Arthrosis or osteoarthritis (OA) is the most widespread rheumatic disease; in Spain it affects 10% of the population over 20 years of age (according to the EPISER 2000) and 19.6% of the population over 40 years of age (according to the EPISER 2016).1,2 The ArtRoCad study of the Spanish Society of Rheumatology estimated that the economic cost of OA in 2007 was 4738 million euros.3,4 Moreover, OA provokes more disability in elderly people than any other disease, significantly reducing their quality of life.
Although the general impression may be that research on OA is not achieving good results, this vision is not totally certain; while it is true that the translation of the results of research in the therapeutic area have yet to produce great changes. It is not totally certain because in these years there have been new concepts that soon will bear fruits. One of them is the consideration of the joint as an “organ” of the human body and OA as a dysfunction of this organ.5 This is meaningful because, although it seems to be obvious, the joint is not considered in the list of organs of the human body.
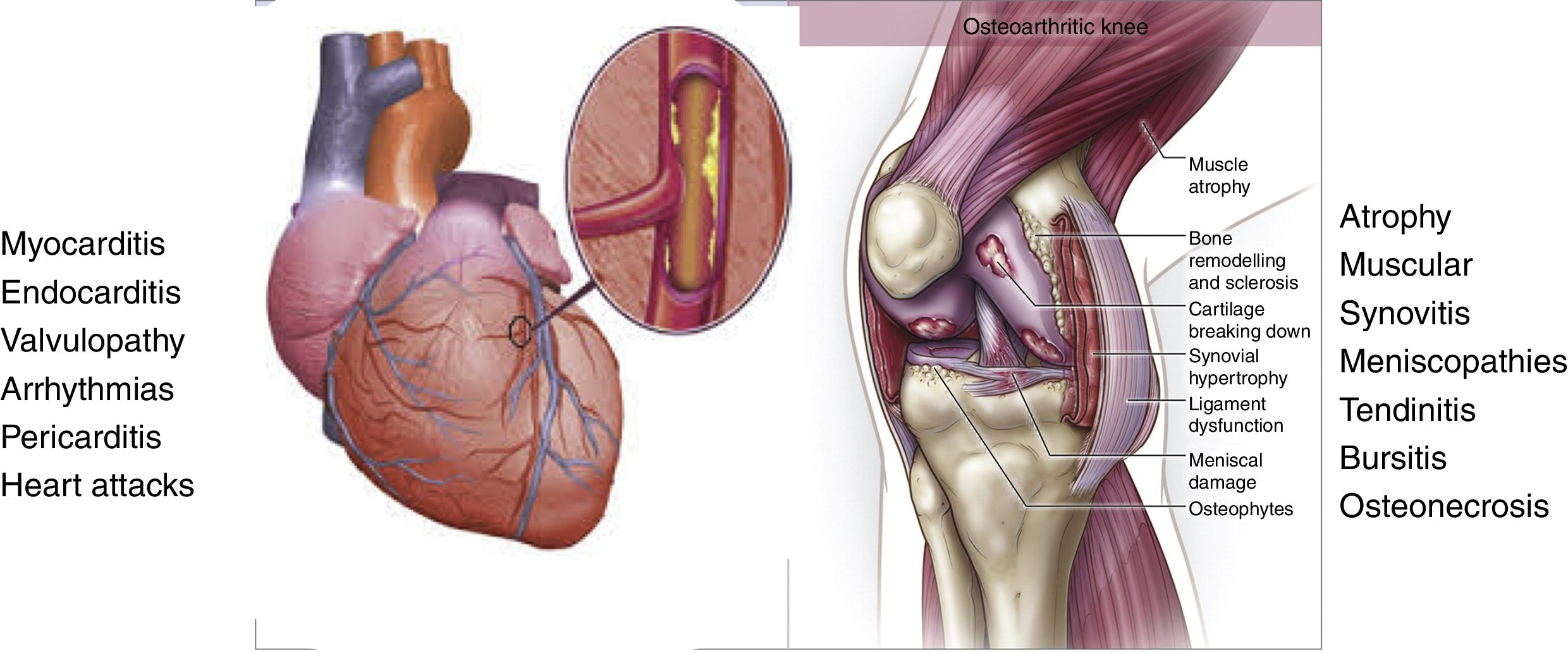
An organ is defined as a group of specialized tissues that has a determined structure and organization to fulfill a specific function. The heart is shown to be an organ constituted by a specific muscle (the cardiac muscle) associated to other types of tissues like the endocardium, the pericardium and conduction tissue structured in a way that it fulfills its major function of pumping blood. The knee joint is constituted by several types of tissues like the subchondral bone, the joint cartilage, the synovial membrane, the cruciate ligaments, meniscuses, the joint capsule, periarticular ligaments, bursae and skeletal muscle that surrounds them. All of these tissues are organized in a very specific form to fulfill the function of joint mobility. Unquestionably this constitutes another organ (Fig. 1).
The joint is like an organ. The knee joint is constituted by the subchondral bone, the joint cartilage, the synovial membrane, the cruciate ligaments, meniscuses, the joint capsule, periarticular ligaments, bursae and skeletal muscle that surrounds them. All of these specialized tissues are organized in such a way that collectively they are capable of fulfilling a function: joint mobility. Damage to these tissues can lead to the development of osteoarthritis and the dysfunction of the organ.
The dysfunction of an organ is generally the consequence of a condition that affects the organ. In the case of the heart, damage to the endocardium, poor function of the heart valves, changes in the conduction system, problems in coronary vascularization or disorders affecting cardiac muscle. If they become chronic, they can cause heart failure, and if they are not rapidly corrected they can lead to heart transplantation or the death of the patient.
In the knee joint, injury to the cruciate ligaments, degenerative menisci, inflammation of the synovial membrane, damage to the subchondral bone, injury to the periarticular musculature, if they become chronic, can lead to the development of OA and the loss of their function. If they are not treated adequately, it may be necessary to perform an implantation of a joint prosthesis (Fig. 1). This confirms that the concept of organ can be fully applied to the knee joint and how OA (as is the case of heart failure) can be considered a consequence of the changes in the joint that lead to the origin of the failure of the organ. This approach can lead us to think that we are talking of what has until now been referred to as “secondary OA”. This is another term that has fallen into disuse; OA is not classified as primary or secondary. Osteoarthritis always has a cause, and if not encountered it can be referred to as idiopathic, as occurs in other diseases. The current approach is that OA be classified in phenotypes; thus we have the aging phenotype, the inflammatory phenotype, the metabolic (changes in lipid or glycide metabolism), the biomechanical, hormonal or also referred to as osteoporotic.6,7 Advances in research will permit that these phenotypes become better defined and will also grow in number.
The OARSI (Osteoarthritis Research Society International) has launched a new definition of OA in the attempt to collect all these and other new concepts that are helping to advance the management of the patient with OA.8 The OARSI defines arthrosis as “a condition that involves the mobile joints characterized by cellular stress and the degradation of the extracellular matrix initiated by micro and macro lesions that activate responses of poor adaptation to reparation, which includes the proinflammatory pathways of innate immunity. The disease is first manifested as a molecular change (change in the metabolism of the joint tissue), followed by anatomical and/or physiological changes (characterized by the degradation of the cartilage, bone remodeling, the formation of osteophytes, inflammation of the joints and loss of their normal function), which may end in the disease.”
Of all the affirmations included in that definition, that which in my opinion is of the greatest relevance is that of proposing molecular changes in the center of the pathological process. It considers them to be the initial changes in joint destruction, and as such, it is where to focus works in research to better understand their pathogenesis, perform earlier diagnoses and improve treatment by discovering new therapeutic targets.
To understand the importance of the molecular changes in OA we can go back to compare the dos organs, the joint and the heart. Obesity and dyslipidemia are clearly risk factors for heart disease. The association between obesity and OA is indisputable. Patients who are obese or are overweight have nearly 3 times greater risk of developing OA in the knee than the population with normal weight, and the decrease in body mass index in 2 units or more over 10 years (approximately 5kg) reduces the risk of developing pain in an OA joint by 50%. This association between obesity and OA is classically explained by a purely mechanical effect: excess weight on the knee. However, today we also know that there are factors aside from the mechanical effect, molecular factors such as adipokines and more specifically leptin, resistin and adiponectin, which participate in the pathogenesis of arthrosis.6,9,10
More recently, work has begun to analyze the role of dyslipidemia and metabolic syndrome in OA. The results show that dyslipidemia damages the joint tissues in a way similar to cardiovascular tissues, which we could define as atherosclerosis of the joint. Synovial fluid (SF) is an ultrafiltrate from serum; for this reason the profile and the lipid levels in the two fluids are similar. The tissues of the knee joint, especially joint cartilage, receive nutrition from the molecules supplied by the SF. The changes in the composition of the SF have an impact on the nutritional status of the cartilage and on the quality of the tissue. Synovial fluid contains fatty acids that are necessary as a source of energy for the tissues of the joint, but they are also important for lubricating the joint and reducing the mechanical friction of the joint, facilitating the sliding of the two articular surfaces. The quantity and quality of the fatty acids in the SF of patients with OA is different than the SF of patients who do not have OA; there is a predominance of lipotoxic fatty acids (like palmitic acid), which induces the death of chondrocytes by apoptosis and the synthesis of proinflammatory and catabolic mediators.11,12 Joint cartilage is a tissue whose major source of energy is glucose; however, the chondrocyte in patients with OA has undergone a change in the ability to metabolize glucose and utilizes fatty acids as an alternative source. This change in the source of energy is referred to as a “metabolic switch” and increases the deposition of fatty acids in the cytoplasm.13 This all originates a loss of quality of the joint cartilage and facilitates its degradation and the process of OA.
Finally, the therapeutic area of the comparative analysis of the two organs, joint and heart, provides data that can help us to improve the treatment of OA. In the Rotterdam cohort, the incidence and progression to OA in the knee was lower among the patients who took statins for the control of dyslipidemia when compared with those who did not take them. This effect was greater in those patients who had been taking statins for more than a year.14 These data open the door to new treatments directed to the control of dyslipidemia (systemic, but also affecting the joints) to reduce the progression to OA of the knee, as well as its incidence. Logically we will need to conduct clinical trials directed at showing and validating this therapeutic approach.
In OA, aside from controlling the structural damage to the joint, the other therapeutic target is pain.15 Continuing with the comparative analysis involving the heart, this pain would represent the “angina of the joint”. Angina pectoris represents an important and alarming symptom that must be treated, but the therapeutic approach is very different from that of “joint angina”. In the case of joint pain it generally is not an alarming finding. In fact, I would even say exactly the opposite; it is reassuring; that is an error. If we treat joint pain with analgesics, we see how, little by little, the joint is destroyed, its function is lost and a joint prosthesis is required. This approach is unthinkable in angina pectoris. Can you imagine administering only treatment for coronary pain and see how the heart is destroyed? Treatment for pain in OA is what has been the focus a large part of research efforts and activity, even leaving apart the control of the joint structure, and this has also been an error. The current approach is different and what is considered a priority is to impede joint destruction, because that is the way not only to help to control the pain and progression to OA disease.
To achieve the therapeutic objectives in OA, as in heart disease, preventive medicine is indispensable, as is understanding the risk factors. Another question in which both areas, joint and cardiac disease again have things in common. However, this is another issue for another moment.
In conclusion, we must consider the joint as an organ and OA as a cause of the loss of function, which has different phenotypes. The knowledge of these new phenotypes will help us to improve the treatment of this disease. The metabolic dyslipidemic phenotype (atherosclerotic) is already a reality in OA and a valid example to continue to progress.
Please cite this article as: Blanco FJ. La artrosis y la ateroesclerosis de la articulación. Reumatol Clin. 2018. https://doi.org/10.1016/j.reuma.2018.08.001