Haglund's syndrome produces posterior impingement of the heel, which is caused by a posterosuperior calcaneal exostosis, known as Haglund's deformity, associated with Achilles tendinitis and retrocalcaneal bursitis. Its pathogenesis is unknown. We report two cases that were diagnosed clinically and confirmed radiographically. One patient was treated conservatively and the other underwent surgery. The diagnosis is based on clinical signs and radiological images, using the measurement of the parallel pitch lines, in a lateral radiograph of the ankle. Initial treatment is usually conservative and includes anti-inflammatory or analgesic agents, physiotherapy and low-heeled, open-heeled shoes. If conservative treatment does not relieve the pain, surgery may be necessary.
El síndrome de Haglund es una causa de atrapamiento tendino-bursal posterior del talón, producida por una exostosis posterosuperior del calcáneo, denominada deformidad de Haglund, asociada a tendinitis aquílea y bursitis retrocalcánea. Su patogenia es desconocida. Se presentan 2 casos, diagnosticados clínicamente, confirmados radiológicamente, y tratados conservadoramente uno y con cirugía el otro. El diagnóstico se realiza por la clínica y por las imágenes radiológicas con el método de medición de las líneas de inclinación paralelas, en una radiografía lateral del tobillo. El tratamiento inicial suele ser conservador e incluye antiinflamatorios o analgésicos, fisioterapia y zapatos con talón abierto y sin tacón alto. Si el tratamiento conservador no alivia el dolor, puede ser necesaria la cirugía.
Haglund's syndrome was described for the first time in 1928 by Patrick Haglund. It is a cause of tendino-bursitis entrapment of the heel, produced by a posterosuperior exostosis of the calcaneus (Haglund's deformity), accompanied by Achilles tendinitis and retrocalcaneal bursitis.1–3
Although its pathogenesis is unknown, there have been reports proposing predisposing mechanical factors such as shoes that are too tight, high heels worn by women, an increased plantar arch, Achilles tendon too tense and situations that increase friction between the tendon and the bone.2
The differential diagnosis should include xanthomatosis, seronegative spondyloarthropathies and gouty and rheumatoid arthritis.2,3
Clinical ObservationCase 1The patient was a 37-year-old woman with a 10-month history of pain located in the Achilles region of right foot, which became more intense with activity. The physical examination revealed the thickening of the Achilles tendon with pain on palpation, the stability of ankle and foot joints was conserved, and the Thompson test was negative. A lateral radiograph of the ankle revealed swelling of the soft tissue of the distal third of the Achilles tendon and a posterosuperior prominence of the calcaneus. Ultrasound showed a hypoechoic Achilles tendon, calcification at its insertion into the calcaneus and hypoechoic images of the Kager fat pad. The symptoms disappeared after physical therapy.
Case 2The patient was a 62-year-old woman who had been treated surgically for Haglund's syndrome with retrocalcaneal bursitis and osteotomy of Haglund's deformity. Five months after the intervention, she came to our clinic with little improvement in the symptoms. She presented with inflammation and pain in the distal third of the Achilles tendon, difficulty in dorsiflexion of the ankle and claudication. The symptoms partially remitted after physiotherapy.
DiscussionHaglund's syndrome is a cause for mechanical pain in the hindfoot. There are several theories about its pathogenesis, although some authors point out the continuous contraction of the sural triceps, which produces an entrapment of the Achilles tendon and the retrocalcaneal bursa against the posterosuperior calcaneal exostosis.4 Other authors propose that the process begins with an external compression on the heel, which applies pressure to the retrocalcaneal bursa, which then presses on the outer part of the calcaneus. Thus, the calcaneal tuberosity increases in size in response to this chronic irritation, and the tuberosity, in turn, compresses the bursa and the Achilles tendon, provoking a vicious circle.2,5
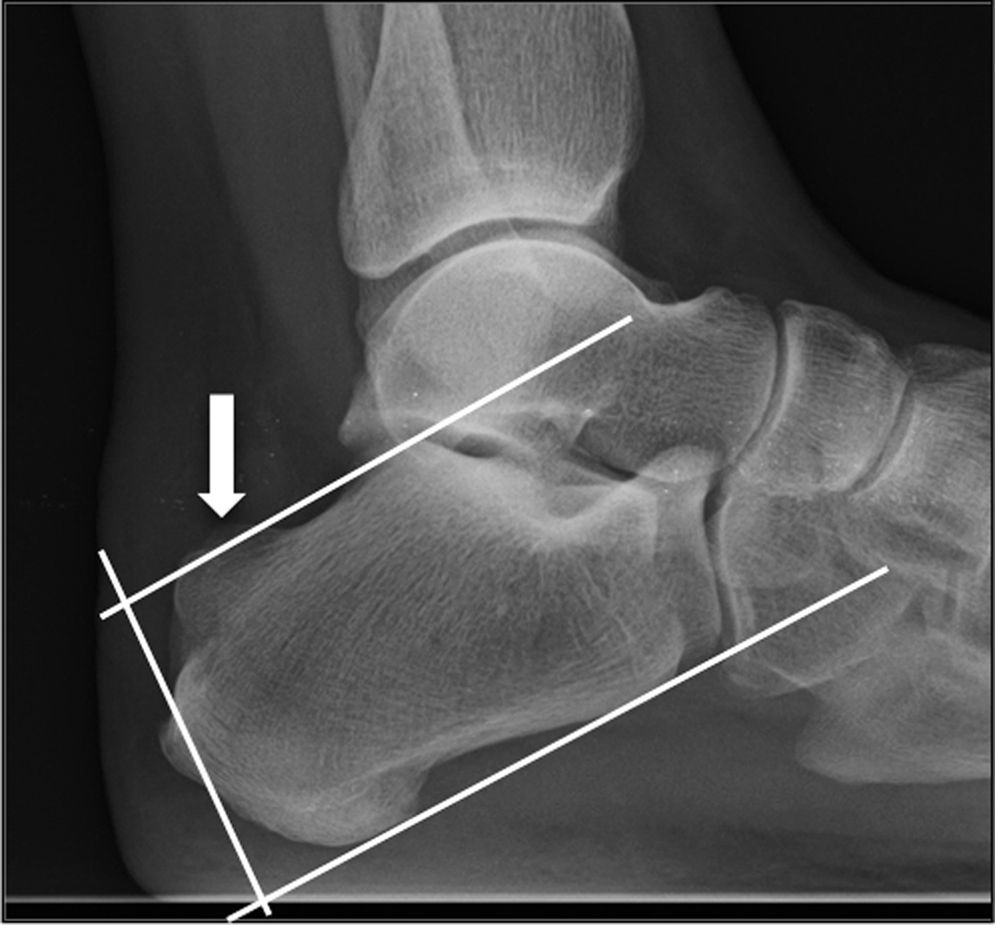
The diagnosis is reached on the basis of the clinical signs and radiological images using the measurement of the parallel pitch lines (PPL) in a lateral radiograph of the ankle. This method consists in tracing a line tangent to the lower margin of the calcaneus, and another parallel to the first on the upper margin, at the height of the highest point of the posterior margin of the subtalar joint surface. If the tuberosity exceeds this line, the cause is considered to be Haglund's deformity (Fig. 1).2,5 In some cases, the diagnosis can be completed using ultrasound or magnetic resonance imaging.2,6
The initial treatment should be conservative, with the avoidance of shoes that are too tight or have a high heel, using foot orthoses, oral anti-inflammatory drugs, local corticosteroid injection and physiotherapy.3,7 If there is no response to conservative treatment, surgery would be indicated. The technique most frequently used is retrocalcaneal bursectomy with osteotomy of Haglund's deformity, as the central approach to the tendon has been found to be safe and effective.7–10
ConclusionHaglund's syndrome is a cause of pain in the hindfoot that should be taken into account in the differential diagnosis. It should be suspected in the light of the clinical characteristic finding, and be confirmed by radiological studies to ensure a correct diagnosis. Conservative treatment involving medical and physical therapy should be the first option before surgery.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Jiménez Martín F, Alonso Valdazo MD, Díaz Peña G, Fernández Leroy J, Hernández Herrero D, Díaz García F. Síndrome de Haglund. A propósito de 2 casos. Reumatol Clin. 2017;13:37–38.