Pseudoxanthoma elasticum (PXE) is a rare hereditary disorder that affects connective tissue and consists of a progressive calcification of the elastic fibers of the skin, the Bruch membrane in the retina and cardiovascular system. Its prevalence in the general population is estimated to be 1:25,000–100,000 population, with a slight predominance of women.1 It frequently presents as yellowish papular lesions, which can converge and form plaques with an irregular morphology and a “paved” aspect due to the fact that the skin becomes laxer and more redundant.
The association of this disorder with other systemic connective tissue diseases is rare. To date, there have been 6 cases associated with rheumatoid arthritis,2–5 2 with systemic lupus erythematosus (SLE)6 and another associated with ankylosing spondylitis.7 We describe a case of PXE in a patient with SLE.
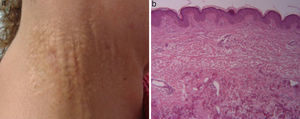
The patient was a 46-year-old woman, an active smoker, who had been diagnosed with SLE at the age of 28 years. She began with a nephrotic syndrome secondary to World Health Organization class IV diffuse proliferative lupus nephritis, which was treated with mycophenolate mofetil. This achieved resolution of the nephrotic syndrome, and she had been asymptomatic since then. During a check-up, she mentioned the development of asymptomatic skin lesions on her neck and in axillae. Physical examination revealed papular lesions measuring around 3cm×7cm, distributed on both sides of her neck. They were yellowish and lax, like “goosebumps” (Fig. 1), and she had others that were similar but smaller in the axillae. A specimen was taken for a skin biopsy which showed the existence of a high number of fragmented elastic fibers in the dermis (Fig. 1), a finding compatible with PXE. The study was completed with an examination of the fundus which showed nothing abnormal and renal ultrasound which revealed no signs of disease.
Pseudoxanthoma elasticum is a hereditary connective tissue disease related to a mutation in the ABCC6 gene located on chromosome 16p13.1, that encodes the multidrug resistance protein 6 (MRP6), which is one of the family of adenosine triphosphate-dependent membrane transport proteins, which are mostly expressed in the liver and kidneys. Two types of inheritance have been described: autosomal recessive in 90% of the cases and autosomal dominant, much rarer. Mutation in the ABCC6 gene provokes an absence of MRP6, which leads to an accumulation of substances with a high affinity for elastic tissues, resulting in the distortion of calcium deposits and fragmentation of elastic fibers.
Cutaneous manifestations include asymptomatic yellowish papules distributed symmetrically from the start of the neck that can extend to the flexure area. Although not pathognomonic, a characteristic ocular finding is the presence of angioid streaks that represent calcium deposits on the Bruch membrane. They can cause rupture of blood vessels, leading to neovascularization and retinal hemorrhage, resulting in a loss of visual acuity. In the cardiovascular system, calcification of the walls of small and medium-sized arteries can produce premature atheromatosis. The diagnosis of PXE is based on clinical suspicion and should be confirmed by a histological study, which reveals fragmentation and distortion of elastic fibers in the reticular dermis and the accumulation of calcium carbonate and phosphates in the extracellular matrix.
The pathophysiological mechanism that demonstrates the possible association between PXE and other inflammatory connective tissue diseases has not yet been established; however, the first case of association was described decades ago and, since then, there have been reports of 9 more cases. Nevertheless, when they are analyzed, no special feature has been identified that would enable us to reach conclusions. Still, given that PXE can be accompanied by potentially serious ocular and vascular manifestations, it is important that clinicians be aware of this possible association.
Please cite this article as: Muñoz Gómez MM, Novella Navarro M, Ramírez Gómez M, Navas-Parejo A. Presentación de un caso de Pseudoxantoma elasticum y lupus eritematoso sistémico: ¿una asociación infrecuente? Reumatol Clin. 2017;13:183–184.