Electronic medical records databases use pre-specified lists of diagnostic codes to identify fractures. These codes, however, are not specific enough to disentangle traumatic from fragility-related fractures. We report on the proportion of fragility fractures identified in a random sample of coded fractures in SIDIAP.
MethodsPatients≥50 years old with any fracture recorded in 2012 (as per pre-specified ICD-10 codes) and alive at the time of recruitment were eligible for this retrospective observational study in 6 primary care centres contributing to the SIDIAP database (www.sidiap.org). Those with previous fracture/s, non-responders, and those with dementia or a serious psychiatric disease were excluded. Data on fracture type (traumatic vs fragility), skeletal site, and basic patient characteristics were collected.
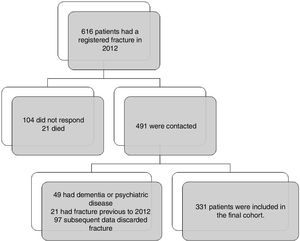
ResultsOf 491/616 (79.7%) patients with a registered fracture in 2012 who were contacted, 331 (349 fractures) were included. The most common fractures were forearm (82), ribs (38), and humerus (32), and 225/349 (64.5%) were fragility fractures, with higher proportions for classic osteoporotic sites: hip, 91.7%; spine, 87.7%; and major fractures, 80.5%. This proportion was higher in women, the elderly, and patients with a previously coded diagnosis of osteoporosis.
ConclusionsMore than 4 in 5 major fractures recorded in SIDIAP are due to fragility (non-traumatic), with higher proportions for hip (92%) and vertebral (88%) fracture, and a lower proportion for fractures other than major ones. Our data support the validity of SIDIAP for the study of the epidemiology of osteoporotic fractures.
La historia clínica informatizada utiliza una lista de códigos diagnósticos pre-especificados para identiticar fracturas, pero estos códigos no permiten distinguir entre fracturas traumáticas y fracturas por fragilidad. Se reporta la proporción de fracturas por fragilidad identificadas en una muestra aleatorizada de fracturas codificadas en SIDIAP.
MétodosEstudio observacional retrospectivo realizado en 6 centros de atención primaria que contribuyen a la base de datos SIDIAP (www.sidiap.org). Se seleccionaron pacientes ≥50 años con cualquier fractura registrada en 2012 (mediante códigos CIE-10) que permanecieran vivos en el reclutamiento y excluyendo aquellos con fractura previa, contacto imposible o aquellos con demencia o trastorno mental severo. Se recogió información sobre tipo de fractura (traumática o fragilidad), localización y características descriptivas de los pacientes.
ResultadosUn total de 491/616 (79,7%) de los pacientes con fractura en 2012 fueron contactados y 331 (349 fracturas) fueron incluidos. Las fracturas más comunes fueron antebrazo (82), costillas (38) y húmero (32); 225/349 (64,5%) fueron fracturas por fragilidad, con mayor proporción para las localizaciones típicas de la osteoporosis: fémur (91,7%), columna vertebral (87,7%) y fracturas principales (80,5%). La proporción fue mayor en mujeres, edad avanzada y pacientes con diagnóstico previo de osteoporosis.
ConclusionesMás de 4 de cada 5 fracturas principales registradas en SIDIAP son por fragilidad, con una mayor proporción para fémur (92%) y columna verterbal (88%), y menor proporción para otras localizaciones no típicas. Nuestros datos apoyan la validación de SIDIAP para el estudio epidemiológico de las fracturas osteoporóticas.
An increasing number of observational studies using electronic medical records (EMR) databases have recently been published, helping us to better understand the epidemiology of osteoporotic fractures, as well as to identify new (emerging) risk factors associated with an excess risk of fragility fractures. These studies have provided us with good-quality data on site-specific associations with obesity, type 2 diabetes mellitus, as well as the effects of a number of drugs.1–7
These EMR databases provide an elevated number of patients and relatively long follow-up, supporting large-scale epidemiologic studies at relatively low cost, compared to primary data collection cohorts.8 In addition, they allow for quick data extraction and analysis, minimizing the wait for recruitment and follow-up in classic cohort studies. The main limitation of epidemiologic EMR-based studies in the field of osteoporosis research, however, is that these data sources – in principle – do not distinguish between traumatic and fragility fractures given that no specific code/s exist that differentiate between them. This can lead to an overestimation of burden of disease by the inclusion of non-osteoporotic fractures, as well as to misclassification of the outcome (i.e., fragility fracture) in association studies. In an attempt to minimize such issues, authors usually focus on major fractures as their study outcome, as these are considered typically associated with low-trauma impact/s and/or fall/s.6,7 In addition, validation studies have generally shown a high concordance between the fracture site recorded in EMRs and the actual site as reported by patient/s or responsible clinicians,9 with no mention of whether the studied fractures were trauma-related or not. Given all this, we aimed to calculate the proportion of fragility fractures identified in a random sample of coded fractures in SIDIAP, both overall and after stratification by fracture site.
MethodsWe conducted a retrospective observational study in 6 primary care centres (La Sagrera, Casc Antic, Gòtic, Via Roma, Verneda Sud i Sant Martí Nord) contributing data to the Sistema d’Informació per al Desenvolupament de la Investigació en Atenció Primària (SIDIAP) database (www.sidiap.org). SIDIAP contains clinical primary care information, with diagnoses coded using the 10th edition of the International Classification of Diseases (ICD-10), clinical measurements, and immunizations, hospital admissions information, and pharmacy invoice data (detailed information on prescribed drugs dispensed in community pharmacies) for >5.5 million patients (80% of the population) in Catalonia, Spain.
We selected all patients ≥ 50 years old with a clinical fracture registered in 2012 primary care records (January 1 through December 31), using pre-specified (and previously validated) lists of ICD-10 codes (T02, T08, T10, T12, S02, S12, S22, S32, S42, S52, S62, S72, S82, S92 and subcategories).9
Patients with a record of dementia or a serious psychiatric disease in the EMR, as well as those with a fracture coded previous to the study period or subsequent data discarded fracture were excluded. Additionally, subjects who had no phone number, did not respond to 3 phone calls (at different times of the day), moved to a different primary care centre, or died during the study were also excluded. Recruitment and clinical interviews for data collection were undertaken from March 1 through December 31, 2013.
A sample size of 304 subjects randomly selected was estimated to be sufficient to estimate an expected positive predictive value of 65% with a 95% confidence and a precision of ±6 percent units, anticipating a 20% attrition rate.
This study was approved by the Clinical Research Ethics Committee of the Jordi Gol Primary Care Research Institute (P12/110), Barcelona, Spain. Verbal informed consent was obtained from all patients before inclusion. Information on patient characteristics, previous fractures, recorded diagnosis of osteoporosis, and previous use of anti-osteoporosis drugs was collected using an electronic data collection sheet.
All patients were asked about the date, site and type (traumatic or fragility) of fracture sustained during 2012. Fragility fracture is defined by the World Health Organization as “a fracture caused by injury that would be insufficient to fracture a normal bone…the result of reduced compressive and/or torsional strength of bone”; and may be clinically defined as a fracture “…that occurs as a result of a minimal trauma, such as a fall from a standing height or less, or no identifiable trauma”.10 Other fractures were considered as traumatic.
We used linear regression models to identify features associated with fragility (rather than traumatic) fracture/s. All the statistical tests were undertaken with a confidence interval (CI) of 95%, using the SPSS statistical package version 13 and R software version 3.2.3.
ResultsWe identified 616 patients with a registered fracture in 2012 and 491 were contacted. In 97 cases subsequent data discarded fracture (mostly teeth breaks coded as fracture of the face, and in a few cases ligament injuries coded as knee fracture). We included 331 patients in the final cohort (Fig. 1). Baseline and subgroup characteristics are described in detail in Table 1.
Baseline characteristics and description of patients subgroups with fragility vs traumatic fracture.
| Subjects included | All (n=331) | Fragility fractures (n=215) | Traumatic fractures (n=116) | P value |
|---|---|---|---|---|
| Age, mean±SD | 69.85±11.13 | 72.23±10.48 | 65.44±11.01 | <0.0001 |
| Sex, ♀; n (%) | 253 (76.4) | 183 (85.1) | 70 (60.3) | <0.0001 |
| BMI (kg/m2); mean±SD | 28.49±5.06 | 25.79±9.55 | 24.92±10.79 | 0.466 |
| Current smoker; n (%) | 42 (12.7) | 21 (9.8) | 21 (18.1) | 0.029 |
| Alcohol intake>3 units/day; n (%) | 10 (3.0) | 2 (0.9) | 8 (6.9) | 0.002 |
| Parental history of hip fracture; n (%) | 37 (11.2) | 34 (15.8) | 3 (2.6) | <0.0001 |
| Oral corticoids users; n (%) | 23 (6.9) | 19 (8.8) | 4 (3.4) | 0.066 |
| Total fractures; n | 349 | 226 | 123 | |
| Previous osteoporosis; n (%) | 86 (26.0) | 68 (31.6) | 18 (15.5) | 0.001 |
| Previous anti-osteoporosis treatment; n (%) | 42 (12.7) | 34 (15.8) | 8 (6.9) | 0.02 |
| Patients with previous fractures; n (%) | 67 (20.2) | 52 (24.2) | 15 (12.9) | 0.015 |
SD=standard desviation; BMI=body mass index.
The most common fractures were forearm (82), feet (49), ribs (38), and humerus (32); other locations were fibula (29), hand or fingers (28), hip (24), tibia (23), vertebral (16), and face or skull (15). In the clinical interview, 225/349 (64.5%) were classified as fragility fractures, with a higher 70.0% (180/257) when non-osteoporotic fracture sites (face, skull, and digits) were excluded. Validity was significantly better for classic osteoporotic fracture sites: 91.7% for hip, 87.7% for spine, and 80.5% when any major fracture (including hip, spine, wrist/forearm, and proximal humerus) was included.
Patients with fragility (non-traumatic) fractures were more often women, older, and had a higher prevalence of recorded osteoporosis compared to patients with traumatic fractures (Table 2).
Features associated with fragility (rather than traumatic) fracture/s.
| Variable | Odds ratio | 95% CI |
|---|---|---|
| Sex (female) | 3.76 | 2.22–6.42 |
| Age | ||
| 50–59 | REF | |
| 60–69 | 1.95 | 1.04–3.71 |
| 70–79 | 3.41 | 1.81–6.53 |
| 80 and older | 5.66 | 2.69–12.50 |
| Previous osteoporosis | 1.92 | 1.29–2.94 |
| Previous anti-osteoporosis treatment | 2.53 | 1.19–6.07 |
| Previous fractures | 2.15 | 1.17–4.13 |
We report the first validation of fragility fractures as identified in primary care centres contributing to an EMR database: >90% hip, >85% vertebral, and >80% major clinical fractures were classified as due to bone fragility rather than high-impact/trauma in 2012 cases identified in SIDIAP in patients ≥50 years old. This is reassuring for researchers using similar EMR datasets for the study of the epidemiology of major osteoporotic fractures. The proportion of fragility fractures was about 70% when all fractures (except face, skull, hand or fingers) were considered, which should be considered for the design, analysis and interpretation of future studies.
In addition, we identified patient characteristics associated with a higher likelihood of fragility fracture (amongst those with coded fractures), including the coded diagnosis of osteoporosis in EMR. Previous studies have shown, however, that about 25% to 30% of patients with a previous osteoporotic/fragility fracture or treated with anti-osteoporosis drug/s have no such diagnosis recorded in their records,11,12 limiting the usefulness of such a strategy for the identification of fragility fractures in these databases.
In validation studies of individual fracture cases, authors have explored the accuracy of fracture date/s and/or site/s using a number of data sources (linked classical cohort data, hospital databases, and free-text review of medical charts) as a reference/gold standard.13,9 Although these have shown EMR databases coding to be highly specific (>95% for all fracture sites tested) and moderately sensitive (almost 70% for hip fractures) for the identification of fracture sites, no previous validation of fragility fractures has been carried out, to our knowledge.
Two classical risk factors for osteoporotic fracture, female sex and age ≥60 years, were also predictors of fragility fracture.14 Other risk factors were more prevalent in the subgroup of patients with fragility fracture, including previous fracture, oral glucocorticoid use, or parental history of hip fracture.
Our study has both strengths and limitations. The main limitation is the representativeness of the SIDIAP database sample. The 6 participating primary care centres are located in urban areas; therefore, no data were included from rural centres. Nonetheless, the study's population base was considerable, with more than 54,000 registered patients in the age group of interest (50 years or older) and 90 GPs in the 6 participating primary care centres. In addition, >80% of the eligible patients were contacted and included, giving high external validity to our sample. Finally, a strength of our data is the individual validation of time, location, and type/nature of each fracture in a clinical interview with affected patients, which provided valuable information on the coding of fractures in the SIDIAP database, and generated recommendations for future research in the field. This EMR database is not used out of Catalonia, but published data from SIDIAP are potentially relevant to clinicians from the rest of the country (and probably from other countries as well).
This is the first individual validation of coded incident fractures in an EMR database, SIDIAP (from Catalonia). We showed that >80% of the major fractures (and >90% of hip fractures) registered for patients ≥50 years old are related to bone fragility rather than to trauma.
Conflict of interestDaniel Prieto-Alhambra's research group has received unrelated research grants from AMGEN, BIOIBERICA S.A., Laboratoires Servier and UCB Pharmaceuticals. The other authors have no conflict of interest.
This study received a research grant from the Primary Care Barcelona Ambit (Institut Català de la Salut), Ajuts XB 2012.