Localized scleroderma is a connective tissue disorder generally involving de entire dermis and usually limited to the subcutaneous tissue; however, it may progress to large indurated plaques, growth retardation, muscle atrophy, and even to flexion deformities or poorly healing ulcers. Unilateral generalized morphea is an extremely rare variant of localized scleroderma which has seldom been reported in the literature. We report the case of a girl who developed unilateral generalized morphea on the right side of the body.
La esclerodermia localizada es una enfermedad del tejido conectivo generalmente limitada a la piel y tejido celular subcutáneo, sin embargo; puede progresar a grandes placas induradas, retraso del crecimiento, atrofia muscular e incluso deformidades en flexión o pobre cicatrización de las heridas. La morfea generalizada unilateral es una variante rara de la esclerodermia localizada descrita ocasionalmente en la literatura. Presentamos el caso de una niña con morfea generalizada unilateral que afectó el lado derecho del cuerpo.
Localized scleroderma, known as morphea, includes a group of different conditions that affect the skin and subcutaneous tissue. It ranges from small plaques affecting the skin to disease which may cause functional and cosmetic deformity, with a variety of extracutaneous manifestations.1 Commonly, localized scleroderma has been divided into 3 groups: morphea, generalized morphea and linear scleroderma. In 2004, the European Society of Pediatric Rheumatology proposed new criteria for the classification of localized juvenile scleroderma and included 5 subtypes: circumscribed morphea, linear scleroderma, generalized morphea, pansclerotic morphea and mixed scleroderma (when a combination of 2 or more of the above are present).1,2 Unilateral generalized morphea us a variant of linear scleroderma in childhood.3
Clinical PresentationA 12-year-old girl came to our hospital in February 2010 due to affection of the right median nerve that required decompressive emergency surgery and, a month later, debridement of the wound and a skin graft. 4–5 months prior, after minimal trauma, she presented pain, swelling and limitation of right hand movements. These symptoms increased without improving and were accompanied by hypopigmented lesions of the same hand, progressively extending to the lower right limb, accompanied by skin thickening. The patient did not use topical drugs or toxins.
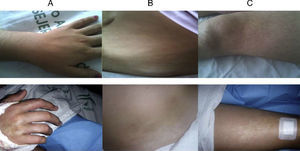
Physical examination showed limitations in flexion of the right hip and knee, flexion contracture of the right hand and hypo/hyperpigmented mottled lesions on the right side of the trunk and upper and lower extremities (Fig. 1), with a diffuse increase in the consistency upon palpation, with the rest of the examination being normal.
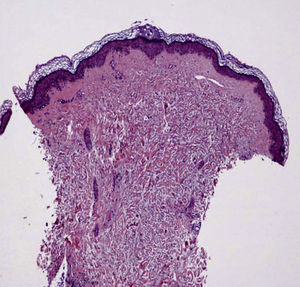
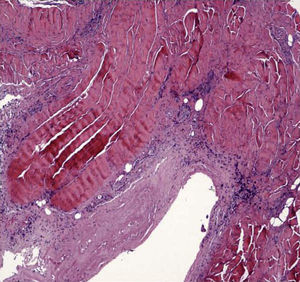
Laboratory testing showed erythrocyte sedimentation rate of 47mm/h, a polyclonal increase in gammaglobulins, thyroid stimulating hormone 5.85μU/ml; autoimmunity: ANA+ with a titer of 1/320, speckled pattern, antihistone +, Scl-70, PMScl, ku, dsDNA, etc., negative. The complete blood count, serum chemistry and muscle enzymes were normal. Rheumatoid factor and arthritis serology (parvovirus, Brucella, Borrelia, etc.) were negative. Chest and bone X-rays (hands, feet, sacroiliacs) were normal. Magnetic resonance of the right carpus (prior to hospitalization) showed proliferative tenosynovitis with synovial hyperplasia. Ultrasound of the right thigh showed discrete diffuse edema of the subcutaneous tissue. A skin biopsy of the right thigh showed skin thickening with disorganized collagen fibers extending to the subcutaneous tissue. Follicles and sebaceous glands showed atrophy, as well as a moderate inflammatory infiltrate with a perivascular disposition (Fig. 2). A biopsy of the flexor right carpal retinaculum at the moment of surgery showed fibrous aponeurotic tissue and striated muscle in a fibrous collagen stroma accompanied by a mononuclear inflammatory infiltrate, predominantly perivascular (Fig. 3). Ecography showed mild mitral insufficiency with no evidence of pulmonary hypertension. Respiratory function tests were normal.
Treatment with pulse 6-MP (750mg) for 3 consecutive days was started and then prednisone (10mg/day) was associated to oral methotrexate (15mg/week), in addition to physiotherapy for softening of the skin lesions and improvement of joint contractions. Currently, after 6 months of therapy, there is no functional limitation for school or home activities.
DiscussionScleroderma is an autoimmune connective tissue disease, characterized by fibrosis of the skin, which can be localized or systemic (involving one or more internal organs).2 Rather than representing two separate entities, this may represent the extremes of a disease continuum.1 To our knowledge, only 6 cases of unilateral generalized morphea have been described in the literature: 5 young adults3,4 and 1 infant.5 These, and our case share some characteristics, such as early onset, unilateral involvement and positive ANA. Furthermore, in our case we found anti-histone antibodies, which are detected in 47% of patients with localized scleroderma and a higher prevalence of generalized morphea1and appear to be related to the severity of the disease and joint contractures.6,7 Thus, our case had carpal tunnel syndrome and contractures, something that is not described in others. Regarding the treatment of localized scleroderma, when there is a significant risk of functional disability or extensive joint involvement of the skin, systemic treatment is recommended. Although no controlled studies exist, there is extensive experience with methotrexate.1 Combined treatment with MP pulses and low-dose methotrexate was used in our case, and the four described3; an adult was treated with oral corticosteroids at high doses associated with methotrexate,4 and one child with topical steroid,5 all with good response. Although the etiology of localized scleroderma is unknown, triggers such as trauma, infection with Borrelia burgdorferi, etc.8 have been described. In our case we identified mild trauma, and in another young adult, exposure to silica and vibration in the hand ipsilateral to sclerosis, but the possible role of these factors is not clear in localized scleroderma.
DisclosuresThe authors have no disclosures to make.
Please cite this article as: Fernández Rodríguez AM, et al. Morfea generalizada unilateral: un caso y revisión de la literatura. Reumatol Clin. 2011;7(6):404–6.