Rheumatoid arthritis (RA) is a systemic chronic inflammatory disease that primarily affects synovial joints.1 However, extra-articular manifestations may be present in up to 40% of RA patients, involving the central (CNS) and peripheral nervous systems (PNS) less frequently, with an estimated incidence of 11%.2,3 Mechanical factors, vasculitis, accelerated atherosclerosis or the systemic illness itself may be involved in its pathophysiology.1,2 Furthermore, iatrogenic events with neurological manifestations can also occur.2,4 We aim to retrospectively characterize the neurological manifestations of RA patients referred to the Neuroimmunology outpatient clinic of a tertiary hospital.
An observational retrospective cohort study was conducted including patients referred to the Neuroimmunology outpatient clinic of Centro Hospitalar Universitário de Santo António between 1976 and 2023 with a diagnosis of RA. We collected demographic and clinical data regarding the patient, the rheumatic disease and the neurological manifestation and performed descriptive analysis.
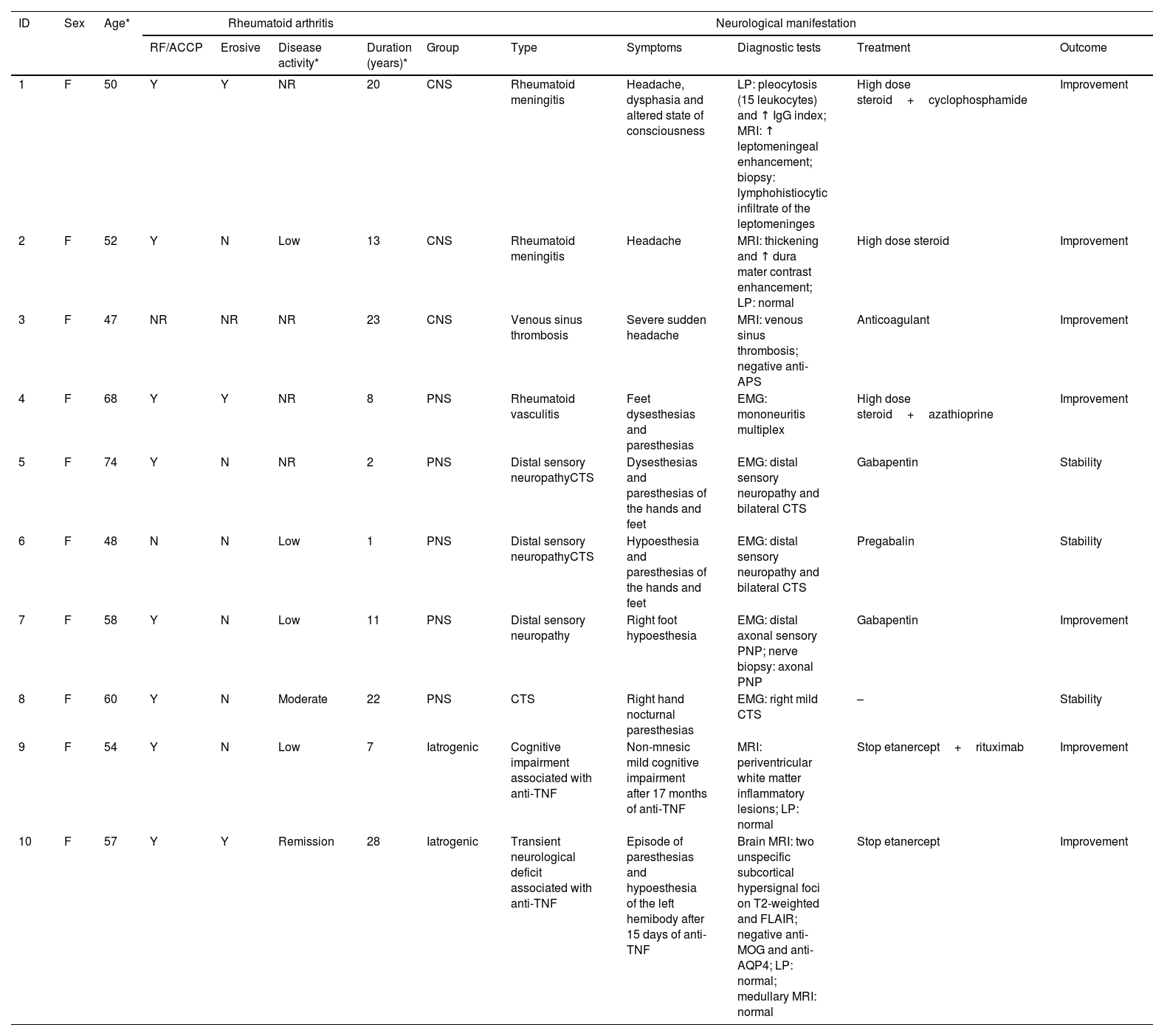
From a total of 1979 patients observed in the Neuroimmunology outpatient clinic, 36 had RA, the majority being female (n=32, 89%), with a mean age of 54.4±13.7 years. Of these, 10 (28%) had neurological manifestations attributable to RA (Table 1), 5 (14%) had neurological autoimmune comorbidities and 21 (58%) suffered from another neurological illness. Among patients with neurological manifestations attributable to RA, the majority had seropositive (n=8, 80%), prolonged disease (mean duration 13.5±9.3 years) and it was in low activity or in remission (n=5/6, 83.3%) at the time of the neurological condition. Excluding iatrogenic events, the PNS was the most frequently affected (n=5 vs. n=3 of CNS involvement), with distal sensory neuropathy and carpal tunnel syndrome (CTS) being the most prevalent manifestations. Regarding the three cases of CNS involvement, two were rheumatoid meningitis that implied an optimization of immunosuppression, and one was venous sinus thrombosis in a patient with other procoagulant risk factors, namely oestrogen contraceptive and recent breast cancer. Two cases of neurological events attributable to the use of anti-TNF were reported, which led to the suspension of the drug with improvement of the condition. Regarding neurological autoimmune comorbidities, four patients were followed for myasthenia gravis and one for multiple sclerosis. In the remaining patients, the symptoms can be categorized into the following groups: cognitive impairment (n=8), headache (n=7), vertigo (n=1), epilepsy (n=1), hypertensive encephalopathy (n=1), diplopia (n=1), gait disturbance (n=1) and depressive syndrome (n=1).
Descriptive analysis of the neurological manifestations presented by patients with rheumatoid arthritis referred to the Neuroimmunology outpatient clinic.
| ID | Sex | Age* | Rheumatoid arthritis | Neurological manifestation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RF/ACCP | Erosive | Disease activity* | Duration (years)* | Group | Type | Symptoms | Diagnostic tests | Treatment | Outcome | |||
| 1 | F | 50 | Y | Y | NR | 20 | CNS | Rheumatoid meningitis | Headache, dysphasia and altered state of consciousness | LP: pleocytosis (15 leukocytes) and ↑ IgG index; MRI: ↑ leptomeningeal enhancement; biopsy: lymphohistiocytic infiltrate of the leptomeninges | High dose steroid+cyclophosphamide | Improvement |
| 2 | F | 52 | Y | N | Low | 13 | CNS | Rheumatoid meningitis | Headache | MRI: thickening and ↑ dura mater contrast enhancement; LP: normal | High dose steroid | Improvement |
| 3 | F | 47 | NR | NR | NR | 23 | CNS | Venous sinus thrombosis | Severe sudden headache | MRI: venous sinus thrombosis; negative anti-APS | Anticoagulant | Improvement |
| 4 | F | 68 | Y | Y | NR | 8 | PNS | Rheumatoid vasculitis | Feet dysesthesias and paresthesias | EMG: mononeuritis multiplex | High dose steroid+azathioprine | Improvement |
| 5 | F | 74 | Y | N | NR | 2 | PNS | Distal sensory neuropathyCTS | Dysesthesias and paresthesias of the hands and feet | EMG: distal sensory neuropathy and bilateral CTS | Gabapentin | Stability |
| 6 | F | 48 | N | N | Low | 1 | PNS | Distal sensory neuropathyCTS | Hypoesthesia and paresthesias of the hands and feet | EMG: distal sensory neuropathy and bilateral CTS | Pregabalin | Stability |
| 7 | F | 58 | Y | N | Low | 11 | PNS | Distal sensory neuropathy | Right foot hypoesthesia | EMG: distal axonal sensory PNP; nerve biopsy: axonal PNP | Gabapentin | Improvement |
| 8 | F | 60 | Y | N | Moderate | 22 | PNS | CTS | Right hand nocturnal paresthesias | EMG: right mild CTS | – | Stability |
| 9 | F | 54 | Y | N | Low | 7 | Iatrogenic | Cognitive impairment associated with anti-TNF | Non-mnesic mild cognitive impairment after 17 months of anti-TNF | MRI: periventricular white matter inflammatory lesions; LP: normal | Stop etanercept+rituximab | Improvement |
| 10 | F | 57 | Y | Y | Remission | 28 | Iatrogenic | Transient neurological deficit associated with anti-TNF | Episode of paresthesias and hypoesthesia of the left hemibody after 15 days of anti-TNF | Brain MRI: two unspecific subcortical hypersignal foci on T2-weighted and FLAIR; negative anti-MOG and anti-AQP4; LP: normal; medullary MRI: normal | Stop etanercept | Improvement |
ACCP: anti-cyclic citrullinated peptide antibody; APS: antiphospholipid syndrome; AQP4: aquaporin-4; CNS: central nervous system; CTS: carpal tunnel syndrome; EMG: electromyography; F: female; ID: identification; LP: lumbar puncture; MOG: myelin oligodendrocyte glycoprotein; MRI: magnetic resonance imaging; N: no; NR: not registered; PNP: polyneuropathy; PNS: peripheral nervous system; RF: rheumatoid factor; TNF: tumour necrosis factor; Y: yes.
Neurological manifestations of RA, although experiencing decreasing incidence thanks to increasingly effective disease-modifying antirheumatic drugs, are still present in clinical practice and can be so severe that may impose optimizing immunosuppression or, in case of an iatrogenic event, to suspend therapy. They are more common in seropositive and longstanding disease and have scarce correlation with disease activity.1–3 PNS is more frequently involved than CNS, usually comprising compressive neuropathies such as CTS, less reported in our cohort because it is rarely referred to Neurology.2,5 Among non-compressive neuropathies, distal sensory, autonomic and sensorimotor neuropathies are other examples of PNS involvement, the latter often vasculitic.2,3 When CNS is affected, it may involve atlantoaxial instability (also seldom referred to Neurology), meningitis, vasculitis and rheumatoid nodules.1,6 Interestingly, most of the neurological symptoms exhibited by our cohort was not directly attributable to the rheumatic disease and a significant number of patients presented cognitive impairment, a condition more frequent in RA than in the general population.2 To our knowledge, this is the first published data describing neurological manifestations in a RA cohort. A multidisciplinary cooperation between Rheumatology and Neurology is essential so that there is a correct recognition and appreciation of neurological complaints of patients with RA.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone declared.