‘True neurogenic thoracic outlet syndrome’ (TN-TOS) is an extremely rare occurrence with a prevalence of 1/1,000,000, affecting young women aged 30-40 years. It is primarily characterized by irradiating neuralgic pain and loss of the motor function of the small muscles of the hand in the affected upper limb. The disease is caused by anatomical anomalies causing compression of the nerves passing through the thoracic outlet.1
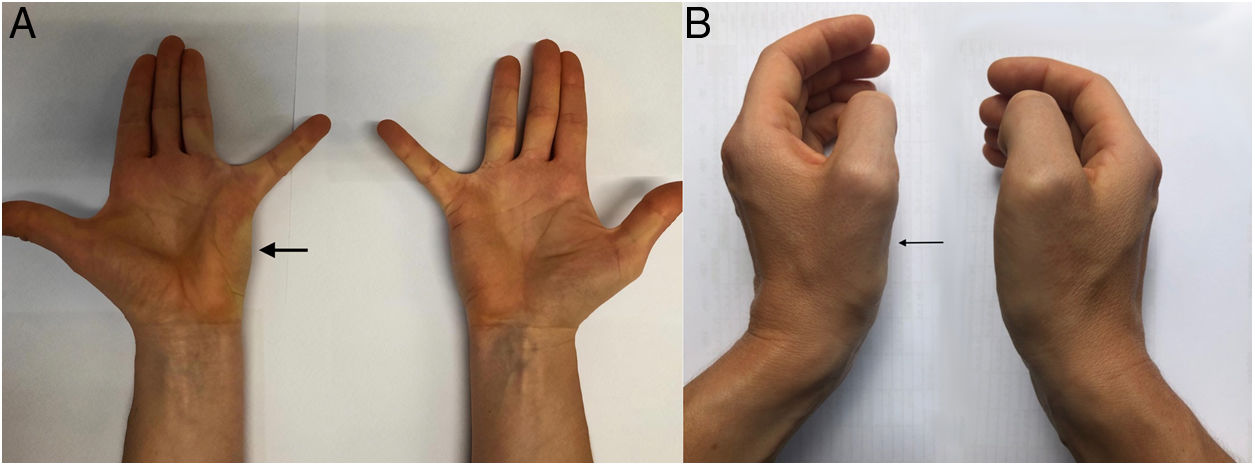
A 25-year-old female patient presented with irradiating pain in the left upper limb. Physical examination revealed a typical neuralgic pain, irradiating to the ulnar side of the upper limb, associated with hypoesthesia in the C8/T1 dermatome and eventually leading to atrophy in the abductor pollicis brevis, abductor digiti minimi and interosseus dorsalis muscles compatible with the typical Gilliat Sumner hand (Fig. 1)2 and suggesting loss of small motor function. There were no symptoms or signs of any vascular compression. Back then, 10 years ago the first examination was conducted by a neurologist who recommended conservative treatment after a negative electromyography (EMG) without requesting any imaging studies, thus missing the diagnosis.
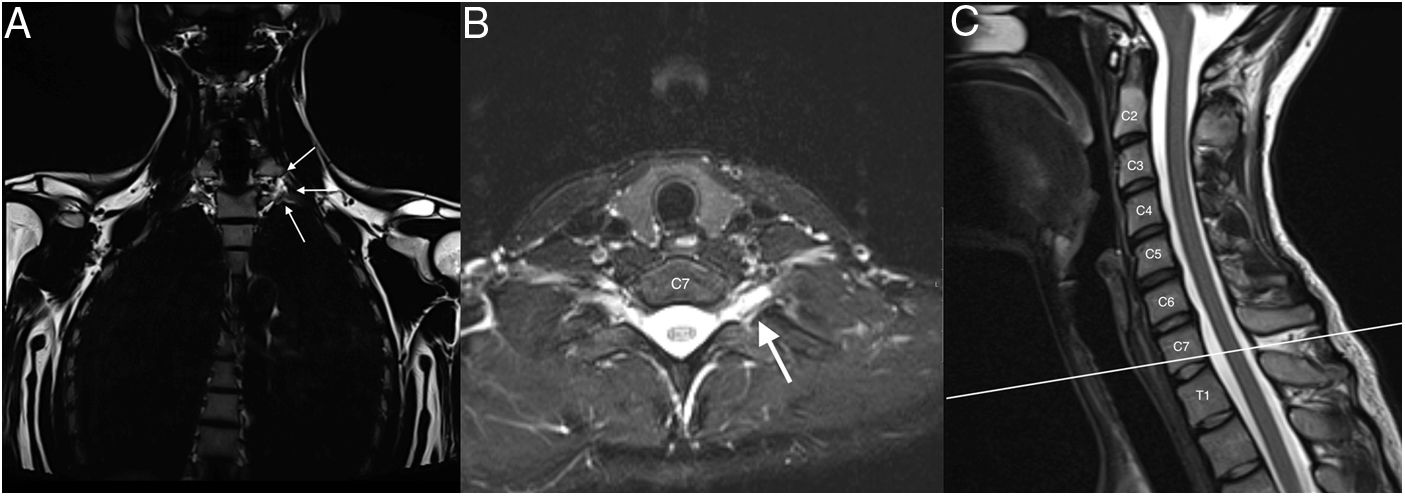
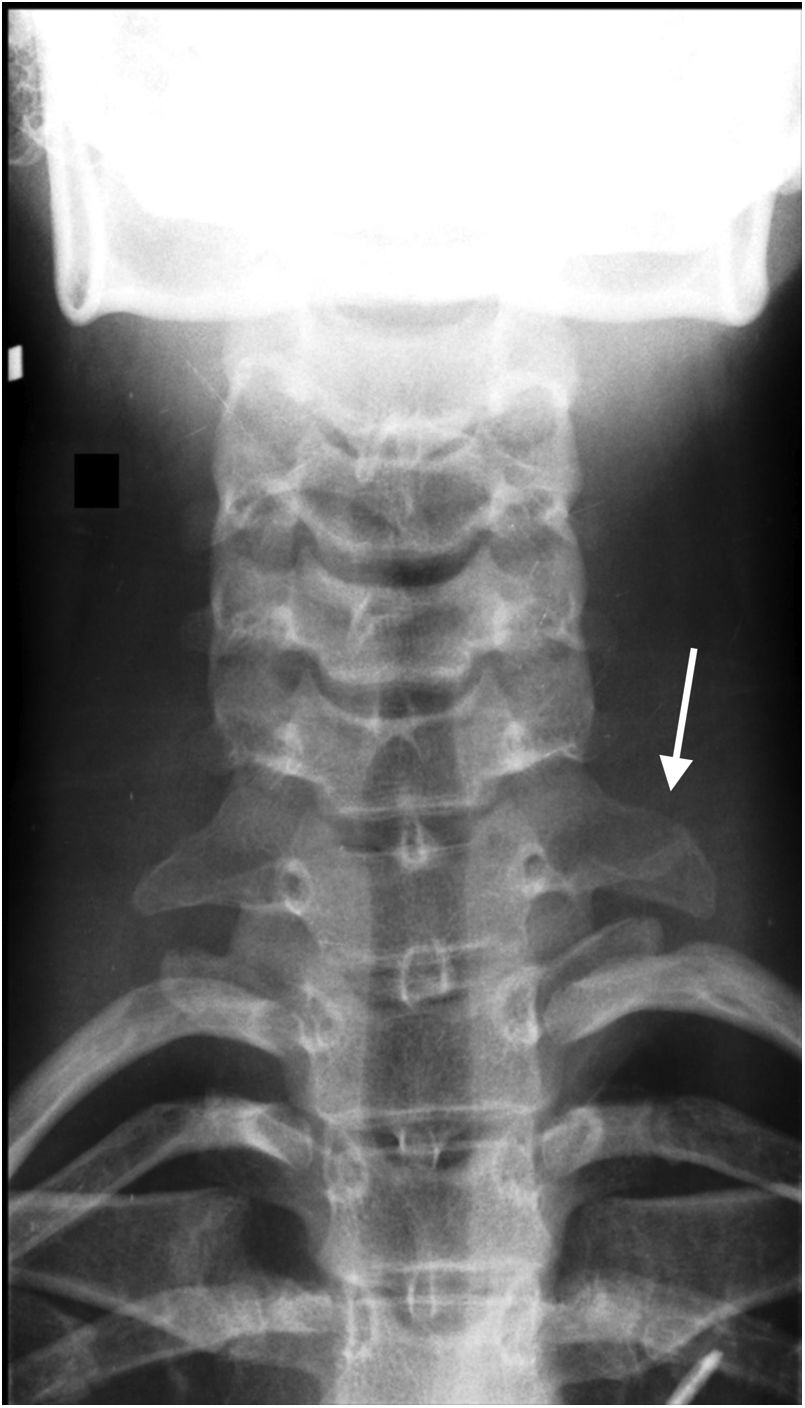
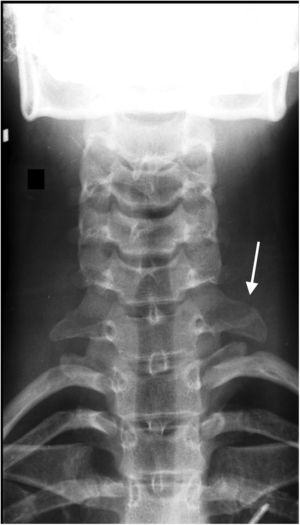
We conducted basic and needle-EMG examinations and found a severe inferior brachial plexopathy associated with severe chronic neurogenic impairment in the C8 and T1 innervated muscles. Further examination with magnetic resonance imaging (MRI) excluded any discoradicular conflict at the level of C8 and T1 but identified small excess of fat and edema in the form of a “teardrop” surrounding C8 and T1 suggesting compression of these nerves at the thoracic outlet level (Fig. 2). A standard radiography of the cervical spine clearly showed an abnormally elongated left C7 transverse process (Fig. 3). A diagnosis of TN-TOS was concluded.
Coronal (A), axial (B) and sagittal (C) MRI of the cervical spine. The coronal recordings are Dixon sequences where fat is emphasized (A), the axial and sagittal recordings are Dixon sequences where water is emphasized (B, C). (A) Notice more fat in the form of a “teardrop” (white on this image) around the left C8 under the transverse process (arrows), compared to right. (B, C) Hyperintensity around left nerve C8 (arrow), indicating more edema than on the right.
In patients with persistent complaints despite conservative treatment approaches, the ideal treatment of TN-TOS involves the timely removal of the structural deformity eventually having the potential to cause muscle atrophy. Identifying TN-TOS at its early stage is therefore imperative to prevent irreversible denervation of hand muscles. Wasting some functions of the hands in this era of radiology should no longer be the fate of patients as radiology offers a wide scale of imaging alternatives to make a timely diagnosis. We hope that this case will help improve the understanding of this disorder.
Authors’ contributionsAuthor Evelien Gryspeerdt has given substantial contributions to the conceptions and design of the manuscript. All authors have participated to drafting the manuscript. Author Koen Peers revised it critically.
All authors read and approved the final version of the manuscript.
CongressesThis paper was presented as poster at the (1) European Society of Physical and Rehabilitation medicine, Congress that was held online on 20th September 2020. (2) The Royal Belgian Society of Physical and Rehabilitation Medicine that was held online on 11th December 2020.
Conflicts of interestThe authors declare no conflict of interest.
The authors acknowledge Simon Van Cauwenberghe for writing assistance.