I read with interest the clinical cases published by Dr Arango Guerra et al.1 on spontaneous pneumomediastinum in patients with anti-MDA dermatomyositis.5
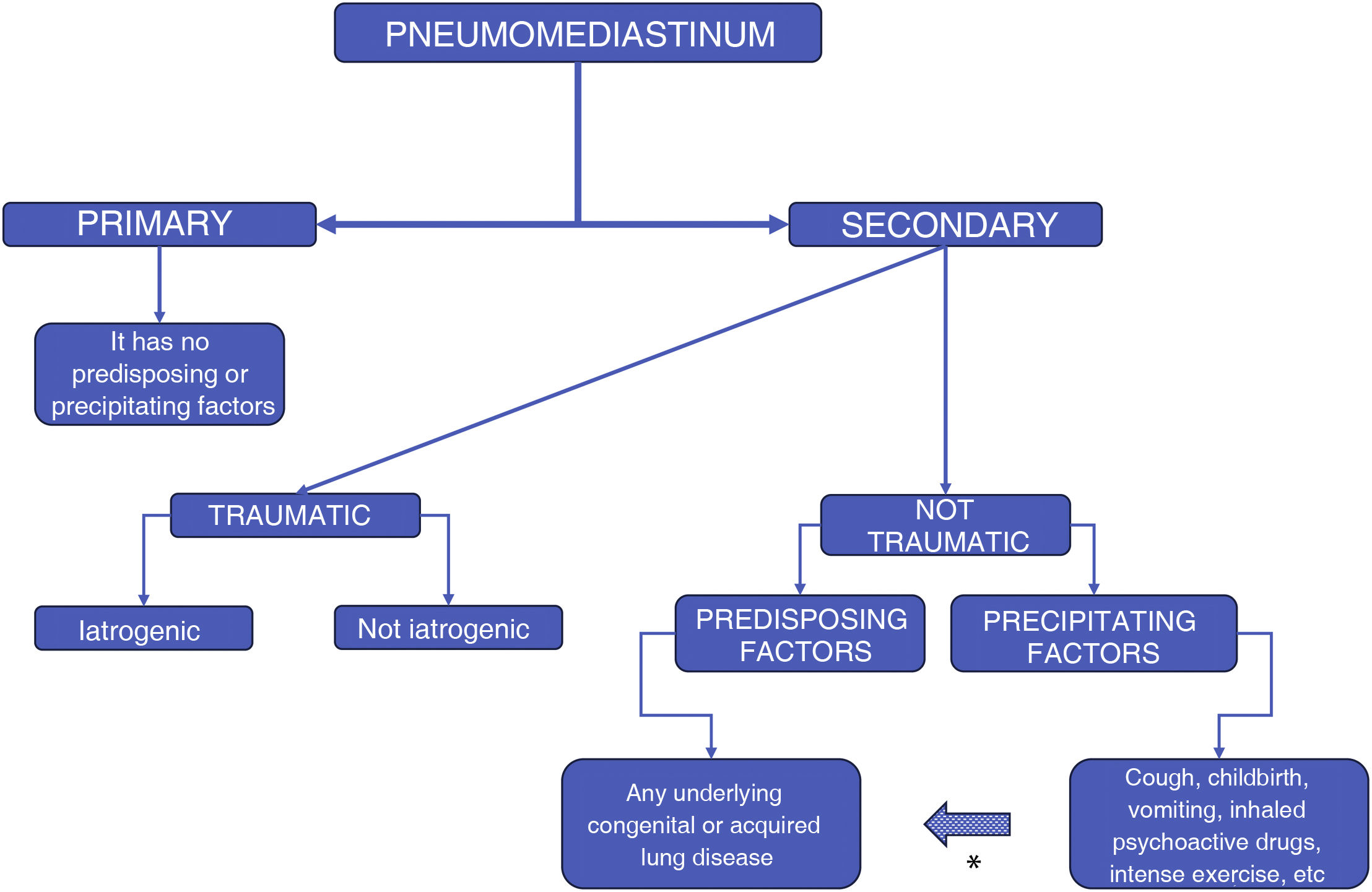
Historically, pneumomediastinum has been divided into two groups: spontaneous, when pneumomediastinum occurs without an apparent cause, and secondary, when an event that triggers it can be identified. In line with the above, we consider that the pneumomediastinum described by the authors was not spontaneous, as both cases presented a previous lesion in the lung parenchyma, due to the interstitial involvement caused by anti-MDA dermatomyositis,5 and this damage predisposes patients to pneumomediastinum. Spontaneous pneumomediastinum cannot have a predisposing disease or precipitating factors: it must occur "spontaneously". This type of pneumomediastinum, according to its definition, is better termed primary, because it does not have a specific cause that gave rise to it. The classification of pneumomediastinum by "spontaneous" and "secondary" is imprecise and should be avoided due to numerous predisposing factors and triggering events present in what is currently called "spontaneous." We believe that the names of medical disorders should optimally reflect the underlying pathophysiology, and when traditional names of disorders lead to confusion between different pathophysiological processes, the name should be changed.
We prefer terminology that takes into account not only the aetiology of pneumomediastinum but that also helps to guide selective management strategies for better care and is also easy to remember and useful for teaching purposes.2,3
Truly "spontaneous" (primary) pneumomediastinum, as expressed, cannot have a specific apparent aetiology, and we emphasise that it cannot have any evident causal factor by its definition, unlike the secondary case, where there are various factors that can trigger this. This classification reflects clinical rather than pathophysiological circumstances and is therefore confusing and inappropriate for our point of view. Consequently, we believe that classification should evolve towards a greater degree of precision (Fig. 1).
If a pneumomediastinum has a predisposing factor that compromises the lung structure, whether congenital, hereditary or genetic (bronchiectasis, cystic fibrosis, surfactant changes, etc.) or acquired (asthma, COPD, interstitial lung disease, COVID-19, etc.), it cannot be spontaneous because there is an underlying disease that gives rise to a predisposition. Similarly, pneumomediastinum that occurs due to a precipitating factor (coughing, labour, intense exercise, use of inhaled drugs, mechanical ventilation, etc.) in a healthy person or with an underlying lung disease, cannot be spontaneous either, as there is an immediate triggering event that causes this. These factors may be present at the same time and cause pneumomediastinum: for example. cough or vomiting and acquired lung disease. The resulting pneumomediastinum is thus secondary.2 Likewise, pneumomediastinum that occurs in other conditions such as anorexia nervosa, Marfan syndrome, Ehlers-Danlos syndrome, malnutrition, idiopathic inflammatory myopathies, diabetic ketoacidosis, etc., is not spontaneous either.
Primary pneumomediastinum is a truly rare event and very rarely reported in the medical literature.4–7
In conclusion
- •
The true definition and classification of pneumomediastinum does not match what has been published. The definition has thus been misused.
- •
The term "spontaneous" pneumomediastinum should be omitted here and termed primary pneumomediastinum.
- •
Primary pneumomediastinum is a pneumomediastinum that occurs without any obvious causal factor (predisposing or precipitating). Under these conditions, it is a supremely rare condition.
- •
Secondary pneumomediastinum is a pneumomediastinum that occurs when there is an obvious causal factor (predisposing or precipitating, or both). This is the most frequently reported condition.
None.
Conflict of interestNone.