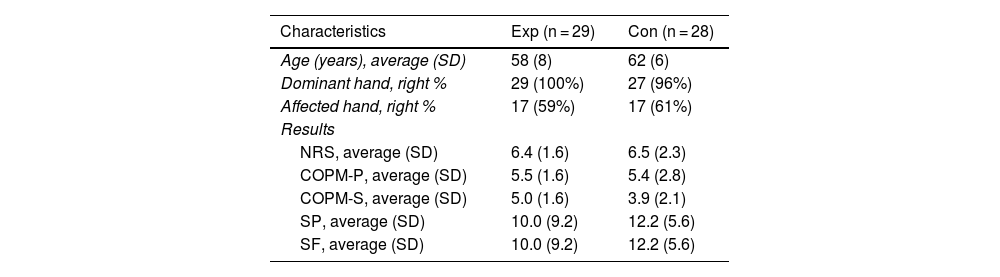
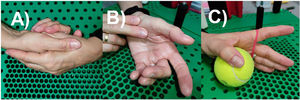
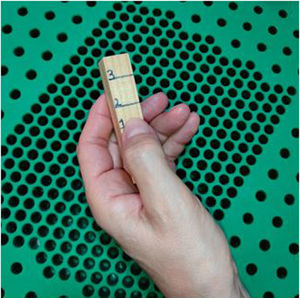
Both groups received an intervention programme based on the use of an orthosis (Fig. 1) and an exercise programme to free and strengthen the joint (Fig. 2). As well as the said exercises, the experimental group also had a specific programme for home proprioceptive exercises17 (Fig. 3) which consisted of reproducing the active movements of the thumb joints in different planes. This protocol was applied during 4 weeks, in which the patients attended the surgery twice a week. On the other days the patients carried out the same exercises in their home. The conservative treatment and the proprioceptive exercises had been demonstrated beforehand in the centre by the hand therapist, to ensure that all of the exercises were comprehended and executed correctly.
The different study variables were measured prior to the intervention (basal), after 4 weeks and after 12 weeks of follow-up by the hand therapist in each centre.
The Numerical Rating Scale (NRS)18 was used to evaluate pain, asking the patient to assess the level of pain from 0 to 10 (understanding 0 to be the absence of pain and 10 to be extreme pain).
Proprioception was evaluated in terms of the sensation of position using the Joint Position Sense Test14 and the sensation of force was evaluated using the Force Sense Test.10 To evaluate the sensation of position (SP) the patient was placed in an initial position with 30 ° thumb abduction, after which they were requested to actively reproduce the same position with their eyes closed. The difference in degrees between both measurements is the datum that was used in the statistical analysis. A digital dynamometer was used to evaluate the sensation of force (SF), and the patient was asked to form a key grip during 3 s, repeating the procedure 3 times with a 1 min. rest between each measurement.
The Canadian Occupational Performance Measure [COPM]19,20 was used to assess functionality. This scale gives two scores—Performance (P) and Satisfaction (S)—in 3 areas: self-care, productivity and leisure. A semi-structured interview was used to measure individual problematic areas identified by the patients in their everyday functioning.
Statistical analysisData were analysed using SPSS Statistics. The results were expressed as averages, standard deviations and/or 95% confidence intervals. The Kolmogorov–Smirnov test was used to show normal data distribution. The ANOVA test was used for variance analysis to compare the difference between the groups and the effects of the intervention on the study variables over time.
Post-hoc comparisons were made using Bonferroni corrections. The sizes of the effect between groups were calculated using Cohen’s d coefficient, considering an effect size: greater than 0.8, large; 0.5, moderate; and less than 0.2, small. The statistical analysis was undertaken with a 95% confidence interval, and P < .05 was considered to be statistically significant.
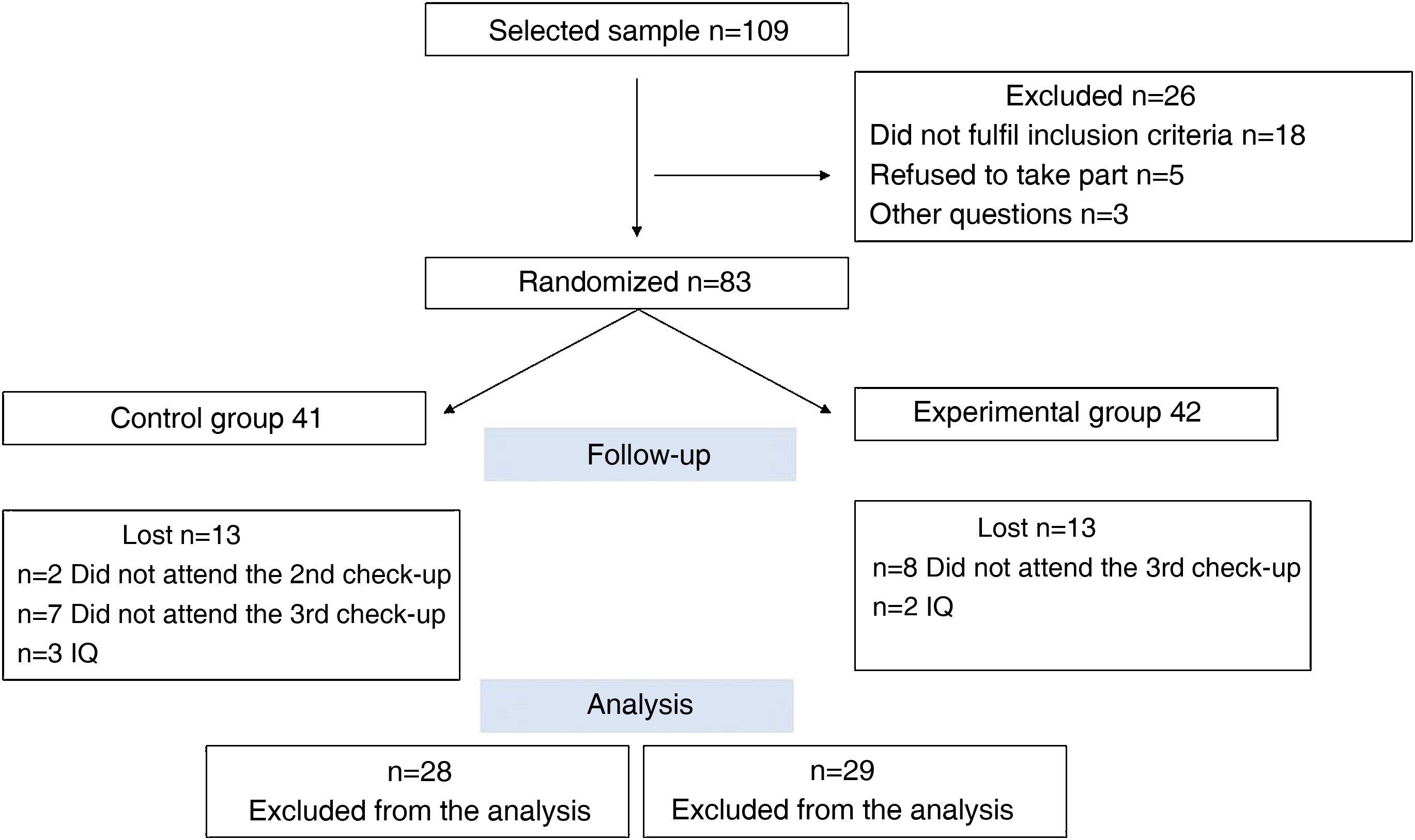
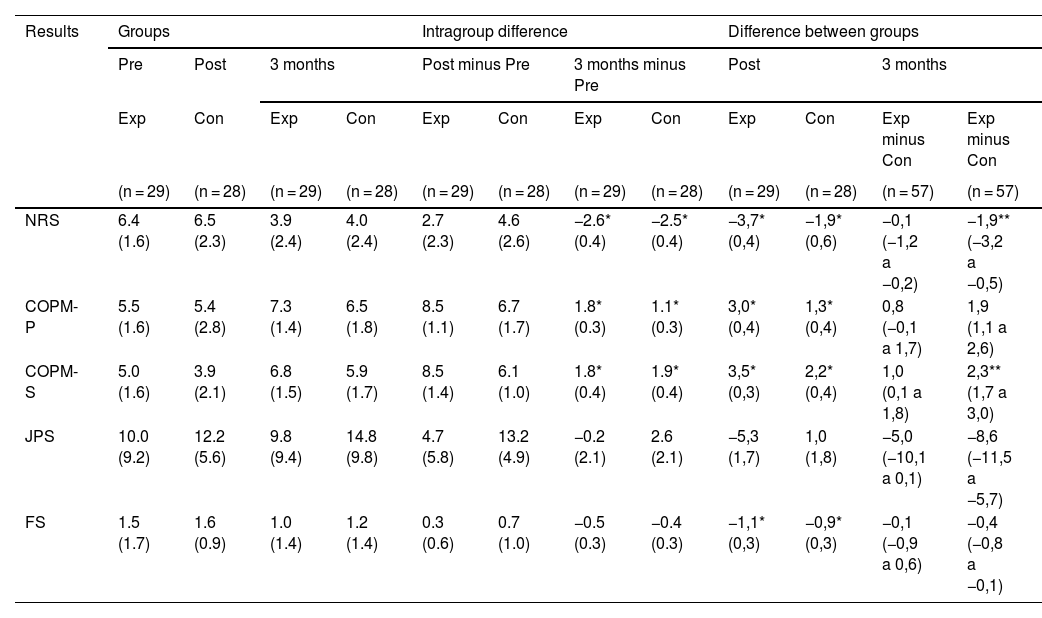
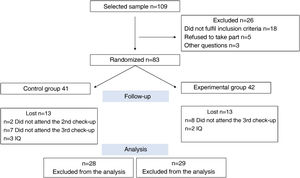
ResultsParticipants109 participants were included at first, 83 of whom were allocated at random to the control or experimental group. Finally, 57 patients (with an average age ± SD: 60 ± 7 years) fulfilled the inclusion criteria and were consecutively assigned at random to the experimental group (29) or the control group (28). The basal characteristics of the patients in each group are shown in Table 1 and the first two columns of Table 2. The flow diagram CONSORT was used to structure the progress of the patients during the different phases of the study (Fig. 4).
Basal characteristics of the participants.
| Characteristics | Exp (n = 29) | Con (n = 28) |
|---|---|---|
| Age (years), average (SD) | 58 (8) | 62 (6) |
| Dominant hand, right % | 29 (100%) | 27 (96%) |
| Affected hand, right % | 17 (59%) | 17 (61%) |
| Results | ||
| NRS, average (SD) | 6.4 (1.6) | 6.5 (2.3) |
| COPM-P, average (SD) | 5.5 (1.6) | 5.4 (2.8) |
| COPM-S, average (SD) | 5.0 (1.6) | 3.9 (2.1) |
| SP, average (SD) | 10.0 (9.2) | 12.2 (5.6) |
| SF, average (SD) | 10.0 (9.2) | 12.2 (5.6) |
With: Control group; COPM: Canadian Occupational Performance Measure; COPM-P: performance subscale; COPM-S: satisfaction subscale; Exp: experimental group; NRS: Numerical Rating Scale; SF: sensation of force; SP: sensation of position.
Intensity of pain (NRS), occupational performance (COPM-P and COPM-S), sensation of position (SP) and sensation of force (SF). Average (SD) for the results of each measurement in both groups, average (SD) for intragroup differences, average (SD) for differences between the groups and average (CI 95%) for differences between the groups.
| Results | Groups | Intragroup difference | Difference between groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 3 months | Post minus Pre | 3 months minus Pre | Post | 3 months | ||||||
| Exp | Con | Exp | Con | Exp | Con | Exp | Con | Exp | Con | Exp minus Con | Exp minus Con | |
| (n = 29) | (n = 28) | (n = 29) | (n = 28) | (n = 29) | (n = 28) | (n = 29) | (n = 28) | (n = 29) | (n = 28) | (n = 57) | (n = 57) | |
| NRS | 6.4 (1.6) | 6.5 (2.3) | 3.9 (2.4) | 4.0 (2.4) | 2.7 (2.3) | 4.6 (2.6) | −2.6* (0.4) | −2.5* (0.4) | −3,7* (0,4) | −1,9* (0,6) | −0,1 (−1,2 a −0,2) | −1,9** (−3,2 a −0,5) |
| COPM-P | 5.5 (1.6) | 5.4 (2.8) | 7.3 (1.4) | 6.5 (1.8) | 8.5 (1.1) | 6.7 (1.7) | 1.8* (0.3) | 1.1* (0.3) | 3,0* (0,4) | 1,3* (0,4) | 0,8 (−0,1 a 1,7) | 1,9 (1,1 a 2,6) |
| COPM-S | 5.0 (1.6) | 3.9 (2.1) | 6.8 (1.5) | 5.9 (1.7) | 8.5 (1.4) | 6.1 (1.0) | 1.8* (0.4) | 1.9* (0.4) | 3,5* (0,3) | 2,2* (0,4) | 1,0 (0,1 a 1,8) | 2,3** (1,7 a 3,0) |
| JPS | 10.0 (9.2) | 12.2 (5.6) | 9.8 (9.4) | 14.8 (9.8) | 4.7 (5.8) | 13.2 (4.9) | −0.2 (2.1) | 2.6 (2.1) | −5,3 (1,7) | 1,0 (1,8) | −5,0 (−10,1 a 0,1) | −8,6 (−11,5 a −5,7) |
| FS | 1.5 (1.7) | 1.6 (0.9) | 1.0 (1.4) | 1.2 (1.4) | 0.3 (0.6) | 0.7 (1.0) | −0.5 (0.3) | −0.4 (0.3) | −1,1* (0,3) | −0,9* (0,3) | −0,1 (−0,9 a 0,6) | −0,4 (−0,8 a −0,1) |
With: Control group; COPM: Canadian Occupational Performance Measure; COPM-P: performance subscale; COPM-S: satisfaction subscale; Exp: experimental group; NRS: Numerical Rating Scale; SF: sensation of force; SP: sensation of position.
A statistically significant reduction in pain was obtained in both groups one month after the intervention (experimental group average, 3.9; CI 95%: 3.4; 1.7; control group average, 4.0; CI 95%: 3.5; 1.6; P < .001; there was no significant difference in the magnitude of the effect between both groups −0.1; CI 95%: −1.2; −0.2, P > .05) and at 3 months (experimental group average, 2.7; CI 95%: 4.8; 2.7; control group average, 4.6; CI 95%: 3.0; 0.9; P < .001; significant difference between the groups −1.9; CI 95%: −3.2; −0.5, P < .05) (Table 2). The magnitude of the effect between the groups was small (d = 0.4) after one month, and moderate (d = 0.8) after 3 months.
Performance and satisfactionThe results for COPM-P and COPM-S showed a statistically significant difference over time (F = 52.281 at 76.443, both with P < .001). Post-hoc analysis showed a significant improvement in COPM-P as well as in COPM-S in both groups after the intervention in comparison with the basal data and data after one month of follow-up (both, P < .001) and after 3 months (both, P < .03), with a statistically significant difference after one month and after 3 months (2.3; CI 95%: 1.7; 3.0, P < .001) in COPM-S (Table 2).
Sensation of positionANOVA analysis did not reveal a significant effect over time (F = 2.705; P = .07). The magnitude of the effect between the groups was d = 1.9 and 1.6 after 3 months follow-up (Table 2).
Sensation of forceThe results for FS (the sensation of force) showed a statistically significant difference between the averages over time (F = 12.274 P < .001). Post-hoc analysis of the intragroup difference revealed an important fall in the scores and therefore an improvement in the sensation of force (FS) in both groups after 3 months of treatment compared with the basal data (P < .02). Nevertheless, this difference was not statistically significant either between the groups or after one or three months after the intervention (Table 2).
DiscussionThe purpose of this study was to determine the effect of a specific proprioceptive programme on the functional recovery of patients with CMC-1 OA during a period of 3 months.
Pain is one of the main reasons why patients go to rehabilitation departments, as it strongly limits functionality.21 Sufficient evidence supports the efficacy of conservative treatment in CMC-1 OA, and the majority of these treatments seek approaches that help to reduce pain.22–25
According to our results, both groups reported a significant improvement in pain at one month after the intervention, so that it is not possible to directly link this improvement to the proprioceptive training. Nevertheless, after 3 months the magnitude of the effect in both groups differed more, as the experimental group showed better results for the pain variable. This agrees with the results of previous studies,26–28 which concluded that proprioceptive exercises produce an improvement in pain intensity for patients with CMC-1 OA. However, we should be cautious here due to the wide range of circumstances that may have a positive effect on pain, including the placebo effect.
In the light of these results, we believe it to be highly important to determine whether this positive effect on pain is maintained over time, so that it would be advisable to apply a follow-up period of at least from 6 to 12 months.
Patients who suffer CMC-1 OA find it difficult to perform everyday activities. The Canadian Occupational Performance Measure (COPM) is an instrument which has been shown to be a good option for evaluating OA patient perception and their satisfaction in different occupational areas (self-care, productivity and leisure).29 We obtained statistically significant results in terms of improved perception and satisfaction with occupational performance after one month and 3 months of follow-up. The proprioceptive exercise programme may therefore help to improve patient perceptions of how they perform their everyday activities. This difference between the groups may be due to several factors, including the possibility that proprioceptive exercises involve performing movements commonly used in everyday activities, so that they may help to improve how they are performed. Nevertheless, we are not aware of the effect that this may have over the long-term, so that it would be appropriate to undertake studies to determine whether this effect is maintained even when patients cease to participate in the proprioceptive exercise programme.
Respecting proprioception, the Joint Position Sense Test (JPST) was used to measure SP.10,22,28 Its results showed no significant differences, unlike the results of previous studies.27 It is possible that SP does not specifically evaluate proprioception in its broadest sense. It is important to consider SF in how patients with CMC-1 OA evolve, although our results do not suggest that proprioceptive exercises lead to a direct improvement of this variable.
ConclusionThe patients with CMC-1 OA who followed a conservative protocol improved over time in terms of pain and their perception and satisfaction with performance and in the proprioceptive components (SP and SF). Implementing a programme of proprioceptive exercises seems to have positive effect on the functional recovery of patients with CMC-1 OA, with a reduction in pain and improvements in occupational performance after 3 months. We do not know the long-term effects or possible placebo effect that the intervention in itself may have.
FinancingFinancing for open publication from the Universidad de Malaga/CBUA.
Conflict of interestsThe authors have no conflict of interests to declare.