Monckeberg's medial sclerosis (MMS) is a non-inflammatory degenerative condition affecting primarily the arteries of extremities and visceral organs. MMS in temporal artery is rare and may present some clinical similarities with giant cell arteritis (GCA). We aimed to draw attention to this pathology by sharing our case with MMS in temporal artery (TA) mimicking GCA.
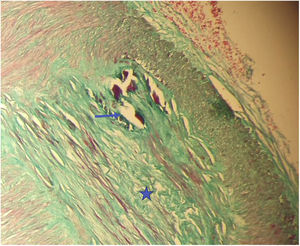
A 72-year-old female patient was referred to our clinic due to severe headache without any pathological finding in cranial computerized tomography and magnetic resonance imaging. She had a two-week history of headache with severe tenderness on right temporal area. Clinical and laboratory evaluations were unremarkable except the tenderness on right temporal area, high erythrocyte sedimentation rate (ESR 37mm/h) and mild anemia. There was no “halo sign” in color Doppler ultrasonography (USG). Oral methylprednisolone was started and temporal artery biopsy (TAB) was performed to confirm GCA. Her complaints were responded to glucocorticoid and resolved in three weeks. In the histopathological evaluation TAB, there were MMS characteristics with degeneration and calcification in the internal elastic lamina in tunica media and obliteration in lumen of medium-large-sized vessel (Fig. 1). GCA was excluded and medication was gradually stopped.
Masson Trichrome, 200×. The histopathological evaluation of temporal artery biopsy specimen; Monckeberg's medial sclerosis characteristics with degeneration (star) and calcification (arrow) in the internal elastic lamina in tunica media and obliteration in lumen of medium-large-sized vessel.
MMS is a non-inflammatory degenerative condition affecting primarily the tunica media of arteries resulting in their calcification.1 As a mimicker of GCTA, it may be considered as a non-giant cell temporal arteritis pathology. It is frequently, but not exclusively, associated with aging, type 2 diabetes mellitus, chronic kidney diseases, hormonal disorders and vitamin deficiencies and it may lead to hemodynamic changes in the microcirculation and with its progress, it may cause decreased organ perfusion.2 It occurs predominantly in femoral, tibial, radial, coronary, cerebral and visceral vessels with generally no symptoms. However, acute vascular complications including ischemic changes have also been reported.3
MMS in TA has only rarely been reported previously and due to shared features with GCA, it may become a diagnostic challenge for the clinician.1–3 Symptoms indistinguishable from GCA such as headache, facial pain, tenderness in the temporal area, temporal artery hardening and acute vision loss have been reported in patients with MMS in TA.1,2 Also the pain due to MMS in TA was reported to be managed with glucocorticoids.1 Although high ESR is expected in GCA, normal values do not exclude the diagnosis. The “halo sign” in Doppler USG is important in GCA however, it is not seen in all patients. Several imaging findings in plain radiographs, CT and USG have also been reported for MMS in the head and neck region.1
TAB remains the gold standard for the diagnosis of GCA. However, besides the possibility of false-negative biopsy result due to the skip lesions in GCA, other vasculopathy possibilities (atherosclerosis in the majority and MMS in the minority of the cases) should also be kept in mind. Histopathologically, besides an intact intima, degenerations and calcification in the internal elastic lamina in tunica media and obliteration in lumen of medium–large-sized vessel can be seen in MMS. However, endothelial structural disorganization, repair and thickening of the intima, as well as deformity of the arterial wall can be identified in atherosclerosis. Indeed, in a large series in suspected GCA cases, MMS was described in 6% of the TAB specimens.4
In conclusion, MMS in TA can mimic GCA due to the similarities of clinical features. It may become a diagnostic challenge for the clinician and an increased awareness of the disease may contribute to diagnosis.
Conflict of interestThe authors declare that they have no conflict of interest.