We present a case of prostatitis with acute urinary retention as a rare initial manifestation of Wegener's granulomatosis.
MethodsThe case was a 48-year-old male with symptoms of prostatitis over 10 days. The patient presented urinary retention, with partial response to antibiotic treatment. High levels of cytoplasmic antineutrophil cytoplasmic antibody and a prostatic biopsy were compatible with Wegener's granulomatosis.
ResultsAfter starting treatment with glucocorticoids and cyclophosphamide, a significant improvement to the point of disappearance of symptoms was observed. At 3 months pulmonary and upper airway symptoms began, requiring higher doses of cyclophosphamide to control symptoms.
ConclusionsWegener's granulomatosis is a multisystem entity whose presentation as prostatitis with urinary retention is rare.
Presentar un caso de prostatitis con retención aguda de orina como manifestación inicial poco frecuente de granulomatosis de Wegener.
MétodosSe presenta el caso de un varón de 48 años con un cuadro de prostatitis de 10 días de evolución, que presentó retención de orina, con respuesta parcial al tratamiento antibiótico, y con niveles elevados de anticuerpos citoplasmáticos contra los neutrófilos con patrón citoplasmático y estudio anátomo-patológico de la biopsia prostática compatible con granulomatosis de Wegener.
ResultadosTras el inicio de tratamiento mediante glucocorticoides y ciclofosfamida se observa mejoría notable de los síntomas hasta su desaparición. A los 3 meses inicia clínica pulmonar y de vías aéreas superiores, precisando para el control de sus síntomas dosis mayores de ciclofosfamida.
ConclusionesLa granulomatosis de Wegener es una entidad multisistémica cuya forma de presentación como prostatitis con retención de orina es poco frecuente.
Granulomatosis with polyangiitis (GPA)1 previously known as Wegener's granulomatosis, is a clinicopathologic entity described by F. Wegener in 1936, characterized by granulomatous lesions in multiple organs and varying degrees of disseminated vasculitis of arteries and veins of medium and small caliber.2 The pathogenesis of the disease remains unknown, although it is believed that an abnormal hypersensitivity response develops against exogenous or endogenous antigens, probably located in the upper respiratory tract, synthesizing antibodies to proteinase 3, an enzyme present in polymorphonuclear cells. These antibodies are associated to a granular cytoplasmic staining pattern in these cells using indirect immunofluorescence, or anti-neutrophil cytoplasmic antibodies (c-ANCA) and may contribute to the pathogenesis of the disease.3 It affects men and women, with a 1:1 ratio, and the highest incidence occurs in the fifth decade of life, with an estimated 20 cases per million per year prevalence.
It affects the upper airway (92%) and lungs (85%), with granulomatous lesions, necrotizing vasculitis, as well as the kidneys (77%) in the form of glomerulonephritis.4 Urological extrarenal manifestations are very low in frequency and almost always develop in an advanced multisystem disease. We present a case of prostatitis as the first manifestation of Wegener's granulomatosis.
Clinical CaseThe patient was a 48-year-old male who was admitted with fever, urinary symptoms, suprapubic pain and acute urinary retention. The onset of symptoms had been 10 days before without other accompanying phenomena present. His medical history was unremarkable, except for being an ex-smoker of 15 cigarettes/day. On physical examination, temperature was 39°C, he had a distended bladder (evacuating, after a suprapubic cystostomy, 750ml), with painless renal fist percussion, and normal external genitalia .Rectal examination was very painful, with a grade 2/4 prostate, congestive without suspicious fluctuating abscessed areas.
Other initial tests highlighted leukocytosis (14.4×103/μl, neutrophils 70.2%), with the rest of the parameters being a normal blood count, a urine sediment with pyuria (410–420cells/field), hematuria (20–25 red blood cells/field) and intense bacteriuria. All other laboratory tests were normal.
With the presumptive diagnosis of acute bacterial prostatitis, treatment was started with ceftriaxone 2g/24h intravenously (iv), IV anti-inflammatory drugs and alpha blockers orally (po). The evolution was torpid, with fever and suprapubic pain yielding partially, but then developing asthenia, anorexia, joint/muscle pain and weight loss 10kg in 1 week. Given the negative results of blood cultures and urine, we started meropenem 1g/8h iv and new laboratory tests were performed: complete blood count with WBC 17,000 (N 93%), hemoglobin 12g/dl, hematocrit 36%, mean corpuscular volume 87fL, ESR: 36mm/h. Biochemistry: alanine aminotransferase 81U/l, gammaglutamil transpeptidase: 159U/l. Rheumatoid factor negative. C-reactive protein: 69. Salmonella and Brucella agglutinations were negative. C3, C4, AAT, copper and ceruloplasmin: normal. Antinuclear antibodies, anti-mitochondrial antibodies, antibodies to extractable nuclear antigens and anti-LKM1: negative. Anti-neutrophil cytoplasmic antibodies (ANCA) were positive at a titer of 1/160 (16U/ml) by indirect immunofluorescence, with a cytoplasmic pattern. Proteinogram: normal. Human chorionic gonadotropin beta and α-fetoprotein: normal. PSA 1.7ng/ml. Syphilis, human immunodeficiency virus, B and C hepatitis virus serology were negative. The Löwenstein–Jensen urine culture was negative.
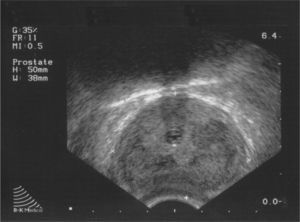
Chest X-ray and CT were normal. Abdominal ultrasound and CT showed a prostate with a volume of 56cm3, without evidence of abscess. Flexible cystoscopy confirmed the enlargement of the prostate.
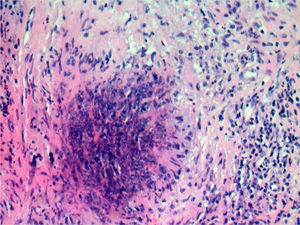
An evaluation by the Rheumatology Department of our center was requested and, suspecting GPA, a prostate biopsy was performed, the pathologic diagnosis being necrotizing epithelioid granuloma and vasculitis of a Wegener type (Fig. 1). Treatment with methylprednisolone was established 40mg/8h iv and cyclophosphamide 100mg/24h vo, increasing to 150mg/24h 5 days later, with disappearing symptoms and a reduction of the prostatic volume to 34cm3. The suprapubic cystostomy was removed to recover spontaneous voiding, with postvoid residue less than 50cm3. Analytically, the c-ANCA became negative.
The patient was discharged with prednisone 60mg/day and cyclophosphamide 150vomg/vo day. He presented systemic recurrence 4 months later, coinciding with the decrease in corticosteroid treatment.
Twelve months into the process, while in remission, we replaced cyclophosphamide for azathioprine due to its better toxicity profile and, 6 months later, for methotrexate, reaching the target of a 20mg/week dose, gradually reducing prednisone to 12.5mg/day, while the patient remained asymptomatic. We made the changed from azathioprine to methotrexate because of the latter's better dosaging profile upon request by the patient, to ensure compliance.
CommentsThe urological manifestations of extrarenal GPA are uncommon, especially in isolation, and in most cases are associated with concomitant renal injury, or may precede the clinical manifestation of the disease, making diagnosis difficult. The prostate is the most frequently genitourinary organ involved (2%–7.4%) after the kidney, but onset with urinary symptoms is rare.5 There is also sporadic involvement of the testicles, bladder, seminal vesicles, urethra, penis, ureter, and adrenal glands6 (Table 1).
Review of the Literature (PubMed) on Urogenital Manifestations of Wegener Granulomatosis (Wegener AND Prostatitis AND Urogenital Manifestations).
| Ref no. | 1st author. Year | No. patients in the series | Urogenital and GPA initial manifestation (no. patients) | Urogenital manifestation in the course of the GPA (no. patients) | Urogenital recurrence in GPA (no. patients) | Urogenital symptoms (no. patients) |
| This work | Pereira J. 2013 | 1 | 1 | Prostatitis (1) | ||
| 12 | Dufour JF. 2012 | 11 | 2 | 9 | 6 | Prostatitis (4)Orchitis (4)Epididymitis (1)Renal pseudotumor (1)Urethral stricture (1)Penile ulcers (1) |
| 11 | Charlier C. 2009 | 113 | 4 | Prostatitis (4) | ||
| 13 | Awadh B. 2006 | 1 | 1 | Prostatitis (1) | ||
| 14 | Helmann F. 2006 | 1 | 1 | Prostatitis (1) | ||
| 15 | See CQ. 2005 | 1 | 1 | Prostatitis (1) | ||
| 16 | Brunner A. 2004 | 1 | 1 | Prostatitis (1) | ||
| 17 | Minee RC. 2009 | 1 | 1 | Orchitis (1) |
The diagnosis of GPA is performed by a combination of clinical and histological data. The initial and characteristic involvement of the upper and lower airways and the subsequent development of glomerulonephritis of varying severity leads the clinician toward the diagnosis. However, a biopsy of the affected organ, and visualization of lesions of necrotizing granulomatous vasculitis, is essential to confirm the diagnosis.
High titers of c-ANCA were identified in 88% of patients with active disease. The finding of high levels of c-ANCA shows a sensitivity of 41%–96% depending on the degree of activity, and a specificity of 99%, in the diagnosis of GPA.2,7
ANCA are a group of autoantibodies, mainly IgG, directed against antigens which are present in the cytoplasm of the neutrophil granulocytes and in the cytoplasm of monocytes, and which are particularly associated with systemic vasculitis. pANCA or perinuclear fluorescence pattern are cytoplasmic autoantibodies against myeloperoxidase (anti-MPO). c-ANCA fluorescence or cytoplasmic pattern autoantibodies are specific against serine proteinase-3 (anti-PR3).
Plasma levels of c-ANCA can be used as immunological (not biochemical) markers of the disease, although they not always have a parallel course to activity.8 They can be used for: monitoring response to treatment, diagnosis of recurrence, determining disease progression and identification of patients who achieved a complete remission, as this is one area where negativisation of antibody titers occurs, although 43% of patients with a complete clinical remission show some degree of positive c-ANCA.8
It is common to find changes in other laboratory tests: elevated ESR, hypergammaglobulinemia and elevated rheumatoid factor, and laboratory abnormalities features that reflect dysfunction of the organs affected by the disease.
In the patient in our case, c-ANCA positivity was a valuable piece of data for diagnosis because of the limited nature of the disease, with no clinical features present as in most patients with GPA. Ultrasonography was not useful for diagnosis, as it only allowed to visualize the existence of an enlarged prostate, which by its sonographic features was indistinguishable from an infectious process at this level, although it was useful for monitoring9 (Fig. 2).
The differential diagnosis is made with infectious processes such as tuberculosis, atypical mycobacterial infection, brucellosis, fungal infections, syphilis and parasitic infections leading to necrotizing granulomatous lesions similar to Wegener's granulomatosis. In our patient, no infectious agent was identified in cultures. This data, together with high titers of c-ANCA, allowed us to diagnose Wegener's granulomatosis.
Therapy of GPA has two components: induction of remission with initial immunosuppressive treatment and maintenance immunosuppressive therapy for a variable period to prevent relapse. The induction of remission is usually accomplished through the combination of glucocorticoid and cyclophosphamide. Glucocorticoids are often administered for 6 months, while treatment with cyclophosphamide is longer, up to one year after complete remission. Other agents used are azathioprine, trimethoprim-sulfamethoxazole and methotrexate.10 Trimethoprim can be useful and beneficial in localized GPA, especially during phases of remission induction and maintenance, and in infections by Staphylococcus aureus or Pneumocystis jirovenci in secretions from the upper respiratory tract. Chemoprophylaxis with cotrimoxazole is used to prevent systemic infections secondary to the use of immunosuppressive drugs.11
Current therapeutic regimens allow for remission rates exceeding 90% in larger series, although 25%–30% of these patients experience a recurrence in the long-term.
Our patient was treated by combining glucocorticoids and cyclophosphamide, with rapid resolution of urological symptoms and complete remission 3 months after starting treatment, demonstrated by the disappearance of symptoms and a negative c-ANCA result, showing early extraurological recurrence after reducing corticosteroid treatment.Surgical treatment, such as transurethral resection of the prostate, is reserved for patients with persistent clinical manifestations despite medical treatment, although cases where nephrectomy or radical prostatectomy for suspected carcinoma was performed have been described. In our case, the patient required suprapubic cystostomy for acute urinary retention.12
ConclusionsProstatitis as the initial presentation of GPA is a rare entity. Prostatitis should be suspected in those patients with poor outcomes despite adequate empiric treatment, negative cultures and malaise. Positive c-ANCA titers guide the diagnosis and help monitor treatment and evolution. Immunosuppressive drugs such as glucocorticoids and cyclophosphamide are the treatment of choice for moderate forms.
Ethical ResponsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of InterestThe authors have no conflicts of interest
Please cite this article as: Pereira Beceiro J, Rodríguez Alonso A, Bonelli Martín C, Pérez Valcárcel J, Mosquera Seoane T, Cuerpo Pérez MÁ. Prostatitis y retención aguda de orina como comienzo de granulomatosis de Wegener. Reumatol Clin. 2014;10:409–412.