To know rheumatologists’ opinion on the usefulness of ultrasound in diagnostic and therapeutic decision making as applied to rheumatic diseases.
Materials and methodsA National survey was sent to all rheumatology units in hospitals with at least 200 beds. The questionnaire included: (a) general data, (b) purpose and most common areas of ultrasound exploration and (c) assessment of the usefulness of ultrasound in routine clinical practice in general and in some rheumatologic diseases.
ResultsOne-hundred and sixty-nine out of 234 rheumatology units contacted answered the questionnaire. The utility in routine clinical practice was scored at 7.8 (scale 0–10) and ultrasound was integrated in making diagnostic and therapeutic decisions. Half of the indications (50.9%) were ultrasound related to the process of diagnosis of diseases or treatment decision making (monitoring synovitis 14.6%, guided puncture 11.4%, early detection of joint erosion or synovitis 10.3%, early detection of enthesopathy 5.9%, carpal tunnel syndrome or other peripheral neuropathies 3.4%, detection of uric acid or pyrophosphate deposits 3%, vasculitis 1% and others 1.1%. On a 1–5 Likert, scale most of the answers support the use of ultrasound in clinical practice, especially in diagnostic and therapeutic decision making for detection of subclinical synovitis, erosions and treatment decisions in rheumatoid arthritis, enthesitis diagnosis, crystal diseases, polymyalgia rheumatica and giant cell arteritis.
ConclusionsUltrasound is becoming a useful tool integrated into clinical practice and is linked to the decision-making processes in the areas of diagnosis, activity and treatment.
Conocer la opinión de los reumatólogos sobre la utilidad de la ecografía en la toma de decisiones diagnósticas y terapéuticas en reumatología.
Material y métodosEncuesta nacional, dirigida a todas las unidades de reumatología de hospitales con más de 200 camas. El cuestionario incluía: a) datos generales; b) finalidad y áreas de exploración ecográfica más comunes, y c) evaluación de la utilidad de la ecografía en la práctica clínica habitual en general y en algunas enfermedades reumatológicas en particular.
ResultadosRespondieron al cuestionario 169 unidades de reumatología de las 234 consultadas. La utilidad se valoró en 7,8 (escala 0-10). La mitad de las indicaciones (50,9%) se relacionaban con el diagnóstico de enfermedades o toma de decisiones terapéuticas (monitorización de sinovitis: 14,6%; punción guiada: 11,4%; detección temprana de erosión articular o sinovitis: 10,3%; detección temprana de la entesopatía: 5,9%; síndrome del túnel carpiano u otras neuropatías periféricas: 3,4%; detección de depósitos de ácido úrico o pirofosfatos: 3%; vasculitis: 1%, y otros: 1,1%). En una escala de Likert de 1-5, la mayoría de las respuestas respalda el uso de la ecografía en la práctica clínica, especialmente en la toma de decisiones diagnósticas y terapéuticas para la detección de sinovitis subclínica, erosiones y decisiones de tratamiento en casos de artritis reumatoide, diagnóstico de entesitis, enfermedades de depósito articular, polimialgia reumática y arteritis de células gigantes.
ConclusionesLa ecografía se está convirtiendo en una herramienta útil integrada en la práctica clínica y vinculada a la toma de decisiones en procesos diagnósticos y terapéuticos.
Ultrasound is a recently introduced technique in the specialty of rheumatology. Although there is a historic precedent, ultrasonography came into our environment at the beginning of the nineties. Today, rheumatologists are showing increasing interest in this technique. The number of ultrasonography articles in journals of rheumatology is growing as are the national associations of Rheumatology who provide ultrasound training programs every year. At the beginning of training, rheumatologists are taught the correct standardization for exploring different anatomical areas, as well as the recognition of different tissues, both the normal and the pathological. However, physicians often need to know not only what happens in a local area, but also what happens to the patient in general. In other words, they need to find answers to questions like what disease does the patient have? or what is the degree of disease activity? Recent publications support the idea that ultrasound has the potential to improve the diagnostic and clinical assessment of patients. If so, ultrasound will change usual clinical practice and, in the near future, the way patients with rheumatic diseases are diagnosed and treated, with greater precision and effectiveness, itself an opportunity to improve health care standards. The question is whether this is a mere illusion of a small group of experts or if it is truly generalized and rising among rheumatologists. The answer to this question is relevant, as it could change our health care model and training programs.
During the past 15 years, the Spanish Society of Rheumatology has developed a systematic ultrasound training program and this has been extended and implemented across the country. In fact, more than 800 rheumatologists have been trained through an educational program consisting of 4 levels.1 Thanks to a recent national survey, we know that 90% of the departments of rheumatology of Spain have ultrasound and that 38.7% of rheumatologists use this technique.2 In this sense, our country could be a good model to understand the perception of ultrasound in clinical practice and how it is used in the decision making process. The main objective of this study was to know the opinion of rheumatologists on the usefulness of ultrasound in clinical practice and in the process of making diagnostic and therapeutic decisions.
Materials and MethodsIt created a scientific committee composed of the 4 first authors of the study, which developed the survey questions and set the universe, after determining that Spain has 277 hospitals with more than 200 beds. The invitation to participate was made by email and addressed to the rheumatology units of 234 different centers, though they were not able to locate all of rheumatology departments or their email addresses. The working group on ultrasound of the Spanish Society of Rheumatology (ECOSER) emailed a personalized letter inviting the head of each unit or the person designated as the most suitable, to participate in the survey. After accepting the invitation, an online survey was accessed by an individual user name and password. The questionnaire consisted of 3 parts: (a) general data, (b) purpose and areas of common ultrasound examination, and (c) assessment of the utility of ultrasound in clinical practice in general and rheumatological diseases in particular. Only one answer was allowed per site, within a period between September 15 and October 20, 2011. The data collected were treated in accordance with Organic Law 15/1999, of December 13, Protection of Personal Data.
Descriptive analysis was performed for each variable, with analysis of means, medians and standard deviations where necessary.
ResultsIndications of UltrasoundReplies were received from 169 rheumatology units of the 234 contacted (72%), distributed in 102 areas. The availability of ultrasound equipment was high (90%). A significant percentage of rheumatologists (38.7%) used the scanner and half of the units had a rheumatologist sonographer with special attention to this technique.
Almost half of the ultrasound indications (49.1%) referred to the examination of specific areas (individual joints or soft tissue). Notably, 50.9% of ultrasound examinations were linked to the process of making diagnostic or treatment decisions, for example, ultrasound monitoring of synovial inflammatory activity (14.6%), ultrasound guided needle aspiration (11.4%), early detection of subclinical synovitis or joint erosion (10.3%), early detection of enthesopathy (5.9%), detection of carpal tunnel syndrome or other peripheral neuropathies (3.4%), detection of deposits of uric acid or pyrophosphate (3%), detecting temporal arteritis (1%) and others (1.1%).
Perception on its UsefulnessIn the section that investigated the subjective opinion of the usefulness of ultrasound in clinical practice, respondents noted that on a continuous scale of 0–10 (being 0=no relevance and 10=maximum relevance), the average relevance of the addition of ultrasound to the rheumatology unit was 7.8.
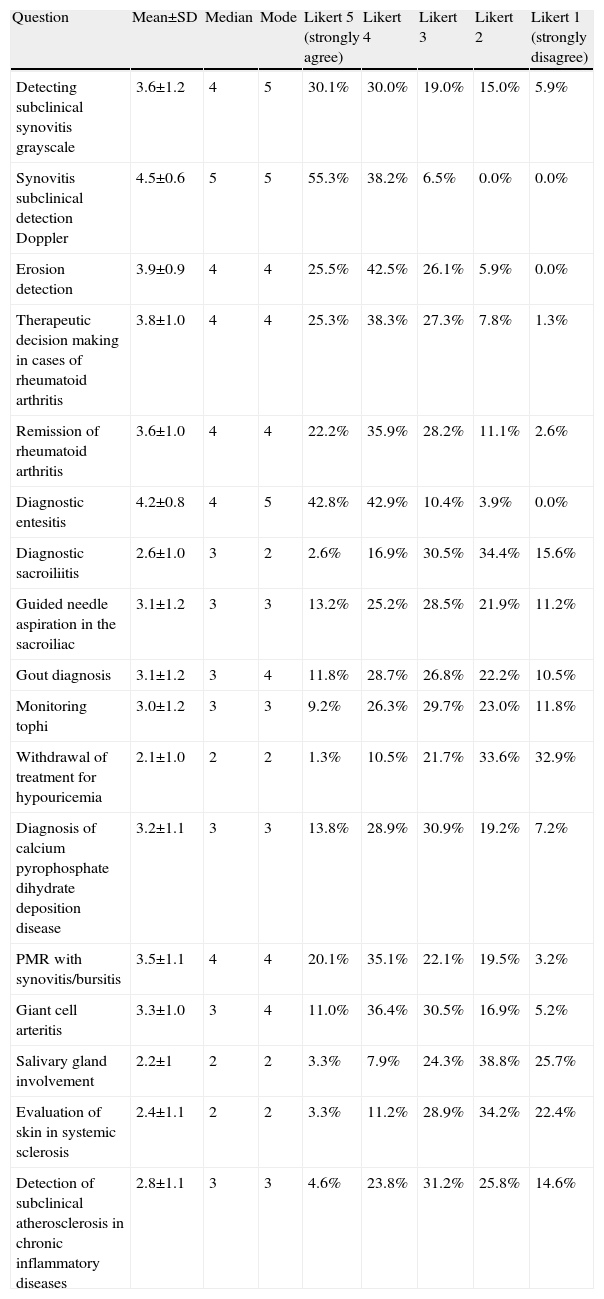
Another important objective of our survey was to ascertain the opinion of rheumatologists on the use of ultrasound in various diseases. Table 1 shows the level of agreement of respondents on a Likert scale (1=strongly disagree, 5=strongly agree) on whether ultrasound should be used in clinical practice in different aspects of diagnostic or therapeutic decision making for various diseases or patient conditions.
Utility of Ultrasound for Making Diagnostic and Therapeutic Decisions in Clinical Practice in Different Conditions.
| Question | Mean±SD | Median | Mode | Likert 5 (strongly agree) | Likert 4 | Likert 3 | Likert 2 | Likert 1 (strongly disagree) |
| Detecting subclinical synovitis grayscale | 3.6±1.2 | 4 | 5 | 30.1% | 30.0% | 19.0% | 15.0% | 5.9% |
| Synovitis subclinical detection Doppler | 4.5±0.6 | 5 | 5 | 55.3% | 38.2% | 6.5% | 0.0% | 0.0% |
| Erosion detection | 3.9±0.9 | 4 | 4 | 25.5% | 42.5% | 26.1% | 5.9% | 0.0% |
| Therapeutic decision making in cases of rheumatoid arthritis | 3.8±1.0 | 4 | 4 | 25.3% | 38.3% | 27.3% | 7.8% | 1.3% |
| Remission of rheumatoid arthritis | 3.6±1.0 | 4 | 4 | 22.2% | 35.9% | 28.2% | 11.1% | 2.6% |
| Diagnostic entesitis | 4.2±0.8 | 4 | 5 | 42.8% | 42.9% | 10.4% | 3.9% | 0.0% |
| Diagnostic sacroiliitis | 2.6±1.0 | 3 | 2 | 2.6% | 16.9% | 30.5% | 34.4% | 15.6% |
| Guided needle aspiration in the sacroiliac | 3.1±1.2 | 3 | 3 | 13.2% | 25.2% | 28.5% | 21.9% | 11.2% |
| Gout diagnosis | 3.1±1.2 | 3 | 4 | 11.8% | 28.7% | 26.8% | 22.2% | 10.5% |
| Monitoring tophi | 3.0±1.2 | 3 | 3 | 9.2% | 26.3% | 29.7% | 23.0% | 11.8% |
| Withdrawal of treatment for hypouricemia | 2.1±1.0 | 2 | 2 | 1.3% | 10.5% | 21.7% | 33.6% | 32.9% |
| Diagnosis of calcium pyrophosphate dihydrate deposition disease | 3.2±1.1 | 3 | 3 | 13.8% | 28.9% | 30.9% | 19.2% | 7.2% |
| PMR with synovitis/bursitis | 3.5±1.1 | 4 | 4 | 20.1% | 35.1% | 22.1% | 19.5% | 3.2% |
| Giant cell arteritis | 3.3±1.0 | 3 | 4 | 11.0% | 36.4% | 30.5% | 16.9% | 5.2% |
| Salivary gland involvement | 2.2±1 | 2 | 2 | 3.3% | 7.9% | 24.3% | 38.8% | 25.7% |
| Evaluation of skin in systemic sclerosis | 2.4±1.1 | 2 | 2 | 3.3% | 11.2% | 28.9% | 34.2% | 22.4% |
| Detection of subclinical atherosclerosis in chronic inflammatory diseases | 2.8±1.1 | 3 | 3 | 4.6% | 23.8% | 31.2% | 25.8% | 14.6% |
SD: standard deviation.
When ultrasound was first used in rheumatology departments, early indications were similar to those in medical imaging departments and we carried out localized examination of shoulders, knees, hands or soft tissue. In fact, most often, only one anatomical region was explored. However, the current standard ultrasound exam may be changing in rheumatology and rheumatologists are going to consider not only what happens to the patient in a particular area, but also on a general level. This could be because, in recent years, numerous articles have been published on the validity of the ultrasound examination in different diseases and conditions.
However, the question is whether such studies are only representative of a small group of researchers not linked to clinical practice, or if they really help rheumatologists to address unmet needs in their practice and if this is changing the clinical routine. Providing an answer to this question was the main objective of our study and we think that in our context, it would be possible to do so.
The survey shows that nearly 50% of the ultrasound examination was performed to diagnose or know the disease activity of our patients. This pattern of use of ultrasound is in accordance with preliminary descriptive data, which suggest that rheumatologists have used this technique to examine more areas per patient and more ultrasounds were performed over small joints, as well as using this technique primarily to contribute to the diagnosis of active inflammation in addition to guiding injections, while less frequently using it to aid in diagnosis of a structural condition and soft tissue.3 Our study, conducted five years later, shows the progress of ultrasound and the use of this technique by rheumatologists not only to improve the diagnosis of our patients, but also to improve treatment decisions, including almost all rheumatic diseases, for example, inflammatory autoimmune diseases, storage articular diseases, vasculitis, spondylitis, systemic sclerosis, disorders of the salivary gland, etc. To our knowledge, this aspect has not been discussed before. Recently, the American College of Rheumatology (ACR) published a report on the reasonable use of musculoskeletal ultrasound in rheumatology clinical practice, using a literature review and a panel of experts.4 Our approach is different in that we turn to the general opinion of rheumatologists in clinical practice as both perspectives can be interesting and complementary.
Another interesting aspect of this research is that the perceived usefulness level differs between the different diseases and, except for some limitations discussed below, are consistent with the evidence.
As a limiting factor of the study, we should mention that this is an opinion poll, which implies a low level of evidence, although it is a good approach to understand what is happening. The analysis of the results might show some bias. In some cases, the results are more optimistic than the published evidence but, in others, the evidence is superior to the perceived utility expressed by the participants in the survey. Finally, another potential bias lies in the influence on the results of the different degree of diffusion of knowledge, courses and conferences on ultrasound on the different diseases.
Perceived usefulness is high for synovitis, which is consistent with evidence from numerous studies published on its validity.5 Ultrasound examination is accepted even in the most recent ACR/EULAR criteria for the classification of rheumatoid arthritis as a valid method for the detection of active synovitis.6 There are also studies showing that ultrasound can detect activity in patients in clinical remission7–9 and this is reflected in the responses.
For the study of entheses there is interesting evidence,10 even in the field of diagnosis11–13 and monitoring response to treatment, and it seems that rheumatologists are aware of such facts,14 although there is still a lot to prove in this field and evidence may be somewhat smaller to the opinions.
Ultrasound examination in joint storage diseases, in giant cell arteritis and polymyalgia rheumatica, has also obtained a positive Likert-scale score between 3 and 4 – and is seen as a useful tool for clinical practice. Perhaps the perception in giant cell arteritis and joint storage diseases is less than the published evidence. In the field of giant cell arteritis, there are 4 metaanalysis,15–17 the highest level of evidence. The limitation may be due to the difficulty to provide training in this technique because of the low prevalence of the disease. In the field of articular storage diseases, the perceived utility is probably less than18,19 the evidence, even in the case of calcium pyrophosphate crystal deposition disease. The proposed new EULAR classification criteria for Calcium dihydrate pyrophosphate deposit disease includes ultrasound as a valid criterion with more evidence than conventional radiology.20 The low level of perceived usefulness in outcomes for vascular atherosclerosis in inflammatory diseases, hypouricemic treatment interruption, the diagnosis of the sacroiliac joint, skin assessment in systemic sclerosis and examination of the salivary glands is due, probably, to the need to incorporate more validity studies to clinical practice in these areas.
When we analyze the time spent to provide training in ultrasound and extend this technique in our country in recent years, we see a potential relationship between support for such training, national conferences and special events with the general perception. In advanced courses, there is a special training on quantification and detection of both synovitis and the enthesis, and in our national congress, we pay special attention to synovitis in rheumatoid arthritis and different sonographic findings in cases of spondylitis and psoriatic arthritis. The perception of lower utility in other conditions with strong evidence, such as joint storage diseases and giant cell arteritis may be due to inadequate dissemination of scientific evidence in these fields. Perhaps, in the future, centers should move parallel to validated data in the literature and special training in advanced courses on ultrasound findings concerning rheumatic diseases at the patient level.
In summary, ultrasound is becoming a useful tool integrated in clinical practice and linked to the decision making processes of diagnosis, activity and treatment. We have detected some discrepancies between evidence and use and it is necessary to maintain a continuous training plan. However, there is no doubt that ultrasound is changing rheumatology.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this research has not been performed on humans or animals.
Confidentiality of dataThe authors state that no patient data appear in this article.
Right to privacy and informed consentThe authors state that no patient data appear in this article.
Conflict of InterestThe authors declare no conflict of interest.
To all rheumatologists who participated in the survey. To Abbvie Spain, for the logistical support provided for this study.
Please cite this article as: de Miguel E, Andreu JL, Naredo E, Möller I, Grupo de Trabajo de Ecografía de la Sociedad Española de Reumatología (ECOSER). La ecografía en reumatología: dónde estamos y hacia dónde nos dirigimos. Reumatol Clin. 2014;10:6–9.