In recent decades the treatment of rheumatoid arthritis (RA) has improved thanks to the use of highly effective drugs. However, patients usually require long term therapy, which is not free of side effects. Therefore RA patients often demand complementary medicine, they seek additional sources of relief and/or less side effects. In fact 30–60% of rheumatic patients use some form of complementary medicine. Therefore, from conventional medicine, if we want to optimally treat our patients facilitating communication with them we must know the most commonly used complementary medicines. The aim of this review is to assess, based on published scientific research, what complementary therapies commonly used by patients with RA are effective and safe.
En las últimas décadas el tratamiento de la Artritis Reumatoide (AR) ha mejorado mucho gracias a la utilización de fármacos altamente eficaces. Sin embargo, los enfermos suelen requerir tratamiento farmacológico de por vida, no exento de efectos adversos. Por esta razón los pacientes con AR a menudo acuden a la medicina complementaria, buscan fuentes adicionales de alivio y/o menores efectos secundarios. Un 30–60% de los pacientes reumáticos utilizan algún tipo de medicina complementaria. Por lo tanto, desde la medicina convencional, si queremos optimizar el tratamiento de nuestros pacientes y facilitar la comunicación con ellos debemos conocer las medicinas complementarias más utilizadas. El objetivo de esta revisión es valorar, en base a la investigación científica publicada, qué tratamientos complementarios habitualmente utilizados por los pacientes con AR son efectivos y seguros.
Recent advances have improved drug treatment of rheumatoid arthritis (RA). Despite this fact, most RA patients need lifelong pharmacological therapy. An increasing number of RA patients are resorting to various complementary and alternative medicine (CAM) approaches for relief of symptoms and general well-being. CAM is the term for medical products and practices that are not part of standard care and are not generally taught in conventional medical schools. Alternative medicine is used instead of conventional medicine, whereas complementary medicine is used together with it. CAM has been mainly used to treat back pain or other back problems, neck pain, joint pain or stiffness and anxiety or depression in RA patients.1 For this reason, rheumatologists should be aware of CAM when treating RA patients.
The American College of Rheumatology (ACR) recognizes the interest in CAM approaches in the Position Statement Document. “The ACR supports rigorous scientific evaluation of all modalities that improve the treatment or rheumatic diseases. The ACR understands that certain characteristics of some CAMs and some conventional medical interventions make it difficult or impossible to conduct standard randomized controlled trials. For these modalities, innovative methods of evaluation are needed, as are measures and standards for the generation and interpretation of evidence. The ACR supports the integration of those modalities proven to be safe and effective by scientifically rigorous clinical trials published in the biomedical peer review literature. In the absence of such rigorous clinical trials, the ACR recommends advising patients that potential harm can occur from unproven or alternative therapies and thus advises caution in the use of unproven treatments. The ACR believes healthcare providers should be informed about the more common CAM modalities, based upon appropriate scientific evaluation as described above, and should be able to discuss them knowledgeably with patients”.2
This article provides an overview of the current body of knowledge about the role of CAM in the treatment of RA.
MethodsIn order to explore available evidence about CAM used in RA patients, we performed a systematic search including Medline and Cochrane library databases. Medline search was performed including the following appropriate combination of MeSH (Medical Subject Heading) terms including: “complementary therapies”, “diet”, “dietary supplements”, “phytotherapy”, “medicinal plants”, “exercise”, “mind-body therapies”, “acupuncture”, “homeopathy”, “hydrotherapy” AND “rheumatoid arthritis”. The references cited in the obtained papers were also examined to identify additional studies not indexed by MEDLINE.
NutritionNutritional interventionNutritional intervention has been used in patients with chronic inflammatory diseases. Specifically, nutritional intervention used in RA patients included: supervised fasting (200–300kcal/day) during 7–10 days, Mediterranean diet (small amount of meat, fish, more fruits and vegetables and olive oil), vegetarian diet, vegan diet, elemental diet (liquid diets that contain nutrients that are broken down to make digestion easier) and elimination diet (foods that are thought to be the cause of symptoms are eliminated, and then added one at a time to find which ones cause symptoms).
There is evidence that fasting produces a decrease in pain and inflammation in RA patients.3 However, the inflammation reappears when the patient starts his/her normal diet.4 It has been shown that fasting followed by a vegetarian diet may help patients with RA. The effect of fasting followed by a year of a vegetarian diet was assessed in a randomized, single-blind controlled trial.5 The diet group showed a significant improvement in the number of tender joints, Ritchie's articular index, number of swollen joints, pain score, duration of morning stiffness, grip strength, erythrocyte sedimentation rate, C-reactive protein, white blood cell count, and a health assessment questionnaire score (HAQ). These benefits in the diet group were still present after one year5 and this improvement can be sustained through an additional follow-up two-year diet period.6
A Mediterranean diet has been proved to reduce blood pressure; improve glucose metabolism, the lipid profile, and lipoprotein particle characteristics and decrease inflammation and oxidative stress.7 In RA patients, a Mediterranean diet decreases pain, morning stiffness, the number of swollen joints and also improves HAQ, Disease Activity Score 28 (DAS28) and disease patient perception.7 Three systematic reviews stated that a Mediterranean diet decreased pain in RA patients.8–10 Moreover, the Mediterranean diet has been recommended for cardiovascular diseases and osteoporosis (frequent RA comorbidities).
A Cochrane review8 assessed the effectiveness and safety of dietary interventions in the treatment of RA. The authors concluded that fasting, followed by 13 months on a vegetarian diet, may reduce pain. The effects of vegan and elimination diets are uncertain due to inadequate data reporting. Trials that studied elemental diets reported no significant differences in pain, function or stiffness.
Nutritional supplementsFish oilFish oil is rich in Ω-3 polyunsaturated fatty acids (PUFAs), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which have been associated with reduced expression of TNF-α and interleukin-1β.11,12 These properties are similar to synthetic drugs used in RA patients such as nonsteroidal anti-inflammatory drugs (NSAIDs) and TNF blockers. Furthermore, EPA and DHA can be metabolized in E-series and D-series of resolvins that reduce inflammation.13 The American Heart Association recommends consuming fish oil to reduce the occurrence of cardiovascular disease events in patients with coronary artery disease.14 RA patients present high cardiovascular morbid-mortality rate and fish oil consumption could represent an additional benefit in this population. A meta-analysis suggested that including omega-3 PUFAs at dosages >2.7g/day in the diet for >3 months reduces NSAID consumption in RA patients.15 A systematic review including 23 randomized controlled trials testing marine Ω-3 PUFAs has been performed in patients with RA. This review has showed a modest benefit on joint swelling and pain, duration of morning stiffness, global assessment of pain and disease activity, and a reduction in the use of NSAIDs.16
Proudman et al. studied in a randomized, double-blind controlled trial the effects of fish oil consumption in early RA, employing a ‘treat-to-target’ protocol in combination with disease-modifying anti-rheumatic drugs (DMARDs). Fish oil intake was associated with a higher rate of ACR remissions, and a reduction in DMARDs dosage.17
Although not necessarily clinically significant, when prescribing Ω-3 PUFAs, rheumatologist should be aware that high dose Ω-3 PUFAs are not recommended in patients who may be susceptible to increased bleeding (e.g., patients taking warfarin), because they may increase coagulation times.18
Virgin olive oilVirgin olive oil contains numerous compounds that exert potent anti-inflammatory and antioxidant actions.19 The main active components of olive oil include oleic acid, linolenic acid, alpha-linoleic acid and phenolic constituents.20,21 Oleic acid is metabolized to eicosatrienoic acid (omega-9 fatty acid) with similar anti-inflammatory properties than fish oil omega-3 fatty acids.21
Berbert et al. evaluated whether supplementation with olive oil could improve clinical and laboratory parameters of disease activity in RA patients who were already taking fish oil supplements. RA patient groups that received fish oil omega-3 fatty acids and olive oil showed a more precocious and accentuated improvement.22
Vitamin DVitamin D plays a role in the maintenance of the homeostasis of the calcium and phosphorus metabolism. Vitamin D deficiency is linked to osteopenia, which is frequently associated to RA. Nevertheless vitamin D functions go much further since it is considered an immune system regulator. It intervenes in the innate and acquired immune systems.23
In vitro, vitamin D inhibits the activation of IL-2, IL-12, IL-6, interferon gamma (IF-γ), and TNF. Instead, vitamin D promotes monocyte differentiation into macrophages. Moreover, vitamin D has anti-inflammatory qualities through its capacity to regulate the production of prostaglandins.24 In fact, in murine models of human arthritis, vitamin D inhibits the progression of arthritis.25
A meta-analysis summarizes published results on the association between vitamin D intake and the development of RA. The authors conclude that an insufficient vitamin D intake is associated with an elevated risk of RA development.26
Vitamin D supplements could have an effect on RA treatment. Brohult et al. studied the effects of large doses of calciferol on patients with RA in a double-blind clinical trial. After 1 year, high dose oral calciferol therapy showed a positive effect on disease activity in RA patients.27
Furthermore, in a 3-month open-label trial, vitamin D administration as an adjunct therapy with DMARDs was correlated with a decrease in pain and PCR in RA patients. No adverse reactions related to vitamin D were reported.28
ProbioticsProbiotics are live microorganisms that, when administered in adequate amounts, confer health benefits on the host.29 Current evidence suggests that probiotics may play a therapeutic role in chronic inflammatory diseases such as RA.30
In murine models of RA, oral administration of Lactobacillus casei decreased the pro-inflammatory cytokines and improved RA index disease activity in comparison with a control group or even compare with a control group treated with indomethacin.31 Furthermore, So et al. demonstrated that the administration of Lactobacillus casei improved histopathological changes, and the lymphocytic infiltrates in the joints, similarly to the administration of methotrexate (MTX).32
Several studies showed an improvement in HAQ or disease patient perception related to probiotics intake.33–36 However, the evidence of the use of probiotics in humans is scarce. A recently reported randomized, double-blind, clinical trial study showed beneficial effects of Lactobacillus casei in pain, tender and swollen joint counts and DAS28, in RA women patients. It also showed amelioration in PCR, TNFα, IL-12 e IL-10 levels.36 No side effects were described.
Herbal medicineSome herbal medicinal products have been shown to interact with the mediators of inflammation and, therefore, may be used in the treatment of RA.37,38 These products can also act as free radical scavengers, and through other mechanisms. For example, topical capsaicin is a highly selective agonist of TRPV1 receptors, which are expressed in afferent neuronal C fibers and some Aδ fibers. Capsaicin induces local depletion of substance P which is thought to be part of its mechanism for pain relief.39
However, few high quality clinical trials have yet been carried out to substantiate the safety and efficacy of herbal medicines, which are not free of potentially serious side effects.
Eleven randomized controlled trials including 940 patients have reported the effects of Tripterygium wilfordii extracts (TWE) in the treatment of RA; the methodological quality of these studies was generally low and the results have been inconsistent.40 A randomized controlled trial by Goldbach-Mansky et al., was conducted to compare the benefits and side effects of TWE with those of sulfasalazine for the treatment of active RA. The results showed that the attainment of the ACR 20 response criteria was significantly higher with TWE extract than with sulfasalazine.41 A multicenter, open-label, randomized controlled trial compared the efficacy and safety of TWE with MTX in the treatment of active RA. After 6 months, the proportion of patients reaching the ACR50 response criteria was 46.4%, 55.1% and 76.8%, respectively, in the MTX, TWE and MTX+TWE groups. The authors concluded that TWE monotherapy was not worse than MTX, and that MTX+TWE was better than MTX alone in controlling disease activity in patients with active RA.42
It has also been suggested that plants such as Borago officinalis, Oenothera blennis and Ribes migrum with a high grade of acid gamma linolenic (AGL) may improve pain and disease activity in RA patients.39 AGL is an essential fatty acid precursor of prostaglandin E1, an eicosanoid with anti-inflammatory and immunomodulatory properties.43 In clinical trials, the AGL group, developed more frequently adverse reactions than the placebo group, although no significant differences were reported. Cases of convulsions due to Oenothera blennis have been reported in epileptic patients or patients being treated with central nervous system medications.39
The quality of herbal medicines can directly affect their safety and efficacy. Good manufacturing practices (GMP) are one of the most important tools to avoid contamination of herbal products.44 If the manufacturer keeps GMP, this issue is rare.
Physical activityPhysical inactivity is the fourth leading risk factor for mortality.45 People who exercise more have lower rates of coronary heart disease, hypertension, stroke, type 2 diabetes, metabolic syndrome, colon cancer, breast cancer, depression and mortality from all causes.46 Physical activity decreases the risk of fracture and loss of bone mineral density and increases muscle mass, strength, power and intrinsic neuromuscular activity.46,47 However, in RA patients physical activity has been considered to increase joint stress, pain, disease activity and joint damage. Then, is it appropriate to recommend exercise to RA patients?
According to the latest evidence, exercise has not been associated with harmful effects on disease activity, pain or radiological damage.48,49 Therefore, physical activity does not worsen RA, and probably provides additional benefits.
Hurkmans et al. reviewed the effectiveness and safety of short-term (
In western countries, mind-body interventions, such as yoga, which combines stress management with physical activity, are growing. Yoga modulates sweating response to dynamic exercise and improves respiratory muscle strength, handgrip strength, handgrip endurance and flexibility.51–53
There is very low evidence of the role yoga plays in RA patients. The methodological quality of the studies is poor because of a lack of patient blindness. Two trials showed a significant improvement of DAS28 associated with yoga.54,55 In other studies, yoga improved pain, HAQ, balance and handgrip strength.54,56,57
Evans et al. aimed to assess the effects of a yoga program on health-related quality of life (HRQoL) for young adults with RA compared with a usual-care waitlist control group. The results of the study suggested that yoga is a feasible and safe complementary treatment for young people with RA, leading to HRQoL, pain, disability, fatigue, and mood benefits.58
No side effects were reported for yoga in RA patients.59
TaichiTai Chi is a Chinese martial art that combines meditation with slow, gentle, graceful movements, as well as, deep breathing and relaxation.60
Wang et al. conducted a systematic review of reports on the effects of Tai Chi over various chronic medical conditions. Nine randomized controlled trials, 23 non-randomized controlled studies, and 15 observational studies were included. Tai Chi appeared to have benefits and also appeared to be safe and effective in promoting balance control, flexibility, and cardiovascular fitness in older patients with chronic conditions.61 Thus Tai Chi may benefit RA patients who have limited strength, mobility and comorbidities (cardiovascular risk, osteoporosis and depression).60
Several reviews about the effect of Tai Chi in RA patients have been published, including a Cochrane Review.59,60,62–64 Tai Chi was associated with improvement in terms of RA disease activity. Although existing evidence remains limited and inconclusive. No adverse events were observed and Tai Chi does not exacerbate RA symptoms.64
MeditationMeditation incorporates a diverse range of techniques that helps to focus attention and bring a state of self-awareness and inner calm. Meditation may alleviate patients’ suffering associated with physical, psychosomatic and psychiatric disorders, it can even reduce cardiovascular risk factors.65 Meditation may improve pain,66 anxiety,67 depression in RA patients,68,69 and fibromyalgia.70
In a randomized, waitlist-controlled pilot study Pradhan et al. evaluated the effect of mindfulness meditation on depressive symptoms, psychological status, and disease activity in 63 RA patients. After 2 months, there were no statistically significant differences between groups in any outcomes. After 6 months, there was significant improvement in psychological distress (35% reduction) and well-being. However, the intervention had no impact on RA disease activity.71
AcupunctureAcupuncture is a traditional Chinese medicine where thin needles are inserted in specific points of the body to facilitate the recovery of health and to enhance well-being. The effectiveness or efficacy of acupuncture has been tested in randomized controlled trials with poor methodological standards.72
The mechanism of action in acupuncture is associated with an analgesic effect by interaction with endogen opioids and serotonin mediators. Mayer et al. reported that acupuncture analgesia was blocked after naloxone administration. These findings support the effect of acupuncture over endogenous opioids.73 A positron emission tomography study showed that acupuncture therapy evoked short-term increases in μ-opioid cerebral receptors binding potential.74 Despite these studies, the current evidence about decreased pain due to acupuncture in RA patients is scarce and non conclusive.75
Two studies involving a total of 84 people were included in a Cochrane review. One study used acupuncture and no significant differences between groups were observed.76 In the second study, using electroacupuncture, a significant decrease in knee pain was reported in the experimental group when compared to the placebo group. However, the authors concluded that the poor quality of the trial, including the small sample size preclude any recommendation.77
More recently, two systematic reviews reported that despite some favorable results in active-controlled trials, conflicting evidence exists in placebo-controlled trials concerning the efficacy of acupuncture for RA. Rigorous and well-controlled randomized trials are warranted. Minor adverse events in the acupuncture groups were observed.78–81
Another systematic review assessed the effect of bee venom acupuncture (BVA) used as an RA therapy. The authors concluded that the evidence is insufficient to suggest that BVA is an effective treatment for RA.82
HomeopathyIn 1978, the first study of homeopathy in RA patients was published. Ninety-five RA patients were randomized to receive acetylsalicylic acid or homeopathy. After 1 year of treatment, 42.6% patients of the homeopathy group and only 14.6% of the salicylate group continued. During the first year of the study, 33.4% patients of the homeopathy group and 85.4% in the salicylate group withdrew the study.83 Gibson et al. compared orthodox first-line anti-inflammatory treatment plus homeopathy with anti-inflammatory treatment plus an inert preparation. In the treatment group improvement in subjective pain, articular index, stiffness and grip strength were observed.84
In a 6-month double-blind trial, 44 RA patients were entered comparing homeopathy with a placebo. There was no statistically significant difference between groups.85 A randomized controlled trial by Fisher and Scott was conducted to study if homeopathy was effective in reducing the symptoms of joint inflammation in RA. The results of the trial showed no evidence that active homeopathy improves the symptoms of RA.86
Brien et al. sought to assess whether any benefits from complementary homeopathic treatment in patients with RA are due to the homeopathic consultation, homeopathic remedies or both. The authors concluded that homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits in RA.87 This publication has received several criticisms,88–90 mainly because the insufficient statistical power to detect differences between groups.
In conclusion, we have limited clinical trials with adequate methodology to assess the effectiveness of homeopathy in patients with RA. None of the published studies have reported side effects associated with homeopathic drugs.
Balneotherapy/HydrotherapyHydrotherapy/Balneotherapy involves the use of water in treatments and in the case of RA is considered the oldest therapy. The recuperative and healing properties of these therapies are based on their mechanic and thermal effects.91 The protracted application of heat, and the pressure exerted by the water carries impulses felt at the skin deeper into the body, where they are instrumental in stimulating the immune system, reducing stress, invigorating circulation and digestion, encouraging blood flow, lessening pain sensitivity and blocking the sympathetic nervous system.92
A Cochrane review assessed the effectiveness of balneotherapy for RA patients. Nine trials, representing 579 people were included. Most trials reported positive findings, but were methodologically flawed to some extent, and withdrawals due to adverse events were not reported.93 Another systematic review found evidence that aquatic exercise had small but statistically significant effects on pain relief and related outcomes in RA. However, due to the poor methodological quality of balneotherapy studies, we are unable to make any conclusion on the effects of this intervention.94
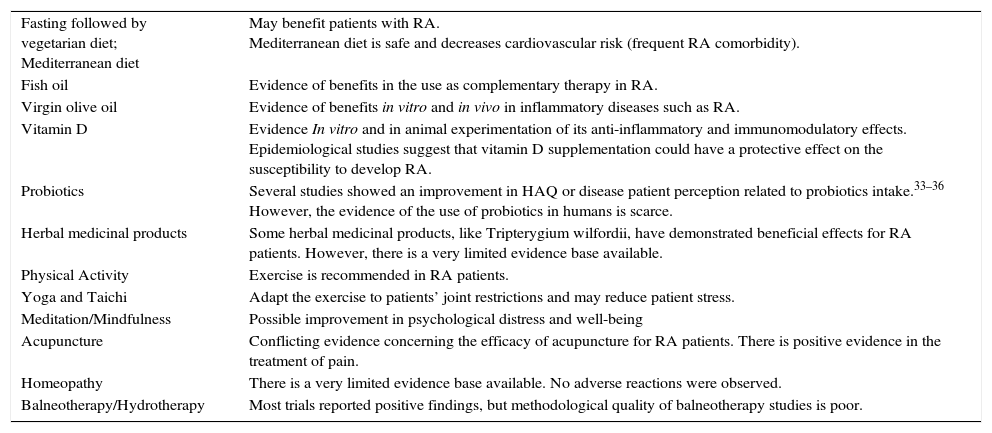
ConclusionThe use of CAM in rheumatology is common.95 The increased interest of RA patients in CAM approaches is a reality, thus rheumatologists should advice their patients with scientific rigor and the best evidence available. In this sense the ACR sets its position which supports rigorous scientific evaluation on all approaches that improve the treatment of rheumatic diseases.2Table 1 presents the CAM approaches that may be beneficial for RA patients, although there is still a long way ahead in terms of research in order to draw firm conclusions. There are no long-term studies, nor studies to assess joint damage progression, however some complementary therapies may represent an opportunity to improve the quality of life of our patients, and in the future may be integrated in the management of RA patients.
CAM modalities that may be beneficial for RA patients.
| Fasting followed by vegetarian diet; Mediterranean diet | May benefit patients with RA. Mediterranean diet is safe and decreases cardiovascular risk (frequent RA comorbidity). |
| Fish oil | Evidence of benefits in the use as complementary therapy in RA. |
| Virgin olive oil | Evidence of benefits in vitro and in vivo in inflammatory diseases such as RA. |
| Vitamin D | Evidence In vitro and in animal experimentation of its anti-inflammatory and immunomodulatory effects. Epidemiological studies suggest that vitamin D supplementation could have a protective effect on the susceptibility to develop RA. |
| Probiotics | Several studies showed an improvement in HAQ or disease patient perception related to probiotics intake.33–36 However, the evidence of the use of probiotics in humans is scarce. |
| Herbal medicinal products | Some herbal medicinal products, like Tripterygium wilfordii, have demonstrated beneficial effects for RA patients. However, there is a very limited evidence base available. |
| Physical Activity | Exercise is recommended in RA patients. |
| Yoga and Taichi | Adapt the exercise to patients’ joint restrictions and may reduce patient stress. |
| Meditation/Mindfulness | Possible improvement in psychological distress and well-being |
| Acupuncture | Conflicting evidence concerning the efficacy of acupuncture for RA patients. There is positive evidence in the treatment of pain. |
| Homeopathy | There is a very limited evidence base available. No adverse reactions were observed. |
| Balneotherapy/Hydrotherapy | Most trials reported positive findings, but methodological quality of balneotherapy studies is poor. |
The authors have no affiliations with or financial interest in any company or organization that could conflict with the views expressed in this manuscript.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this research has not been conducted experiments on humans or animals.
Confidentiality of dataThe authors declare that this article does not appear patient data.
Right to privacy and informed consentThe authors declare that this article does not appear patient data.