For the purpose of assessing the impact of ultrasound in patients with acute shoulder pain, we conducted an analysis of quality health care indicators: need for reevaluation of the pain, rate of referral to specialized medicine and length of time in the emergency department. We reviewed the 1433 records of patients attended to between 2015 and 2016.
Thirty days after the first examination, 90 patients (10.1%) had returned to the control group (56 through the emergency department and 34 because of the), whereas, in the ultrasound (US) group, 14 (2.5%) had returned at least once (12 through the emergency department and 2 because of the PCC) (P<.001). The rate of referral to specialized medicine in the control group was 36.5%, whereas in the US group it was 6.21% (P<.0001). The average length of stay was 94.5 (standard deviation [SD] 34.3) minutes in the control group and 105.4 (SD 40.1) minutes in the US group (P<.0001). Our results suggest that the practice of shoulder ultrasound improves health care quality in these patients, at the cost of a slight increase in health care time.
Con el fin de valorar el impacto de la ecografía en pacientes con dolor agudo de hombro realizamos un análisis de indicadores de calidad asistencial: necesidad de reevaluación por dolor, tasa de derivación a consulta especializada y tiempo de estancia en urgencias. Se revisaron los 1.433 registros de pacientes atendidos entre 2015 y 2016.
A los 30 días de la primera valoración, 90 pacientes (10,1%) habían reconsultado en el grupo control (56 por urgencias y 34 por AP), mientras que en el grupo ECO habían reconsultado 14 (2,5%) al menos una vez (12 por urgencias y 2 por AP) (p<0,001). La tasa de derivación a especializada en el grupo control fue del 36,5%, mientras que en el grupo ECO fue del 6,21% (p<0,0001). El tiempo de estancia media fue de 94,5 (DE: 34,3) minutos en el grupo control y de 105,4 (DE: 40,1) minutos en el grupo ECO (p<0,0001). Nuestros resultados sugieren que la práctica de ecografía de hombro mejora la calidad asistencial de estos pacientes a costa de un discreto incremento en los tiempos de atención.
The diagnostic value and usefulness of musculoskeletral ultrasound in shoulder pain of non traumatic origin is recognized within our speciality1,2 and is extensively used as a diagnostic tool in our practice.3 However, assessment of a painful shoulder of recent onset is usually performed within a primary care environment or in hospital emergency units.
Unlike protocolised ultrasound for polytraumatised patients which has been widely used in emergency units during the last decade and is known as “point of care” or POCUS,4,5 the availability of locomotor system ultrasound and training in this technique is currently much more limited and experience with records is occasional and confined to very few centres at emergency department levels.6 As with any other diagnostic or therapeutic intervention measure, the value of ultrasound of the shoulder must be measured according to direct objective care variables (satisfaction surveys, waiting times) or indirect (generation of referrals, high resolution or the need for reassessments).7
Our hypothesis is that using ultrasound as a diagnostic tool in assessment of patients with acute painful shoulder has a positive effect in terms of reducing the need for further urgent assessments, referrals and waiting times.
MethodA descriptive, retrospective and cross-sectional study based on records of patients regularly attended for locomotor system pathologies in our emergency unit was conducted. Three care quality indicators were chosen arbitrarily. One was direct and two indirect. The direct marker was the length of stay in the emergency department. The two indirect markers were the need for reassessment of pain and the corresponding survival rate when this need was not present, and the rate of referral to a specialist.
The records of all patients attended for acute omalgia between 2015 and 2016 were reviewed. Acute omaliga is understood to be: all shoulder pain which has not lasted for over 3 weeks. Only those omaligias where no traumatic event was recorded to be directly related with pain onset were included. All patients who had been originally attended by the trauma unit according to the triage system criterion of our centre were excluded. All direct or non direct accidental contusion which had taken place in the region of the painful shoulder was considered a traumatic event. Once the records had been identified, they were grouped according to whether use had been made or not of the ultrasound as a diagnostic or a diagnostic and therapeutic tool. All imaging interpretations were made in accordance with applicable current European recommendations and definitions.8,9
Information on waiting times was obtained using the electronic patient admission register which is accessed using the electronic management system of clinical records. Waiting time in the emergency unit was considered to be the period of time—measured in minutes—from when medical care began up until when the patient was discharged. To determine the need for pain reassessment and the rate of referral to a specialist the overall clinical file of the patient was consulted, with identification of further visits to the emergency services within the health area of the autonomous community using the IT tools HORUS® and CAJAL®. For statistical analysis the Student's t-test, the exact Fisher test and the survival curve (waiting time in emergency department, rate of referral to specialist and need for reassessment of pain, respectively) were used.
As part of the medical care in the emergency services, patients were informed of the possibilities of returning due to the persistence of symptoms, worsening of symptoms or side effects from medication. Equally, patients received a written report from the doctor's surgery which included—when there was one—the corresponding ultrasound report.
This study forms part of a research project in epidemiology and management of mulsculoskeletral pathology approved by the Ethics Committee of Scientific Research of our hospital (File 151/16).
ResultsOnce 62 patients had been excluded, 1433 patient records were assessed during the stated period. Of these, 547 (38.1%) were assessed with ultrasound care (ECO group), from which 2 assessments were made by a radiologist and the remainder by a trained specialist (rheumatologist or GP, both with specific training in musculoskeletal ultrasound and with not under 3 years of experience carrying out these tasks). The remaining assessments, 886 (61.8%), were made without the use of the ultrasound (control group), although in 540 cases, a shoulder X-ray was made. No differences in demographical and epidemiological characteristics between the two groups were made, with exception of the proportion of patients who had previously been consulted in their respective primary care centres (Table 1).
Demographic and epidemiological characteristics of the patients whose records were included.
| Variable | US group (n=540) | Control group (n=886) | P value |
|---|---|---|---|
| Age±SD (years) | 55.6±8.3 | 56.7±9.3 | .0243 |
| Women, n (%) | 365 (67.5) | 560 (63.2) | .0923 |
| Time from symptom onset±SD (days) | 7.6±4.8 | 7.9±4.1 | .2096 |
| Patients who had consulted previously in primary care attention, n (%) | 115 (21.2) | 146 (16.4) | .0224 |
| Medical specialty responsible for emergency care, n (%) | >.05 | ||
| Rheumatologist | 288 (53.3) | 451 (50.9) | |
| GP | 216 (40) | 405 (45.7) | |
| Other specialist | 36 (6.6) | 30 (3.3) | |
SD: standard deviation; US: ultrasound.
No pathologies were identified in 39 ultrasounds (7.1%). Of this group, 6 corresponded to chest pains which spread to the shoulder, 5 to neuropathies of paravertebral origin and in 28 cases no diagnostic was established. Of the remaining 508 records, in 104 (20.4%) straining of the subacromial, subdeltoid or both bursas was determined. In 380 patients (74.8%) a pathology in the supraspinal tendon was determined, in 130 (25.5%) in the subscapular tendon, in 112 (22%) in the long arm of the biceps tendon and in 4 (.7%) in the infraspinatous tendon. The most frequent lesion in rotor cuffs was tendinosis without sinew tear in 315 cases (62%), followed by sinew tears in 111 cases (21.8%) and calcifications in 96 cases (18.8%). In 9 patients (1.7%) there was straining of the posterior recess at labrum level was determined.
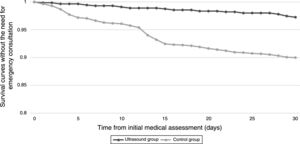
Prior to the 30 days of the first assessment, 90 patients (10.1%) had re-consulted in the control group (56 in the emergency department and 34 in primary care), whilst in the ECO group 14 had re-consulted (2.5%) at least once (12 from the emergency department and 2 from primary care), (P<.001). The difference between the patient survival rates of both groups according to the Kaplan–Meier comparison curve had a Z value of=5.17, P<.01 (Fig. 1). The referral rate to the specialist in the control group was 36.5%, whilst in the ECO group it was 6.21% (P<.0001). The number of referrals to shoulder surgery was 9 and they all came from the ECO group. Six of the patients were referred for tendon tear and 3 for subacromial obstructions. Mean stay was 94.5 (SD: 34.3) minutes in the control group and 105.4 (SD: 40.1) minutes in the ECO group (P<.0001).
ConclusionsAccording to different epidemiological studies, locomotor system pathologies are one of the most frequent causes to require emergency consultation.10–12 The direct healthcare burden is obvious, whilst its indirect impact is difficult to measure due to the fact that many different variables are involved which include length of disability, costs of additional tests, disabilities, new appointment generation, along with many other factors.13,14
This study had the following limitations. On the one hand, due to the characteristics of its design, it was not possible to assess the level of satisfaction of users in terms of a Likert type scale. Although this is a subjective method and probably impressionable due to the mere effect of the use of diagnostic apparatus, it is an easily interpretable assessment and enables comparison to be made outside the local environment. Other interesting variables are the effect of management in terms of changes in the perception of pain or the functionality of the shoulder. Both measurements can be made through immediate and short-term scales. Furthermore, we cannot necessarily attribute all the differences found between the groups exclusively to the fact of carrying out an ultrasound assessment or not, since the study included data obtained from the exercise of regular clinical practice and that which is subject to the decision. However, it is more probable that the patients who were clinically more complex had been assessed with help from the ultrasound, and the differences observed could therefore be underrated.
Shoulder pathology attended to through the emergency services has epidemiological characteristics which distinguish it from the pathology we are used to dealing with in consultations with specialists.15 This explains, for example why referral rates for shoulder surgery were particularly low, since the degenerative pathology as origin for emergency consultation is not as frequent as it could be in specialized consultation. Moreover, the use of ultrasound as a diagnostic tool in this pathology appears to be reasonably effective1 and access to ultrasounds in hospital emergency and outpatients departments is increasingly greater, although no objective data exists in our environment. Like with any tool, prior to recommending usage we need to demonstrate that it has a favourable impact on patient care and for this we cannot do without indicators. We should also mention that ultrasound is a tool that depends on the user and the results of which also depend on the quality of the equipment used. Furthermore, it is the surgeon's job to decide whether a nuclear magnetic resonance is required prior to the planning of surgery resulting from an ultrasound outcome.
Our study shows a notable reduction in the rate of referrals to specialists and the need for further re-assessments within a period of 30 days from the first clinical assessment. Previous studies carried out in the same environment show that repeated consultations for musculoskeletal pathologies are the greatest cause of overburden in emergency departments. In contrast, waiting time in the emergency department significantly increased, although with a difference of around 10min.
A reduction in the need for referrals to specialists and a higher rate of survival without the need for further consultations justify a higher use of musculoskeletal ultrasound as a diagnostic tool in patient care units of those who consult due to emergency. For this extension it is probable that useful measures would be the opening of direct channels between the rheumatology departments and emergency departments, with the consequent higher provision of specialists with training in this technique. Thus the growth and development point of care ultrasound (POCUS) is having in the emergency services and which has demonstrated considerable improvements in care quality,5 could also begin to be seen in the globalization of musculoskeletal ultrasound as an available tool for patients for attend emergency services.
Conflict of interestsAll the authors have no conflict of interests to declare.
Please cite this article as: Guillén Astete C, Rodrigo González S, Alfonso Pérez D, Luque Alarcón M, Penedo Alonso R, Estévez Rueda MJ. Calidad asistencial en el hombro doloroso agudo: ¿qué aporta la ecografía musculoesquelética? Reumatol Clin. 2020;16:290–293.