This paper emphasizes the anatomical substrate of several foot conditions that are seldom discussed in this context. These include the insertional and non-insertional Achilles tendinopathies, plantar fasciopathy, inferior and posterior heel spurs, foot compartment syndromes, intermetatarsal bursitis and Morton's neuroma. It is a rather superficial anatomical review of an organ that remains largely neglected by rheumatologists. It is our hope that the cases discussed and the cross examination by instructors and participants will stimulate study of the foot and the attention it deserves.
Este artículo enfatiza las estructuras anatómicas que sirven de sustrato a entidades clínicas como la tendinopatía no insercional e insercional del tendón de Aquiles, la fasciopatía plantar, los espolones calcáneos, los síndromes compartamentales del pie, las bursitis intermetatarsianas y el neuroma de Morton. Es un recorrido superficial por una zona que alberga abismos, ya que no podemos designar de otra manera el desconocimiento que muchos reumatólogos tenemos acerca del pie. Es nuestro deseo que este resumen y las demostraciones cruzadas de los elementos anatómicos accesibles sirvan para estimular el estudio profundo del pie por nuestros colegas.
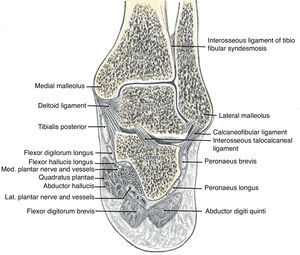
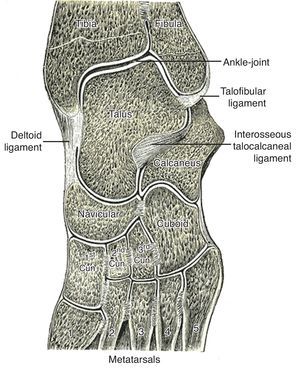
The leg bones, tibia and fibula, articulate with the top bone of the hindfoot, talus, at the talocrural joint (ankle) joint (Fig. 1). Talus, in turn, articulates with calcaneus below and navicular in front at the subtalar joint (talo-calcaneal-navicular joint) (Fig. 1). The talocrural joint is a hinge that dorsiflexes and plantarflexes the foot. The subtalar joint, however, has an axis that is oriented upward, anteriorly and medially entering the posterolateral angle of the calcaneus and piercing the superomedial aspect of the talar neck.1 Given this axis, flexion at the subtalar joint is associated with supination and adduction, while extension causes pronation and abduction. The talonavicular joint and the calcaneocuboid joint, although separate anatomically, are in the same transverse plane and jointly form the transverse tarsal joint (Fig. 2). The axis of this joint is longitudinal and follows the second metatarsal. Thus, motions at the midtarsal joint are rotatory motions along this axis. The long tendons plantar flex the talocrural joint if they run posterior to the malleoli and dorsiflex it if they run anterior. The same tendons, whether flexors or extensors of the talocrural joint, deviate the calcaneous in and supinate the forefoot, or deviate the calcaneous out and pronate the forefoot depending on their position in reference to the axis of the subtalar and midtarsal joints. As an example, in foot inversion, the tendons that stand out are those of posteriort tibialis (plantar flexor) and tibialis anterior (dorsiflexor). During gait, in the first half of the support phase, the axis passes through the center of the heel and follows the medial border of the 3rd metatarsal. In the second half, the heel is lifted and the axis is directed inward. At the end of the step the axis lies between the first and the second toes.2 There are, in addition, the intrinsic muscles that admirably adapt the foot to irregular surfaces that escape the control of the long muscles. In comparison with the hand, the foot is specialized to one function, which is to allow the body to stand, walk and run, while the hand lacks specialization and is therefore able to perform infinite tasks.
Patient 1. Non-insertional Achilles tendinopathy. “A 65 year-old man was seen with a severe posterior left heel pain that developed while walking. He had a history of asthma and had received monthly intramuscular depo-steroid injections for over a year. In addition, he had just completed a week of a fluoroquinolone antibiotic for the treatment of a urinary tract infection. On examination the left Achilles tendon was swollen and tender 4cm above the calcaneal insertion. Ten days later the tendon had a complete rupture while visiting a museum in Madrid. The rupture had to be repaired (Fig. 3)”.
Patient 2. Achilles entheseal organ inflammation. “A 35 year-old man was seen because of a bilateral posterior heel pain. He had had 3 episodes of acute anterior uveitis. On examination the back of both heels was swollen and tender to the level of the posterior superior calcaneal angle. When examined face down fluid could be fluctuated between the Achilles tendon and the calcaneus on both sides”.
Patient 3. Plantar fasciopathy. “Every morning when I gel up I have a severe pain under my right heel. I take a few steps and the pain goes away until the next morning, when I once again have the pain”.
Achilles tendon concentrates and then disperses the insertional fibers of 4 plantar flexor muscles that are essential for walking, running and jumping: lateral and medial gastrocnemiae, plantaris and soleus. The lateral and the medial heads of gastrocnemius arise from the back of the femur just above the lateral and medial femoral condyles, respectively. The knee joint capsule contributes fibers to both heads. The fabella is a sesamoid bone in the lateral head of gastrocnemius. Plantaris has its origin near the lateral head, runs an oblique course between gastrocnemius and soleus, and inserts in the medial aspect of calcaneus anterior to the Achilles tendon. Soleus, a leg muscle, has its origin in the fibula, an arch between the fibula and the tibia, and the tibia at the soleal line. In the middle of the calf gastrocnemius fuses with the Achilles tendon while soleus contributes muscle fibers to this tendon almost to its lower end. The course of the Achilles tendon is not straight but spiral, suffering a 90° rotation during its course.3,4 Due to this rotation the gastrocnemius tendinous fibers attach in the posterolateral, and the soleus tendinous fibers in the posteromedial, aspect of the calcaneus. Achilles tendon is the thickest and strongest tendon in the human body and is able to withstand a load of up to 12× the body weight while running. Achilles tendon lacks a synovial sheath. Instead, it has a paratenon which is a thin layer of fibrovascular tissue. Looking at the distal leg from the side, the Achilles tendon follows a course down and posterior while the bones and the remaining leg muscles go straight dow. This leaves a triangular space that is filled with fat, known as Kager's fat. The blood supply of Achilles tendon comes from 3 sources: the myotendinous union proximally, vessels derived from the periostium in the distal 2cm, and vessels from the paratenon and Kager's fat pad5 throughout its course. There is agreement in that the mid portion of the tendon is relatively hypovascular especially past middle age. This portion is prone to fatigue tendinopathy including rupture, damage from fluoroquinolone antibiotics, tophi deposition in gout patients, and nodules in rheumatoid arthritis.
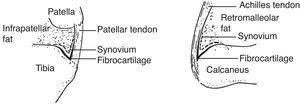
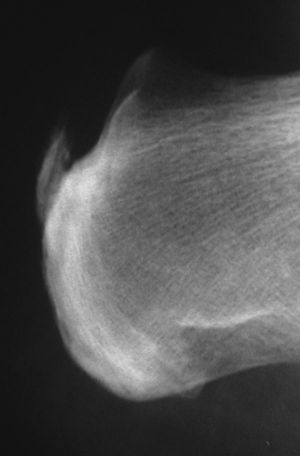
The Achilles entheseal organ6The anatomy of the Achilles entheseal organ is homologous to the patellar tendon entheseal organ.7 Instead of the tibia in the back is the calcaneus in the front. Instead of the patellar tendon in the front, is the Achilles tendon in the back, and instead of Hoffa's fat hanging apron on the top there is Kager's fat wedge on the top (Fig. 4). Both the deep infrapatellar bursa and the retrocalcaneal bursa have two fibrocartilaginous walls, one being tendon sesamoid cartilage and the other, periosteal fibrocartilague. In both the synovial lining is limited to the fat body. Also, both enthesis organs are affected with predilection in the spondyloarthritis in which bone erosions appear not at the actual site of tendon insertion, but in bone that underlies the periosteal fibrocartilague.8 In fresh cadavers without a history of rheumatic disease the retrocalcaneal bursa regularly contained a small amount of viscous synovial fluid which on all counts was similar to normal synovial fluid.9 Glycosaminoglycans were studied in this fluid and large amounts of hyaluronan were present explaining its high viscosity. This was in contrast to subcutaneous bursae such as the olecranon and the prepatellar. These sacs lacked free fluid and bursal washings revealed very little hyaluronan. In ultrasound and magnetic resonance studies was obtained with the foot in dorsal flexion and plantar flexion, and Kager's fat wedge was seen to exit and enter the bursa, respectively. Haglund's deformity is a posterior superior calcaneal prominence that may be asymptomatic or may cause pain and swelling by pressure on the retrocalcaneal bursa and the Achilles tendon.10
Calcaneal (Achilles) and patellar tendon entheseal organs. There is a striking homology between these structures. This includes a bursa that has a synovial-layered (interrupted line) wall that covers a hanging fat body, a cartilaginous anterior wall and a cartilaginous posterior wall (thick black line). Traces of a highly viscous fluid is normally contained in the calcaneal bursa.
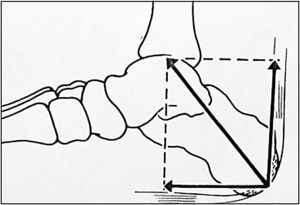
The relevant anatomy of Patients 1, 2 and 3 focuses on a functional unit, the Achilles-calcaneal-plantar (ACP) system and the plantar heel pad. The ACP system concept, which was developed by R. Arandes and A. Viladot in the 50ties, emphasizes the embryologic, anatomical and pathogenetic interrelationships between the Achilles tendon, the calcaneal tuberosity, the plantar fascia, and the plantar muscles abductor hallucis, flexor hallucis brevis and flexor digitorum brevis (Fig. 5).11 Unaware of this previous work, the hindfoot components of the ACP were recently studied based on the analysis of human fetuses of various ages and indeed there is a continuity between the Achilles tendon, the primordium of the calcaneal tuberosity and the plantar fascia. Unfortunately this study was not extended into the forefoot and the muscle connection explored in the earlier study was not assessed.12 The Achilles tendon appears to have 3 attachments. On the one hand, it is strongly attached to the calcaneal tuberosity. In addition, high quality sagittal MRI scans not only demonstrate continuity between the Achilles tendon and the plantar fascia but also, via myriad fibrovascular septae, between the distal Achilles tendon and the plantar fat pad.12 Thus, the Achilles tendon has three insertions: (a) osseous to the tuberosity of calcaneous, (b) fascial around the calcaneus and into the plantar fascia, and (c) into the skin via the plantar fat pad and its intricate system of fibrovascular septae. It should be mentioned that the calcaneal insertion of the Achilles tendon is not at a single point, as it could be inferred from sagittal imaging studies, but as a crescent-shaped, partially encircling structure that attaches to the calcaneal tuberosity posteriorly and on the sides.13 Finally, the tridimentional anatomy of the calcaneal plantar fat pad has been recently elucidated based on the reconstruction of coronal and axial CT sections. The pad is thick under the heel and has flanges on the sides and in back of the calcaneus where it covers the Achilles tendon insertion. In addition, it has a constant crest that corresponds to the lateral plantar septum that separates the lateral and central compartments of the foot.14 This crest appears to both anchor the pad and provide entrance into the pad to the neurovascular structures that traverse the septum. Current view among many professionals (among them rheumatologists) is that a plantar hindfoot pain indicates plantar “fasciitis” (a more correct term would be plantar fasciopathy). However, a cursory review of the anatomy of the subcalcaneal fat pad and the soft tissues that underlie the plantar fascia should make us pause and raise questions rather that hold on to a tenuous diagnosis. Hidden under the plantar fascia there are several foot compartments, 3 layers of short muscles, long tendons that enter the plantar aspect of the foot such as tibialis posterior, peroneus longus, flexor hallucis longus and flexor digitorum, a tendon intersection between flexor hallucis longus and flexor digitorum, the regional nerves, plus ligaments such as the plantar calcaneonavicular (spring) ligament and the long plantar. Progress in the elucidation of plantar pain can only be made after these and other structures are recognized and their individual and collective functions are understood.
The plantar fasciaThe undistinguished appearance of the posterior insertion of the plantar fascia says nothing about the exquisite complexity of its anterior insertions.15 As mentioned, the plantar fascia inserts in the inferomedial calcaneal tuberosity, adds superficial fibers from the Achilles tendon that contour the calcaneus, and anchors the fibrovascular trabecular skeleton of the retro- and subcalcaneal fat pad. In the forefoot, however, the plantar fascia resolves in a complex and highly directional system that includes a firm anchor to the fibrous flexor sheaths of the toes, vertical strands to the skin and sagittal septae that contain submetatarsal fat cushions as well as fat cushions around the digital nerves. This complexity is necessary to steady the fat pad under the metatarsophalangeal (MTP) joints and around the digital nerves while standing and during the late stance phase of gait as dorsiflexion of the MTP occur. This anchoring function can be shown with a simple experiment15: in the relaxed state the skin under the MTP joints is soft and can be freely displaced in all directions. With the toes in dorsiflexion, however, the skin cannot be displaced. The plantar fascia helps maintain the longitudinal arch of the foot and surgical fasciotomy, that was used in the past to treat unremitting plantar fasciopathy, causes a significant flattening of the foot. Finally, the plantar fascia has elasticity and accumulates energy during gait. This phenomenon is probably enhanced by the “windlass effect”, which is an increase in the concavity of the foot that occurs with toe dorsiflexion.
Calcaneal spursThere are two types of calcaneal spurs, the posterior and the inferior or subcalcaneal spurs (Fig. 6). Structurally and pathogenetically they appear to be quite different. Posterior spurs occupy the most superficial portion of the Achilles tendon near its insertion in the calcaneal tuberosity. Thus, they are intratendinous, their pattern of ossification is a composite of various types of ossification-endocondral, intramembranous and chondroidal- and their development appear to be a response to longitudinal traction.16 Plantar spurs, on the other hand, do not grow into the plantar fascia but their location is immediately deep to it. In their formation there is a cartilaginous front that is being replaced by bone. The stimulus for their formation appears to be vertical stresses placed on the calcaneus.17
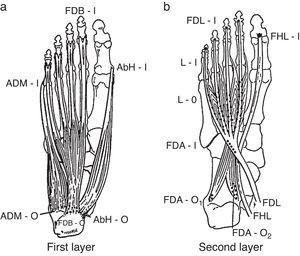
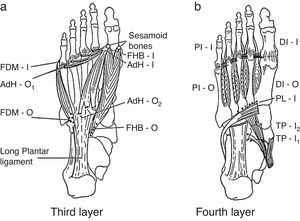
Foot compartmentsDeep to the plantar fascia there are 4 foot compartments, the lateral, the central, the medial and the interosseus.18,19 The medial plantar septum separates the medial and the central compartments. Two muscles occupy the medial compartment, abductor hallucis and flexor hallucis brevis, plus the tendon of flexor hallucis longus. The central compartment comprises three muscle levels or layers (Figs. 7a and b, 8a and b). Most superficially lies flexor digitorum brevis which originates in the medial calcaneal tuberosity deep to the plantar fascia and inserts in the middle phalanges of digits 2–5. The next level contains quadratus plantae that arises in the calcaneus and attaches to the tendon of flexor digitorum longus, and the lumbrical muscles that have their origins in the tendons of flexor digitorum longus and insert in the dorsal aponeurosis of the toes 2–5. The deepest level contains adductor hallucis brevis. The lateral plantar septum separates the lateral and the central compartments. As mentioned, this septum carries important neurovascular bundles that enter the subcalcaneal fat pad via its crest. The lateral compartment contains abductor digiti minimi, flexor digiti minimi and opponens digiti minimi. There is also a deep plantar fascia that covers the interosseous muscles and separates them from the aforementioned compartments.
From the plantar surface down, the 1st and the 2nd muscle layers of the foot muscles are shown. 1st layer: ADM, abductor digiti minimi; AbH, abductor hallucis; FDB, flexor digitorum brevis; O, origin; I, insertion. 2nd layer: FDA, flexor digitorum accesorius; FHL, flexor hallucis longus; FDL, flexor digitorum longus; L, lumbricals; O, origin; I, insertion.
Additional foot muscle layers include: 3rd layer: FDM, flexor digiti minimi brevis; AdH, adductor hallucis; FHB, flexor hallucis brevis. 4th layer: PI, plantar interossei; DI, dorsal interossei; PL, peroneus longus; TP, tibialis posterior; O, origin; I, insertion.
In the medial retromalleolar region, the most superficial tendon is tibialis posterior. Tibialis posterior has its origin in the fibula, the tibia and the inseroseus membrane. As the ankle is approached the tendon of tibialis posterior runs along the medial border of the tibia where it is seen to tent the skin when the foot is held in inversion. The tendon contours superficially the medial malleolus and proceeds anteriorly to a broad insertion in the tubercle of the navicular, the first-third cuneiforms and the base of the metacarpals second-fourth. Deep (lateral) to tibialis posterior in back of the medial malleolus runs flexor digitorum longus. This tendon inserts at the base of the distal phalanges of the second-fifth toes. And deep or lateral to flexor digitorum longus runs flexor hallucis longus which in its way to the base of the distal phalanx of the big toe has to relocate medial to the former tendon and does so at an intersection known as “knot of Henry” in which flexor hallucis longus runs deep to flexor digitorum longus. An intersection syndrome may occur at this site which is deep to the medial malleolus or the navicular process. Pain at this site is increased by active motions of the big toe.20 The true frequency of the condition among the many causes of plantar pain is unknown.
Lumbricals, ventral and dorsal interossei21Their disposition is similar to the one they have in the hand. However, the axis of the forefoot is the second ray (metatarsal and phalanges). Seen from the plantar side, the lumbricals are superficial to the deep transverse intermetatarsal arch which is the ligamentous structure that binds the sides of the plantar plates of adjacent toes. There are 4 lumbricals and their insertion is to the extensor lamina of toes second-fifth. On the other side of the deep transverse metatarsal ligament lie the 3 plantar and the 4 dorsal interossei. Each of the 3 lateral toes have a plantar interosseus that approximate them to the second toe. Regarding the dorsal interossei, that separate the toes, the second toe has 2 (same as the middle finger in the hand), and the third and fourth toes have 1.
Patient 4. Morton's neuroma “A 37 year-old woman is seen with right forefoot pain. The pain has a shooting quality and between paroxysms there is a burning, tingly sensation in the third web space. Pain is triggered by wearing high heel shoes and goes away if she wears sandals.”
Patient 5. Intermetatarsal bursitis “A 32 year old woman with a poorly treated rheumatoid arthritis is seen with right forefoot pain and her perception that the third and fourth toes are increasingly separated. High heel shoes exacerbate her pain.”
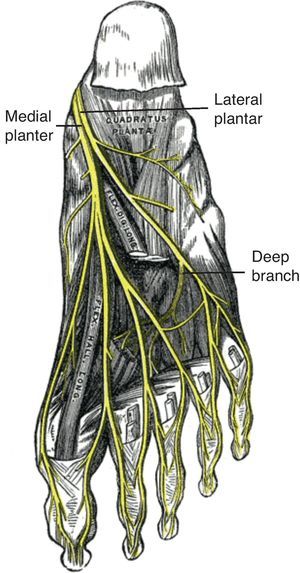
These structures are considered together to facilitate the recognition of Morton's neuroma and intermetatarsal bursitis. In our experience these entities are often confused with each other due to deficient anatomical knowledge. The first structure to be considered is the tibial nerve and its branches, the medial and lateral plantar nerves (Fig. 9). These nerves supply all of the muscles in the plantar side of the foot as well as the plantar skin in such a manner that the lateral plantar nerve is homologous to the ulnar nerve and the medial plantar nerve is homologous to the median nerve. The superficial branches of the plantar nerves may be proper or common. A proper nerve supplies the skin of the fibular or the radial sides of a toe. The medial plantar nerve branches into one proper nerve to the medial side of the great toe, and 3 common plantar nerves which in turn innervate kissing surfaces of the first-fourth toes. The lateral plantar nerve has a proper branch to the fibular half of the fifth toe and common nerve that divides into 2 proper nerves for the medial side of the fifth toe and the lateral side of the fourth toe. This pattern of innervation is identical to the share of the ring digit between the median and the ulnar nerves. Morton's neuroma refers to a degenerative neuropathy in which a plantar proper digital nerve is surrounded by fibrosis. The condition is a result of microtrauma and occurs predominantly in women who wear high heels. Morton's neuroma is superficial to the deep intermetatarsal ligament, is bound on both sides by the fibrous flexor tendon sheaths, and is superficially covered by plantar fat (Fig. 10).22,23 On the other side of the transverse metatarsal ligament lie the intermetatarsal bursae which occupy the space between the metatarsal heads and extend distally about 1cm.24,25 Intermetatarsal bursitis is common in rheumatoid arthritis patients. Since the intermetatarsal bursa is wedged between 2 metatarsal heads, when the bursa is swollen it separates 2 toes. In contrast, in proliferative synovitis of one metatarsophalangeal joint 3 toes is separated: a neighbor toe is pushed to one side, the other neighbor toe is pushed to the other side and the affected toe remains in the middle.
Patient 6. Subtalar joint rheumatoid synovitis “A 28-year old woman with rheumatoid artritis is seen with persistent pain and swelling in the left ankle. Flexion and extension movements of the talocrural joint are painless. Inversion and eversion movements of the heel cause severe pain. Her medications were optimized and she was given a steroid infiltration in the left subtalar joint.”
Aspiration of the foot joints is difficult because of the weird orientation of the articulating surfaces. While aspiration of the talocrural joint has an AP direction, at the subtalar joint is a lateromedial, horizontal and slightly posterior affair. In the remaining joints blind aspiration or injection is always difficult but it becomes less difficult if the anatomy is recognized by palpation. Ultrasonography, when available, facilitates or makes possible all of these procedures. The same goes for aspiration or injection of the retrocalcaneal bursa.25
Conflict of interestThe authors have no conflict of interest to declare.
Arches
Examination of joints
Talocrural (ankle)
Subtalar (talo-calcaneal-navicular joint)
Midtarsal joint (talonavicular joint plus calcaneocuboid joint)
Metatarsophalangeal
Intermetatarsal spaces
Interphalangeal
Anterior aspect
- •
Neck of talus in plantar flexion
- •
Anterior tibialis tendon
- •
Extensor pollicis longus tendon
- •
Extensor digitorum longus
- •
Extensor digitorum brevis
- •
Pedal artery
Medial aspect
- •
Medial malleolus
- •
Posterior tibialis tendon
- •
Flexor digitorum longus
- •
Flexor hallucis longus tendon
- •
Sustentaculum talis
- •
Spring ligament
- •
Tubercle of scaphoid
- •
Posterior tibial artery
Lateral aspect
- •
Peroneal tubercle
- •
Proximal head of the fifth metatarsal
- •
Peroneus tertius
- •
Peroneus brevis
- •
Peroneus longus
Posterior aspect
- •
Calcaneal tuberosity
- •
Posterior superior angle of calcaneus
- •
Gastrocnemia
- •
Soleus
- •
Plantaris
- •
Non insertional and insertional Achilles tendon
- •
Kager's fat
- •
Retrocalcaneal bursa
- •
Retroachilles bursa
Plantar aspect
- •
Plantar fat pad
- •
Plantar tuberosity
- •
Plantar fascia
- •
Windlass effect of toe dorsiflexion
- •
Site of tendon intersection (flexor hallucis longus/flexor digitorum longus)
- •
Metatarsal heads
- •
Site of the intermetatarsal bursae
- •
Course of medial and lateral plantar nerves
- •
Site of Morton's neuroma