Infectious arthritis is a medical emergency whose prognosis, in terms of general morbidity and the final functionality of the joint, depends on rapid diagnosis and treatment. The sternoclavicular joint is an area of low prevalence of this type of arthritis, although its frequency is often concentrated in immunosuppressed patients, users of parenteral drugs or after traumatic events. We present a series of 5 microbiologically documented cases of sternoclavicular septic arthritis, 3 of which occurred in immunocompetent patients, and a short review of this pathology.
La artritis infecciosa es una urgencia médica de cuyo rápido diagnóstico depende el pronóstico a corto y medio plazo del estado general del paciente y de la funcionalidad final de la articulación. La articulación esternoclavicular es una región de baja prevalencia de este tipo de artritis, aunque su frecuencia se suele concentrar en pacientes inmunosuprimidos, usuarios de drogas parenterales o tras procedimientos traumáticos. Presentamos una serie de 5 casos microbiológicamente documentados de artritis infecciosa esternoclavicular, 3 de los cuales se presentaron en pacientes inmunocompetentes, y una revisión de esta peculiar enfermedad.
Septic arthritis of native joints (NJSA) often poses a diagnostic problem as its cardinal clinical semiology is comparable to that of other forms of arthritis.1,2 Also, certain topographical locations make it difficult to recognize because of the poorly distensible nature of some synovial joints, low inflammatory permeability or because they are certainly uncommon. This is the case of septic arthritis of a sternoclavicular joint, in which infectious disease is considered very rare,1,3 and which, moreover, has been associated with immunosuppression situations, neoplasia or secondary metabolic deficiency states.2–6
Clinical ObservationWe present a series of 5 cases of sternoclavicular NJSA diagnosed in the emergency department of our hospital between 2012 and 2013, but none of which have been previously included in other series (Table 1).
Demographic Overview, Additional Tests and Management-Development.
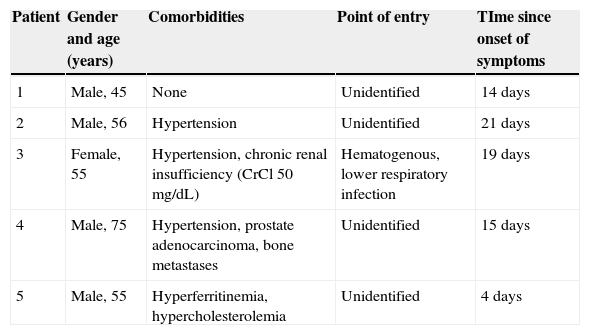
| Patient | Gender and age (years) | Comorbidities | Point of entry | TIme since onset of symptoms |
|---|---|---|---|---|
| 1 | Male, 45 | None | Unidentified | 14 days |
| 2 | Male, 56 | Hypertension | Unidentified | 21 days |
| 3 | Female, 55 | Hypertension, chronic renal insufficiency (CrCl 50mg/dL) | Hematogenous, lower respiratory infection | 19 days |
| 4 | Male, 75 | Hypertension, prostate adenocarcinoma, bone metastases | Unidentified | 15 days |
| 5 | Male, 55 | Hyperferritinemia, hypercholesterolemia | Unidentified | 4 days |
| Patient | Leukocytes (% neutrophils) | CRP (mg/L) | X ray of sternoclavicular joint | Ultrasound | CT |
|---|---|---|---|---|---|
| 1 | 12,500 (80) | 240 | No findings | Distension of the joint capsule, PDS signal (+ + +/+ + +) | Sternoclavicular arthritis, sternal osteomyelitis |
| 2 | 16,800 (85) | 188 | Not performed | Distension of the joint capsule, PD signal (+ +/+ + +) | Sternoclavicular arthritis, sternal and clavicular osteomyelitis, sternohyoid myositis and clavicular body of the sternocleidomastoid |
| 3 | 13,400 (85) | 211 | Irregularities in the clavicular cortical side | Distension of the capsule, cortical irregularity, negative PD signal | Sternoclavicular arthritis, myositis of the sternocleidomastoid clavicular body |
| 4 | 12,300 (86.1) | 290 | Not performed | Not performed | Sternoclavicular joint arthritis with effusion without cortical damage. Myositis in the sternocleidomastoid, platysma and prelaryngeal muscles and subcutaneous tissue |
| 5 | 7,550 (78.3) | 391 | Not performed | Distension of the capsule, positive PD signal, presence of periarticular subcutaneous abscess | Sternoclavicular joint arthritis with effusion. Involvement of the clavicular sternocleidomastoid branch. Subcutaneous abscess at the joint surface |
| Patient | Germ isolated | Intravenous treatment | Oral treatment | Progression |
|---|---|---|---|---|
| 1 | Staphylococcus aureus | Cloxacillin, 6wk | Amoxicillin, 4wk | Rapid improvement of the general state and fever on the third day. Complete functional recovery |
| 2 | Staphylococcus aureus | Vancomycin 4wk | Amoxicillin, 4wk | Required surgical debridement. Subsequently, good evolution.Required physiotherapy due to limitation of external rotation of the shoulder and neck with contralateral lateralization |
| 3 | Streptococcus pneumoniae | Cloxacillin, 6wk | Cloxacillin, 6wk | Required surgical debridement. Subsequently, good performance. Required physiotherapydue to limitation of cervical extension and intermediate degrees of rotationin contralateral direction to the lesion |
| 4 | Staphylococcus aureus | Vancomycin metronidazole+3wk | Vancomycin metronidazole +6wk | Favorable recovery |
| 5 | Staphylococcus aureus | Cloxacillin 16 days | Clindamycin, 8wk | Required surgical debridement. Good progression afterward |
CrCl: creatinine clearance of 24h; HT: hypertension; CRP: C-reactive protein; PD: power Doppler signal; CT: computed tomography.
Case 1. Male, 45 years. He consulted for clavicular pain of 2 weeks duration and fever of recent onset with pain and sternoclavicular swelling. Ultrasonography showed capsular distension with intraarticular and periarticular power Doppler signal (PDS). The patient was successfully treated with cloxacillin for 6 weeks and then amoxicillin for 4 weeks. Staphylococcus aureus was isolated both in the synovial fluid (SF) and in the blood culture.
Case 2. Male, 56 years. He consulted for clavicular and cervical pain of 3 weeks of evolution. The point of entry was not identified. One day before admission the patient had high fever and severe fatigue. In the ER we detected fever, tachycardia, and malaise, with a normal blood pressure. On ultrasound we found capsular distension of the sternoclavicular joint with intraarticular PDS (+) identified as well as in the territory of the clavicular sternocleidomastoid. Computed tomography (CT) showed myositis of the sternohyoid and the distal medial clavicular fibers of the sternocleidomastoid branch. It required surgical lavage. Staphylococcus aureus was isolated in blood cultures and SF.
Case 3. 55-year-old woman, who had a mechanic shoulder pain radiating to the collarbone since 19 days earlier. She had been hospitalized about five days ago for pneumonia and, postdischarge, consulted for progressive shoulder pain and fever in the past 2 days, with no respiratory symptoms. Ultrasonography showed capsular distension, cortical irregularities on both sides, with PDS (−) intraarticularly and PDS (+/+ + +) in the fibers of the clavicular sternocleidomastoid body. Surgical lavage was performed and treatment was started with cloxacillin, with a good response. SF Cultures showed Streptococcus pneumoniae.
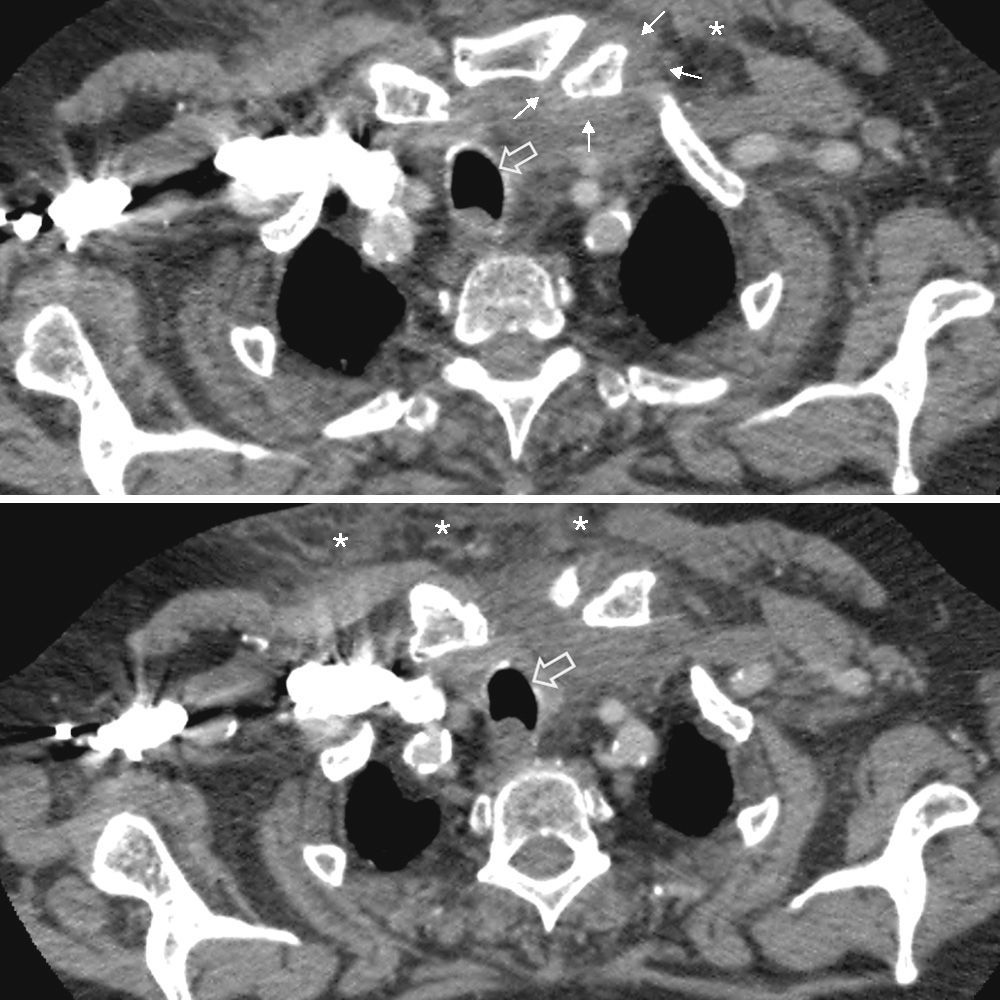
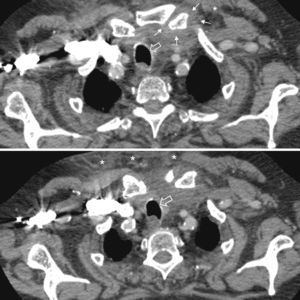
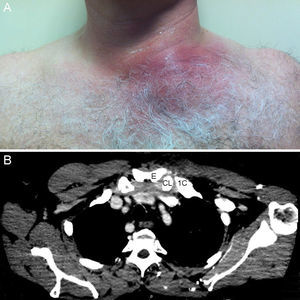
Case 4. Male 75 years, allergic to beta-lactams, diagnosed with actinic proctitis. He consulted for rectal bleeding, fever of 39° C and pain in the cervical region for 2 days. In the ER he developed erythema and edema, as well as pain on palpation of the anterior cervical region. A cervical CT angiography determined swelling of the sternoclavicular joint and the sternocleidomastoid, with protrusion into the premediastinic space (Fig. 1) contacting the brachiocephalic vein. In the SF, Staphylococcus aureus was isolated.
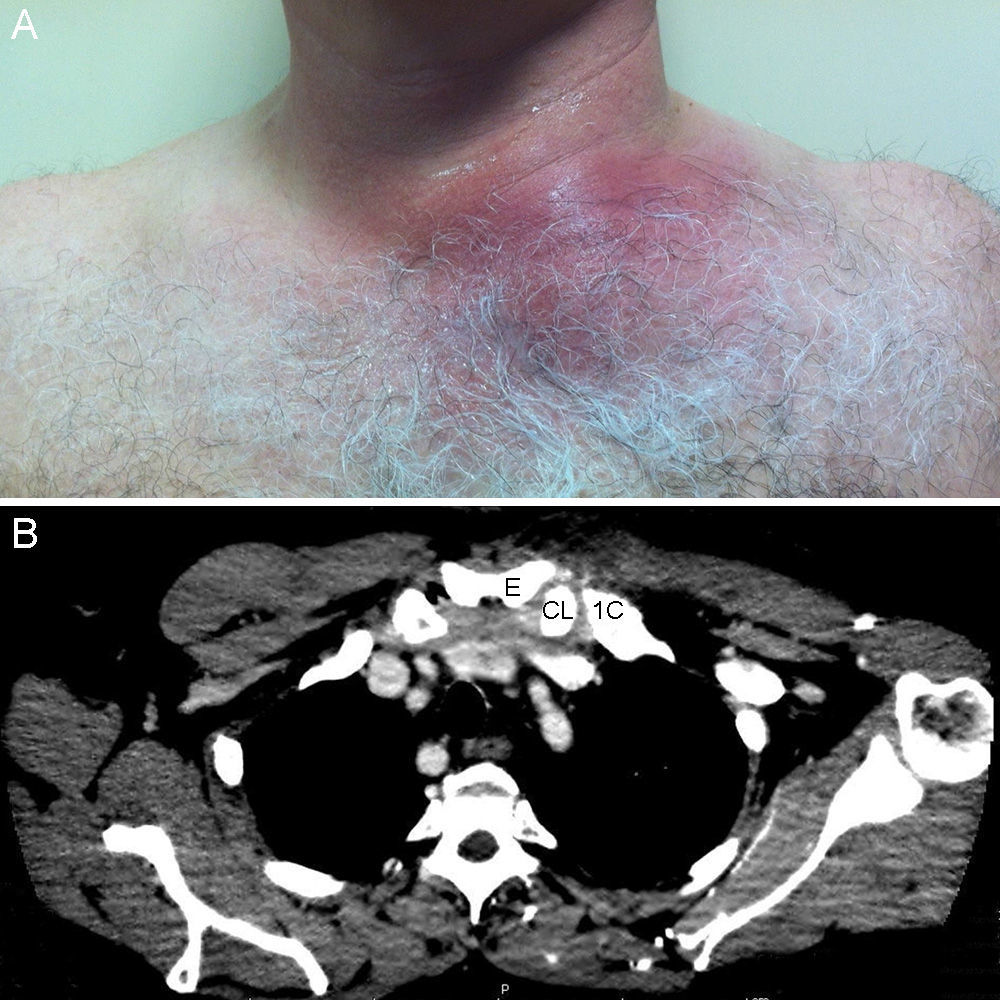
Case 5. Male 55 years. He consulted for a painful swelling of the left chest, of 24h of evolution. Four days before he consulted for atraumatic left shoulder pain. He presented erythematous and painful swelling of the sternoclavicular joint, fluctuating and with sharp edges. Ultrasonography showed capsular distension and PDS (+) both intracapsular as extracapsularly. A superficial abscess of the joint was also identified. A CT scan confirmed the findings and also detected involvement of the distal clavicular sternocleidomastoid body (Fig. 2 Surgical drainage was required. S. aureus was isolated in the culture.
Discussion and ConclusionsSternoclavicular NJSA is an uncommon disease, in both immunocompetent and immunosuppressed patients.1,7 The largest collection of the world's scientific literature includes 170 cases from more than 70 studies published between 1970 and 2004.6 Another more recent compilation published in 2004 collected 15 cases, documented between 1989 and 2012.5 It is usually described in the fourth to fifth decade of life, like other atypical location NJSA.1,4,6 The risk factors identified in the literature are: intravenous drug use, infections at a distance, diabetes mellitus, local trauma, central line infection, chronic renal failure, alcoholism, HIV infection, neoplastic disease and cirrhosis,1–3 Usually it is clinically insidious and can be confused with mechanical neck pain or shoulder pain with clavicular irradiation.1 In our series, the diagnosis is established after the second week of the onset of symptoms, with the exception of case 4. The most commonly used test for diagnosis was ultrasonography, although confirmation and assessment of the cortical scope required a CT. The most common complication in our series was myositis, a situation that requires surgical debridement, prolonged hospital stays and physical therapy due to residual functional limitation. Osteomyelitis has also been reported in other series.8 In ours, osteomyelitis was described mainly in patients with PDS (+) an intraarticular, sonographic sign denoting intense hyperemia.9
The sternoclavicular joint is poorly vascularized, so antibiotic treatment is usually prolonged and management follows a pattern similar to empirical antibiotic therapy of infections of the more common joints affected.2,3
In general terms, the clinical onset in immunocompromised patients is no different from the one presented in immunocompetent patients. In our series, we have seen striking differences in the presentation of clinical symptoms: insidious, referred pain to the neck or shoulder, and fever.1,3 In this sense, we conclude that the situation of immunocompetence should neither rule out the diagnosis nor defer empiric treatment of suspected sternoclavicular NJSA.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients, and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Guillén Astete C, Aranda García Y, de la Casa Resino C, Carpena Zafrilla M, Braña Cardeñosa A, Roldan Moll F, et al. Artritis infecciosa esternoclavicular: serie de 5 casos y revisión de la literatura. Reumatol Clin. 2015;11:48–51.