The aim of this study is to examine how gene mutation diversity and disease severity affect physical capacity and quality of life in children/adolescents with Familial Mediterranean Fever (FMF).
MethodsEighty children/adolescents (42 female, 38 male) diagnosed with FMF according to Tell-Hashomer diagnostic criteria were included in this study. Disease severity score (PRAS), running speed and agility and strength subtests of Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2 SF), Physical Activity Questionnaire, Pediatric Quality of Life Inventory 3.0 Arthritis Module (PedsQL) was used for evaluation. Participants were divided into 2 groups as M694V and other mutations according to MEFV gene mutation and were divided into 3 groups as mild, moderate and severe according to PRAS.
ResultsWhen the data were compared between groups; in terms of gene mutation, a significant difference was observed in treatment subtest of PedsQL-parent form in favor of the M694V gene mutation group (p<0.05). In terms of PRAS, significant difference was seen in the pain, treatment subtests and total score of the PedsQL-child form, and in the pain, treatment, worry subtests and total score of the PedsQL-parent form in favor of the mild group (p<0.05).
ConclusionsMEFV gene mutations in children and adolescents with FMF did not differ on physical capacity and quality of life. PRAS was not effective on physical parameters, but quality of life decreased as the severity score increased. Encouraging children/adolescents with FMF to participate in physical activity and to support them psychosocially can be important to improve their quality of life.
El objetivo de este estudio es examinar cómo la diversidad de mutaciones genéticas y la gravedad de la enfermedad afectan la capacidad física y la calidad de vida en niños/adolescentes con fiebre mediterránea familiar (FMF).
MétodosSe incluyeron en este estudio 80 niños/adolescentes (42 niñas y 36 niños) diagnosticados con FMF según los criterios diagnósticos de Tell-Hashomer. Disease Severity Score (PRAS), running speed and agility and strength subtests of Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2 SF), Physical Activity Questionnaire, Pediatric Quality of Life Inventory 3.0 Arthritis Module (PedsQL) se utilizó para la evaluación. Los participantes se dividieron en 2 grupos como M694V y otras mutaciones según la mutación del gen MEFV y se dividieron en 3 grupos como leve, moderado y grave según PRAS.
ResultadosCuando se compararon los datos entre grupos; en términos de mutación genética, se observó una diferencia significativa en la subprueba de tratamiento de la forma parental PedsQL a favor del grupo de mutación genética M694V (p<0,05). En términos de PRAS, se observaron diferencias significativas en las subpruebas de dolor, tratamiento y puntuación total del formulario PedsQL-niño, y en las subpruebas de dolor, tratamiento, preocupación y puntuación total del formulario PedsQL-padre a favor del grupo leve (p<0,05).
ConclusionesLas mutaciones del gen MEFV en niños y adolescentes con FMF no difirieron en la capacidad física y la calidad de vida. PRAS no fue eficaz en los parámetros físicos, pero la calidad de vida disminuyó a medida que aumentó la puntuación de gravedad. Animar a los niños/adolescentes con FMF a participar en actividades físicas y apoyarlos psicosocialmente puede ser importante para mejorar su calidad de vida.
Familial Mediterranean Fever (FMF) is the most common inherited autoinflammatory disease in the world. FMF is an autosomal recessive autoinflammatory disease characterized by recurrent inflammatory attacks of the serosal and synovial membranes, accompanied by fever, abdominal pain, chest pain, and joint pain.1 It is especially common in communities around the Mediterranean, such as Jews, Turks, Armenians and Arabs. Although different prevalences are reported in studies conducted in Turkey. There are individuals with FMF over 100,000, and the carrier rate has been reported as 1/5.2
FMF is caused by mutations in MEFV gene, which encodes a protein called pyrin (pyrin), which has regulatory functions on the innate immune system.3,4 The MEFV gene responsible for this disease was identified in 1997 and 335 kinds of mutations have been reported to date, but their clinical relevance is largely unknown and their interpretation is difficult.5 The most common mutations are M694V, M680I, M694I, V726A and E148Q.6 In FMF, mutations in the MEFV gene disrupt the interaction of pyrin with microtubules PKN and 14-3-3 proteins, facilitating the formation of a proinflammatory pyrin inflammasome. Pyrin activates caspase-1 to convert pro-IL 1β and pro-IL-18 into mature forms IL-1β and IL-18 when inflammatory combine, and cells undergo an inflammatory breakdown called pyroptosis. Overactivation of pyrinitis and the resultant inflammation triggers the febrile inflammatory episodes typical of FMF.3,4 Characteristics of FMF attack is the presence of pain due to inflammation that starts in one or more parts of the body, accompanied by fever, the attacks last for up to 1–4 days and can heal without treatment, and the individual is completely normal between attacks. The frequency of attacks can vary from once a week to every 3–4 months.7 FMF patients can usually recognize the triggers that cause an attack beforehand. e.g.; emotional stress, exposure to cold, menstruation or travel.8,9
Joint pain is the most common symptom of FMF after abdominal pain and fever in children. A non-erosive arthritis involving a single large joint is usually seen in the lower extremity. In addition, symmetrical or asymmetrical involvement of more than one joint in childhood is a condition that can be encountered. During attacks, myalgias, which usually start spontaneously or with exercise and predominantly affect the lower extremities, can also be seen.10 Arthritis symptoms usually resolve after an attack, but cases of chronic arthritis have also been reported.11 In chronic arthritis, involvement of the hip and knee joints can be seen, which can last for weeks or even months.12 In addition, some patients complain of muscle pain in the lower extremity that occurs after physical exertion or prolonged standing.13 Joint attacks are more common in patients with M694V mutation and have been reported to be associated with more severe disease and an increased risk of AA type amyloidosis.14 Due to FMF attacks and related musculoskeletal problems, individuals can reduce their daily living activities. We think that the decreased activity level may negatively affect the ability of the individual to maintain the activities necessary for daily life and thus physical independence and quality of life. This can create a vicious cycle resulting in symptoms leading to loss of physical capacity, resulting in symptom exacerbation and poor quality of life. In the literature, there are not enough studies evaluating the physical capacity and quality of life of children/adolescents with FMF according to gene mutation or disease severity. A study was reported that attacks of FMF significantly affected patients’ physical activity, but reaching this conclusion did not make any comparisons.15 In terms of MEFV gene mutation, FMF are compared with healthy group or age groups in a small number of studies investigating the relationship between the disease characteristic features and the disease severity. And these studies were emphasized that more studies are needed to support the data obtained.16,17
Considering all these situations, we aimed to investigate how gene mutation and disease severity affect physical capacity and quality of life in children/adolescents with FMF.
MethodsThis study was planned as a single-center cohort study. Eighty children/adolescents between the ages of 7–18, who were diagnosed by a rheumatologist according to Tell-Hashomer criteria at Pamukkale University Pediatric Rheumatology Clinic and followed by Pamukkale University Pediatric Rheumatologic Physical Therapy And Rehabilitation Clinic were included in the study.
Inclusion criteria: (a) Being diagnosed with FMF according to the criteria of Tell-Hashomer, (b) being between the ages of 7–18, (c) volunteering to participate in the study. Exclusion criteria: (a) Presence of cardiovascular, pulmonary, orthopedic and neurological problems that may affect physical condition. (b) Having a cognitive disability that is unable to cooperate. (c) Inability to understand or speak Turkish. (d) Concurrent autoimmune or inflammatory disease. (e) Diseases affecting the central nervous system. (f) Serious psychiatric conditions that preclude participation (e.g., psychotic disorders). (g) Have had any surgery in the past six months.
Ethical approval of the study was obtained from the Non-Interventional Clinical Research Ethics Committee of Pamukkale University (60116787-020/75852). All individuals were informed verbally and informed consent forms were signed.
Patient assessmentAll evaluations were carried out by the same researcher, in the same conditions, by face-to-face interview method. After the demographic and clinical data of the participants were recorded, disease severity was evaluated with PRAS disease severity score; motor proficiency with running speed and agility and strength subtests of Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2 SF); physical activity level with Physical Activity Questionnaire; quality of life with Pediatric Quality of Life Inventory 3.0 Arthritis Module (PedsQL). Evaluations were carried out in approximately 40min. Participants were divided into 2 groups as M694V and other mutations according to MEFV gene mutation and were divided into 3 groups as mild, moderate and severe according to PRAS.
PRAS disease severity scoreThis scoring system was developed by Pras et al. to determine the disease severity in individuals with FMF. Disease severity score was classified as mild (3–5), moderate (6–9), and severe (>9). The higher the score, the higher the disease severity.18
Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2 SF)BOT-2 short form consists of 8 subtests and 14 items and can be completed in 15–20min. Subtests were fine motor precision, fine motor integration, manual dexterity, bilateral coordination, balance, running speed and agility, upper limb coordination, and strength. Motor skill increases as score increases.19 BOT-2 provides information about general motor skills as well as fine and gross motor skills separately. Compared to other motor skill tests, it is advantageous in that it has a wider age range, is easily understood by children, attracts children's attention in terms of visuality, is easy to apply and, unlike other tests, it evaluates coordination. In our study, running speed and agility (One leg Stationary Hop) and strength (Sit Up, Push Up) subtests of BOT-2 SF were used to evaluate.
Physical Activity QuestionnaireThe Physical Activity Questionnaire was developed in the United States by Kowalski et al.20 This questionnaire contains nine items. It examines the physical activities of children aged 7 and over in the last seven days and the frequency of these activities. The answers are a five-point likert. An increase in the score indicates an increase in the physical activity level.
Pediatric Quality of Life Inventory (PedsQL) 3.0 Arthritis ModuleThe PedsQL 3.0 Arthritis Module was developed to assess health-related quality of life in children with rheumatic disease. PedsQL 3.0 Arthritis Module has “Pain” (4 items), “Daily Activities” (5 Items), “Treatment” (7 items), “Worry” (3 items) and “Communication” (3 items) subtests and consists of 22 items in total. There are child and parent forms separated by different age groups (2–4 years, 5–7 years, 8–12 years and 12–18 years). In our study, 8–12 age and 12–18 age child and parent forms were used to evaluate the quality of life of individuals with FMF. A high total score indicates a high quality of life.21
Statistical analysisThe data were analyzed with the SPSS 21.0 package program. The Kolmogorov–Smirnov test was used to determine whether the continuous variables were normal distributions. Continuous variables were expressed as mean±SD for normal distributions and median (minimum–maximum) for non-normal distributions. The categorical variables were expressed in numbers and percentage. One Way Anova Test and Independent Sample T-Test for comparison of independent group differences when parametric test assumptions were met; When parametric test assumptions were not met, Kruskal–Wallis Test and Mann–Whitney U test were used to compare independent group differences. A value of p<0.05 was accepted as statistically significant.
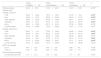
ResultsThe demographic and clinic data of the participants are shown in Table 1. The distribution of the participants according to the gene mutation is given in Table 2. The descriptive data of the evaluation parameters are in Table 3.
Demographic and clinical data of participants.
| Variables | n (%) |
|---|---|
| Gender | |
| Female | 42 (52.5) |
| Male | 38 (47.5) |
| Dominant side | |
| Right | 74 (92.5) |
| Left | 6 (7.5) |
| Use of colchicine | |
| Right | 74 (92.5) |
| Left | 5 (6.3) |
| Colchicine daily dose | |
| One | 27 (33.8) |
| One and a half | 8 (10) |
| Two | 32 (40) |
| Three | 3 (3.8) |
| Consanguineous marriage | 16 (20) |
| FMF family history | 36 (45) |
| Fire | 49 (61.3) |
| Stomach ache | 51 (63.7) |
| Arthralgia | 53 (66.3) |
| Arthritis | |
| Total | 28 (35) |
| Knee | 24 (30) |
| Ankle | 25 (31.3) |
| Elbow | 5 (6.3) |
| Wrist | 8 (10.0) |
| Single limb | 54 (67.5) |
| Bilateral | 23 (28.7) |
| Pleuritis | 26 (32.5) |
| Diarrhea | 20 (25) |
| Redness | 15 (18.8) |
| Skin rash | 13 (16.3) |
| Vasculitis | 1 (1.3) |
| Dialysis history | 13 (16.3) |
| Oralafht | 24 (30) |
| Headache | 35 (43.8) |
| Amyloidosis | 1 (1.3) |
| Mean±SD | Median (min/max) | |
|---|---|---|
| Age (years) | 12.6±3.10818 | 13 (7/18) |
| Height (m) | 1.51±.15969 | 1.54 (1.10/1.87) |
| Body weight (kg) | 44.78±15.67173 | 45.5 (8/104) |
| BMI (kg/m2) | 19.5458±7.49211 | 18.51 (3.46/76.03) |
| Age of diagnosis | 7.75±3.96663 | 7.5 (1/17) |
| Clinical well-being (physiotherapist) | 74.22±26.96897 | 80 (10/100) |
FMF: Familial Mediterranean Fever; kg: kilogram; m: meter; mg: milligram; BMI; body mass index.
Distribution of participants by gene mutation.
| Gene mutation | n | % |
|---|---|---|
| M694V | 27 | 33.8 |
| V726A | 6 | 7.5 |
| E148Q | 3 | 3.8 |
| R202Q | 5 | 6.3 |
| M680I | 5 | 6.3 |
| S166I | 2 | 2.5 |
| Compound mutation total | 28 | 35.0 |
| n | % | |
|---|---|---|
| • M694V.M680I.R202Q | 4 | 5.0 |
| • R202Q.V726A | 1 | 1.3 |
| • R202Q.M694V | 9 | 11.3 |
| • M694V.V726A.R202Q | 4 | 5.0 |
| • M694V.M680I | 2 | 2.5 |
| • E148Q.P369S | 1 | 1.3 |
| • R202Q.M680I | 1 | 1.3 |
| • E148Q.M694V | 2 | 2.5 |
| • E148Q.F479L | 2 | 2.5 |
| • P369S.I591T | 1 | 1.3 |
Descriptive data of evaluation parameters.
| Variables | Mean±SD | Median (min/max) |
|---|---|---|
| PRAS | ||
| Mild | 4.41±0.9380 | 5 (1/5) |
| Moderate | 7.05±0.7361 | 7 (6/8) |
| Severe | 10.71±1.8898 | 10 (9/13) |
| BOT-2 SF strength | ||
| Sit up | 3.47±1.2010 | 4 (0/6) |
| Push up | 3.38±1.3547 | 3 (0/6) |
| Running speed and agility | ||
| One leg stationary hop | 7.26±2.0047 | 8 (0/9) |
| Physical activity questionnaire | 20.47±6.9961 | 19.70 (7/42.14) |
| PedsQL child form | ||
| Total | 81.83±14.51 | 83.64 (32.22/100) |
| Pain | 73.49±26.3259 | 81.25 (0/100) |
| Daily activities | 93.5±12.3606 | 100 (40/100) |
| Treatment | 80.91±18.3094 | 85.74 (21.42/100) |
| Worry | 82.08±22.3103 | 91.66 (16.66/100) |
| Communication | 79.16±26.3196 | 83.33 (0/100) |
| PedsQL parent form | ||
| Total | 79.93±17.20 | 81.94 (17.84/100) |
| Pain | 75.56±24.7252 | 82.25 (0/100) |
| Daily activities | 94.25±12.6065 | 100 (30/100) |
| Treatment | 77.57±21.1900 | 80.35 (0/100) |
| Worry | 71.87±30.5947 | 83.33 (0/100) |
| Communication | 80.41±28.2249 | 100 (0/100) |
PRAS: Disease Severity Score; PedsQL: Pediatric Quality Of Life Inventory 3.0. Module Arthritis; BOT-2 SF: Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form.
When the data were compared according to the PRAS groups; there was a significant difference in favor of the mild group in the pain, treatment subtests and total score of the PedsQL-child form and in the pain, treatment, worry subtests and total score of the PedsQL-parent form (p<0.05). There was no difference between the groups in physical activity score and BOT-2 SF (p≥0.05) (Table 4). When the data were compared between M694V and Other Mutations, a significant difference was found in favor of the M694V gene mutation group only in the treatment subtests of the PedsQL-parent form (p:0.045). There was no difference between the groups in physical activity score and BOT-2 SF (p≥0.05) (Table 5).
Comparison of data by PRAS groups.
| PRAS-mildMean±SD | PRAS-moderateMean±SD | PRAS-severeMean±SD | p | |
|---|---|---|---|---|
| Physical activity questionnaire | 20.16±6.79 | 21.61±6.90 | 16.67±8.08 | 0.219* |
| PedsQL child form | ||||
| Total | 86.27±12.23 | 79.72±13.81 | 67.29±19.41 | 0.002* |
| Pain | 84.39±19.70 | 68.59±23.92 | 36.60±31.95 | 0.000** |
| Daily activities | 94.87±10.09 | 92.50±12.98 | 90.71±20.29 | 0.490** |
| Treatment | 85.67±18.74 | 79.19±14.77 | 62.75±20.91 | 0.003** |
| Worry | 84.61±19.82 | 82.10±23.22 | 67.85±28.63 | 0.416** |
| Communication | 81.83±24.69 | 76.22±29.66 | 78.57±17.91 | 0.613** |
| PedsQL parent form | ||||
| Total | 86.97±11.31 | 76.60±16.44 | 56.88±24.38 | 0.000* |
| Pain | 86.89±16.31 | 69.30±22.94 | 42.85±34.12 | 0.000** |
| Daily activities | 97.17±7.05 | 92.50±14.36 | 86.42±22.30 | 0.074** |
| Treatment | 85.22±16.21 | 73.42±21.01 | 55.12±27.41 | 0.000* |
| Worry | 81.19±25.84 | 68.62±29.37 | 35.71±34.59 | 0.003** |
| Communication | 84.40±25.80 | 79.16±28.59 | 64.28±36.86 | 0.213** |
| BOT-2 SF strength | ||||
| Sit up | 3.43±1.20 | 3.44±1.28 | 3.85±.69 | 0.726** |
| Push up | 3.56±1.23 | 3.20±1.40 | 3.28±1.79 | 0.356** |
| Running speed and agility | ||||
| One leg stationary hop | 7.10±2.13 | 7.35±2.02 | 7.71±.95 | 0.793** |
BOT-2 SF; Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form; PedsQL; Pediatric Quality Of Life Inventory 3.0. Module Arthritis; Bold p values are significant. p<.05.
Comparison of data between M694V and other mutations.
| M694VMean±SD | Other mutationsMean±SD | p | |
|---|---|---|---|
| Physical activity questionnaire | 21.64±7.76 | 19.80±6.63 | 0.282* |
| PedsQL child form | |||
| Total | 85.08±10.29 | 79.50±16.45 | 0.116* |
| Pain | 78.84±23.05 | 70.59±28.34 | 0.201* |
| Daily activities | 93.14±11.10 | 93.64±13.15 | 0.333** |
| Treatment | 83.99±16.10 | 78.61±19.45 | 0.227* |
| Worry | 83.33±22.04 | 80.20±23.29 | 0.516** |
| Communication | 86.11±19.74 | 74.47±29.34 | 0.092** |
| PedsQL parent form | |||
| Total | 83.70±13.05 | 77.60±19.52 | 0.151* |
| Pain | 79.86±23.91 | 73.95±25.89 | 0.334* |
| Daily activities | 94.25±9.27 | 94.68±14.26 | 0.155** |
| Treatment | 83.60±20.32 | 73.19±22.98 | 0.045* |
| Worry | 73.76±28.74 | 70.31±33.01 | 0.991** |
| Communication | 87.03±20.32 | 75.86±32.08 | 0.178** |
| BOT-2 SF strength | |||
| Sit up | 3.29±1.35 | 3.58±1.02 | 0.315** |
| Push up | 3.62±1.44 | 3.35±1.15 | 0.209** |
| Running speed and agility | |||
| One leg stationary hop | 6.70±2.46 | 7.66±1.35 | 0.051** |
PedsQL; Pediatric Quality Of Life Inventory 3.0. Module Arthritis; BOT-2 SF; Bruininks-Oseretsky Test of Motor Proficiency Second Edition Short Form; Bold p values are significant. p<.05.
We examined how gene mutation and disease severity affect physical capacity and quality of life in children/adolescents with FMF. As a result, we have seen that the MEFV gene mutations has similar effects on physical capacity and quality of life, disease severity has a similar effect on physical parameters, but the quality of life decreases as the disease severity score increases in children/adolescents with FMF.
Cekin et al.,16 examining the relationship between MEFV mutations and clinical symptoms in the literature, emphasized that M694V was the most common genotype and individuals with M680I, P369S, and K695R genotype mutations had more severe symptoms, while FMF-related symptoms were less severe in individuals with E148Q or V726A-related genotypes. We could not find any study in the literature showing which gene mutation type affects physical activity level and quality of life. Therefore, we divided and analyzed our participants into two groups, the most common genotype, M694V and other mutations. As a result of our evaluations, we saw that the type of mutations had a similar effect in terms of physical capacity and quality of life. So, we think that the disease caused low physical capacity and quality of life by affecting the disease regardless of gene mutation, therefore, it did not make a difference between the groups. However, our study evaluated only children/adolescents with FMF who applied to the clinic of the region we live in. For this reason, we believe that evaluations should be made in larger sample groups to examine whether the type of gene mutation is effective or not. Since it is a common disease in Turkish society, it is very important to review a general evaluation for our country from this point of view. The results can help reorganize treatment programs by providing clinicians and researchers with an idea about how the disease will progress.
Today, the PRAS Scoring System, developed by Pras et al.,13 is most frequently used to evaluate the severity of FMF disease. In this scoring system, the age of onset of the disease, the number of attacks per month, acute or prolonged arthritis status, the presence of erysipelas-like erythema, the development of amyloidosis and the dose of colchicine used are evaluated. In our study, we used this system to classify the exposure of children/adolescents with FMF to the disease. In the comparative analysis made according to this classification, we observed that the level of exposure to the disease did not make a difference on the physical capacities and activity levels of these children/adolescents, while it made a difference on the quality of life. This result showed us that these children/adolescents have similar physical capacity regardless of the effect of the disease, but their quality of life is affected worse as the disease becomes active.
Symptoms seen in rheumatic diseases cause a sedentary lifestyle.15,22,23 Alaylı et al.24 reported that children with FMF had lower functional capacity and muscle strength compared to healthy children. The effect of the disease exposure of children/adolescents with FMF on physical capacity and physical activity level was examined in only one study. Babaoglu et al.15 measured physical activity levels, using a pedometer, and determined that the steps in the attack period were significantly reduced compared to the non-attack period. In children and adolescents with FMF as in other rheumatological diseases, musculoskeletal symptoms that occur during the attack and can become chronic may decrease the level of physical activity by causing a sedentary lifestyle. While this situation was caused by pain and joint swelling due to joint involvement during attacks, the postural disorder of this acute effect in the long term may have led to impaired alignment of muscles and joints, atrophy, contractures and deformities, leading to limitation of physical activities. Also, patients with FMF need daily use of colchicine. However, this drug can cause myopathy and reduce muscle strength.25 Decreased muscle strength may also have made these individuals reluctant to participate in physical activity. In the light of all these reasons, the insufficient activity in each period of the disease, as in our study, may not have made a difference by creating a similar effect for these children in each period of the disease.
Chronic diseases cause both psychological and physical symptoms, and these symptoms lead to difficulties in daily living activities and quality of life.26 Increasing the quality of life in individuals with chronic diseases is one of the most important goals of treatment. Quality of life is a multidimensional concept that focuses on the subjective perception of emotional, social and physical functioning.27 Therefore, we think that it is important to evaluate the quality of life in order to understand the effects of the disease on the life of the patients. Although evaluation studies on quality of life in children and adolescents with FMF are generally performed on young adults, we see that there are also studies on children. Studies have emphasized that the quality of life of adults and children with FMF is lower compared to healthy controls.24,27–31 In a study comparing patients with FMF in Germany and Turkey, they stated that quality of life was affected, but there was no relationship between disease severity and quality of life.32 Our study also stated that the level of disease severity affects the quality of life of children/adolescents with FMF. Progression of the disease with attacks, emergence of symptoms during the attack period, etc., as seen in other studies, were expected to affect the quality of life. Our study observed that the quality of life of children/adolescents with FMF and their families decreased as the disease severity score increased. Therefore, we believe that these children/adolescents and their families need psychosocial support.
The strength of this study is that it is the first study to evaluate together the effects of gene mutation and disease severity score on physical capacity and quality of life in children/adolescents with FMF. The limitation of our study is that cases belonging to a single clinic were evaluated.
ConclusionThe results of our study showed that the gene mutation and disease severity of children/adolescents with FMF did not make a difference on physical capacity. We think that the literature on the evaluation of physical activity levels is insufficient and there is a need for more studies with a larger sample size on which factors are effective on physical capacity in these children/adolescents. Another result of our study was that the quality of life of children/adolescents with FMF was affected by disease severity level. Poor sleep quality, anxiety, depression, and fatigue are frequently neglected health problems in FMF patients.31,33 Since the presence of these problems may also affect the quality of life, we believe that such psychosocial parameters should be included in the evaluations in future studies and that it is important to support these children/adolescents and their families from a psychosocial point of view.
Authors’ contributionsBBC and EGK participated in the design of the study. ZET and GOY diagnosed patients and checked eligibility for inclusion criteria. MB, EGK and BBC collected data. EGK and BBC did statistical analyses, commented on statistics. MB and EGK wrote the article. EGK, BBC and SY contributed to the critical revision of the manuscript.
Ethical approvalEthical approval of the study was obtained from the Non-Interventional Clinical Research Ethics Committee of Pamukkale University (60116787-020/75852).
FundingThis study did not receive any specific grant from funding agencies.
Conflicts of interestThe authors declare that there is no conflict of interest.