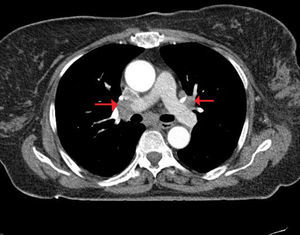
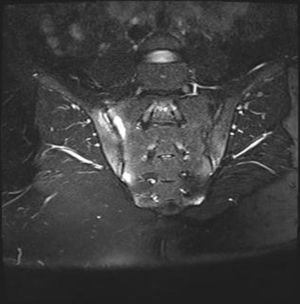
Sarcoidosis is a systemic disease characterized by the involvement of multiple tissues and organs with a non-calcified granuloma reaction, which is not yet well understood.1 Although the exact pathogenesis of sarcoidosis is not known, it is currently accepted that, in genetically susceptible individuals, it is caused through alteration of the cellular immune response after exposure to an environmental, occupational or infectious agent.2 It is presented with bilateral hilar lymphadenopathies, infiltrations in the lung, skin and eye lesions. The pathognomonic histological finding is the presence of non-calcified granulomas.3 These granulomas may form in almost any organ in the body. Sarcoidosis is one of the most important causes of granulomatous lymphadenitis.4 Development of lymphedema is the result of the involvement of lymph nodes and obstruction of lymphatic drainage. In this report we present a female case of sarcoidosis and ankylosing spondylitis co-occurrence that applied to our clinic with widespread lymphedema on her left leg. The patient is 50-year-old female who presented to our clinic with lymphedema and swelling started from the left inguinal region and spread to the whole left lower extremity. She had also complaints of inflammatory low back pain going on for the last 15 years. In her physical examination there was widespread lymphedema on her left foot, lymphadenopathies on her left inguinal region, restriction on her neck and hip range of motion and bilateral Fabere/Fadir test positivity. Laboratory studies showed erythrocyte sedimentation rate and C-reactive protein elevation, serum calcium and angiotensin converting enzyme (ACE) elevation and chronic disease anemia. There were widespread conglomerate lymphadenopathies in the left inguinal region according to the soft tissue ultrasonography examination. Thorax CT showed paratracheal, mediastinal and bilateral hilar lymphadenopathies (Fig. 1). Sacroiliac joint radiography showed bilateral joint space narrowing and sclerosis. Sacroiliac MRI scan was reported as chronic sacroiliitis with the presence of active lesions (Fig. 2). Genetic analysis showed that HLA-B27 was positive. Biopsy of the inguinal lymphadenopathies revealed granulomatous lymphadenitis and non-calcified granulomas. M. tuberculosis was not detected owing to her PPD was negative, acid-fast stain on tissue samples from the biopsy was negative. According to clinical, laboratory, histopathological and radiological findings, we diagnosed our patient as sarcoidosis and ankylosing spondylitis, then she received 40mg of prednisolone per day. Lower extremity edema, inguinal lymph nodes and clinical complaints regressed during the follow up period. Control erythrocyte sedimentation rate and C-reactive protein were normal. Control thorax CT showed significant diametric regression of the hilar and bilateral mediastinal lymph nodes. Sarcoidosis may imitate different rheumatologic diseases and/or may be seen with them.5 Sacroiliac joint involvement is a major joint involvement of sarcoidosis and it may be seen in 6–14% of the patients which causes the diagnostic confusion with ankylosing spondylitis.6,7 HLA-B27 is helpful for the differential diagnosis besides the major method is the histopathological evaluation. Even if it is rare; like in our case, these two diseases may occur together. However this co-occurrence is not because of a common etiopathogenesis, but because of an incidental association. Granulomatous lymphadenitis is an important finding of sarcoidosis.8 The lymphadenopathies that develop in different regions cause organ and system dysfunctions. There are some reported sarcoidosis patients in the literature that were presented with lymphedema. Putkonen et al. has identified a female case that started with lower extremity lymphedema and they reported significant regression after treatment with corticosteroids.9 Nathan et al. reported a 32-year-old black female case that suffered from foot lymphedema going on for the last 11 years.10 As in our case, the lymphedema development on these patients feet is because of the obstruction of the lymphatic drainage due to the involvement of the lymph nodes. Chronic, asymmetric feet edema presentation without venous obstruction should always suggest the probability of sarcoid lymphadenopathy for early diagnosis and treatment of this clinical condition. In conclusion, granulomatous lymphadenitis is an important clinical presentation of sarcoidosis. Different clinical findings may occur because of the compression of the conglomerated lymph nodes. For patients presented with compressive peripheral lymphadenopathy, sarcoidosis is a disease that should be kept in mind.
The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2025
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more