The recent FRIDEX calibration proposed cost-effectiveness thresholds for the Spanish population. The aim of our study is to evaluate the impact of its application in routine clinical practice and to compare its thresholds with those of the National Osteoporosis Guideline Group (NOGG).
Material and methodsCross-sectional study in women referred to a bone densitometry unit who were not receiving antiresorptive therapy. The absolute risk of major fracture or hip fracture was calculated with the Spanish and British formulas of the FRAX® tool using the intervention thresholds of the FRIDEX calibration and the NOGG guideline, respectively.
ResultsThe study included 607 women with a median age of 59.4 (IQR=14) years. Treatment was initiated in 31.4% after bone mineral densitometry. With the application of the FRIDEX calibration, bone mineral density testing would have been indicated in 35.4% of the sample and treatment in 26.7%, reducing costs by 18.8% over a 5-year period. The NOGG guideline would have recommended testing in 32% and treatment in 21.3% of the participants, resulting in a reduction in costs of 35% over 5 years, when compared with the standard approach. Agreement between the FRIDEX calibration and the NOGG guideline, as defined by Cohen's kappa coefficient, was low in terms of both diagnostic (0.16 [95% CI, 0.09–0.24]) and therapeutic indications (0.39 [95% CI, 0.31–0.47]).
ConclusionsThe application of the FRIDEX calibration and the NOGG guideline improves efficiency in the management of osteoporosis, although the level of agreement between the two is low.
En España, el estudio FRIDEX ha aportado recientemente unos umbrales de riesgo coste-efectivos para el manejo de la osteoporosis. El objetivo del estudio es evaluar el impacto de su aplicación en la práctica clínica habitual, comparándola también con los umbrales de la National Osteoporosis Guidelines Group (NOGG).
Material y métodosEstudio transversal realizado en mujeres remitidas a una unidad de densitometría ósea. El riesgo absoluto de presentar una fractura mayor o de cadera se calculó mediante la fórmula FRAX® española y británica para poder emplear los umbrales de intervención de la calibración FRIDEX y de la guía NOGG, respectivamente. Se descartaron mujeres con tratamiento antirresortivo.
ResultadosFueron incluidas 607 mujeres con una mediana de edad de 59,4 (RIQ=14) años. El 31,4% recibieron tratamiento después de la densitometría ósea. El empleo de la calibración FRIDEX indicaría una densitometría ósea al 35,4% y tratamiento al 26,7%, lo que supondría una reducción de gastos a los 5años del 18,8%. Según la guía NOGG precisarían densitometría ósea el 32% y tratamiento el 21,3%, siendo el ahorro de un 35% a los 5años respeto a la actitud habitual. La concordancia de la guía NOGG y del FRIDEX según el coeficiente kappa de Cohen fue baja tanto a nivel diagnóstico (0,16 [IC 95%: 0,09-0,24]) como terapéutico (0,39 [IC 95%: 0,31-0,47]).
ConclusionesLa aplicación de la calibración FRIDEX y de la guía NOGG aumentaría la eficiencia del manejo de la osteoporosis, aunque su concordancia es baja, indicando tratamiento en diferentes perfiles de mujeres.
Around 200 million individuals worldwide have been diagnosed with osteoporosis and, each year, there are 1.7 million osteoporotic fractures involving the hip.1 In Spain it has been estimated that over the next 10years there will be 714,000 osteoporotic fractures, most of them in women over 70years of age.2 However, many cases of osteoporosis are not diagnosed and, frequently, no treatment is prescribed even after the patient has had a fracture.3,4 The impact on public health is enormous because of the high morbidity and mortality rates and the effect of these fractures on quality of life, in addition to their being accountable for increasing health costs.5
At the present time, attention is focused on identifying individuals with a high osteoporotic fracture risk, more than on detecting those with osteoporosis diagnosed exclusively by measuring bone mineral density (BMD).6 This identification is carried out with the help of tools—like the FRAX® score—which, integrating the information from different risk factors, enables the calculation of the absolute risk of fracture in coming years as the most accurate way to decide the need for ancillary diagnostic tests or of initiating a specific therapy. The intervention thresholds are established depending on local factors, such as reimbursement policies, health economic evaluation, willingness to pay for osteoporosis care and access to dual-energy X-ray absorptiometry (DXA).4,7
The recommendations issued by the National Osteoporosis Guideline Group (NOGG) of the United Kingdom, one of the guidelines with the greatest international influence, are based on this model of intervention and are supported by the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF), although many European countries have their own policies.8 In Spain, at this moment, there is no consensus on the thresholds for intervention; however, researchers working with the Risk Factors and Densitometry by Dual-energy X-ray Absorptiometry (FRIDEX) cohort, recently proposed a cost-effective calibration of the FRAX®.9
The objective of our study is to evaluate the impact of the application of the FRIDEX calibration in routine clinical practice and determine whether it translates into a reduction in the number of densitometries and treatments prescribed and, thus, increasing the efficiency of the associated costs. Moreover, it is compared with the NOGG guideline thresholds to detect possible differences.
Material and MethodsStudy DesignWe designed a cross-sectional study to be carried out in a sample of women referred from different health care settings (primary and specialized care) of the health area of León, in northwestern Spain, to undergo axial DXA in the morning shift of the University Health Care Complex of León between May 2014 and December 2014.
Inclusion and Exclusion CriteriaWomen between 40 and 90years of age with no previous treatment for osteoporosis (bisphosphonates, calcitonin, hormone replacement therapy, strontium ranelate, denosumab, teriparatide, raloxifene or bazedoxifene) were consecutively enrolled. We excluded patients who were referred to undergo DXA during follow-up after bariatric surgery and those diagnosed with a metabolic bone disease other than osteoporosis (for example, osteomalacia or Paget's disease), myeloma or any cancer involving bone.
Study ProcessAncillary staff of the radiology department, properly trained, gathered the necessary clinical information by means of a structured questionnaire. In addition, the same members of the team performed the pertinent measurements for the physical examination. In every case, the patient's history was reviewed to reduce possible information biases. One month after the test, the women who met the criteria for inclusion were telephoned regarding the post-DXA approach of their attending physicians.
The risk factors considered were those included in the FRAX® tool.10
Bone mass measurements were made by the same qualified technical staff using the same densitometer. The technique employed for the measuring the bone mass was DXA. For this purpose, we used a Lunar Prodigy Primo densitometer equipped with an EnCORE Windows-driven software platform (GE Healthcare, Wilmington, MA, United States).
Evaluation of Fracture RiskTo calculate the 10-year probability of a hip fracture and of a major fracture we utilized the FRAX® application for the Spanish and the United Kingdom populations which is freely available on the Internet: http://www.shef.ac.uk/FRAX/.
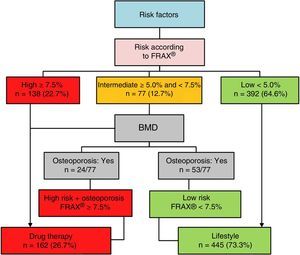
FRIDEX CalibrationThe FRIDEX cohort is a dynamic cohort of Spanish women aged 40 to 90years who were selected by their attending physicians to undergo DXA and were followed for a period of 10years.11 A model of the FRAX® tool calibrated for the Spanish population based on the FRIDEX cohort was recently reported. It enables the identification of groups of women with a low and high risk of fragility fracture over a 10-year period and involves a cost-effective assessment.9 The flow chart based on this model can be observed in Fig. 1.
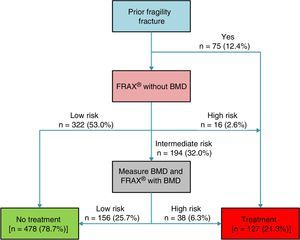
National Osteoporosis Guideline GroupThe British guidelines, referred to as NOGG, propose the FRAX® tool for population screening and establish 3 categories depending on the absolute risk of fracture over a 10-year period: high risk, intermediate risk and low risk.12 Based on these results and an analysis of cost-effectiveness, NOGG proposes an algorithm for diagnostic decisions and certain thresholds for the initiation of drug therapy that vary according to patient age (Fig. 2).
Cost ComparisonFor the comparative analysis of the costs we utilized the NOGG guidelines and the FRIDEX calibration. The cost estimated for DXA was the rate applied by the public health service of the Spanish autonomous community of Castile and León (Sacyl) for agreements with third parties, amounting to €58.6 (Official Gazette of Castile and León 31/1/2011, available at: http://bocyl.jcyl.es/boletin.do?fechaBoletin=31/01/2011). To calculate the mean cost of 1 year of treatment, we used data from the publication of the Instituto de Salud CarlosIII, Madrid, based on the medications most frequently administered in the treatment of osteoporosis in Spain during 2010, with the exception of calcium and vitamin D supplements.13 The mean cost, according to the profile for the consumption of medications for osteoporosis in Spain, was €427/year in 2010. The cost of 5years of treatment was estimated (€2135) for all of the models (approach adopted, NOGG and FRIDEX calibration).
Statistical AnalysisBased on previous studies, we calculated a sample size of 607 patients to be able to detect 25% of preventable BMD with a 95% confidence interval and an error of 3%.14 All of the collected variables (categorical and continuous) were loaded onto a database (Microsoft Access) and then analyzed using a statistical software package (SPSS version 15.0, SPSS Inc., Chicago, IL, United States). The normal distribution of the continuous data was confirmed with the Kolmogorov–Smirnov test; if the distribution was normal, they are presented as the mean (standard deviation [SD]) and if it was not normal, as the median (interquartile range [IQR]). The categorical data are expressed as percentages. For the analysis of the data, we used the chi-square test for the comparison of proportions and categorical variables, the Wilcoxon signed-rank test for continuous variables in which the data was not normally distributed and Student's t test for unpaired or paired data for variables with a normal distribution. The confidence intervals were calculated by means of a bootstrapping technique. Cohen's kappa coefficient was utilized to evaluate agreement in each system for diagnostic and drug intervention, and the level of agreement was considered high when the kappa statistic was >0.8 and good when it was >0.6. A P value <.05 was considered to indicate statistical significance. This report is adapted to the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) initiative.15
Ethical AspectsThe nature of the study was explained in detail to each patient and they provided their verbal informed consent. The study protocol was approved by the research committee of our center.
ResultsThe study population included 607 women with a median age of 59.4 (IQR=14) years; the average body mass index (BMI) was 26.3 (SD=4.5)kg/m2. According to the densitometry performed, they had a T-score of −1.4 in spine (SD=1.3), −1.4 in femoral neck (SD=1.3) and −2.2 in total hip (SD=1.2). The prevalences of the risk factors that are included in the FRAX® tool were, in descending order: secondary osteoporosis (24.1%), tobacco use (16.5%), parental hip fracture (15.2%), prior clinical fracture (12.4%), corticosteroid therapy (8.4%), rheumatoid arthritis (7.6%) and alcohol consumption (2.1%). In all, 31.4% of the women in the sample were prescribed medication by their attending physician after densitometry, whereas 36% of those who had a history of a fragility fracture were not being treated.
Application of the FRIDEX CalibrationAccording to this calibration (Fig. 1), the women in the study were classified as follows: 392 (64.6%) as low risk, 77 (12.7%) as intermediate risk and 138 (22.7%) as high risk. The FRIDEX calibration proposes that bone densitometry be performed in those patients with high and intermediate risk, that is, 35.4% of the women in this study sample. Of the women analyzed, 26.7% required treatment.
Application of the NOGG GuidelinesThe utilization of the NOGG guidelines allocated the women into 3 risk groups (Fig. 2): 322 (53.0%) as low risk, 194 (32.0%) as intermediate risk and 91 (15.0%) as high risk. Only the group at intermediate risk (32.0%) required DXA. In accordance with the therapeutic intervention thresholds, drug therapy would be indicated in 21.3% of the participants.
Comparison Including the Approach Adopted, the FRIDEX Calibration and the NOGG GuidelinesThe percentage of DXA requested on the basis of the NOGG guidelines and of the FRIDEX calibration was not statistically significant (P=.059). However, according to Cohen's kappa coefficient, the level of agreement was low (0.16; 95% CI: 0.09–0.24). With respect to therapy, according to the FRIDEX calibration, it would be indicated in 26.7% of the women, a lower proportion than the number actually treated (31.3%, P<.001), but higher than that of the NOGG guidelines (21.3%, P<.001). The level of agreement between the FRIDEX calibration and the therapeutic approach adopted was 0.29 (95% CI: 0.31–0.47). The characteristics of the women in which the results differed can be seen in Table 1.
Characteristics of the Women in Whom the Results Based on the NOGG Guidelines and on the FRIDEX Calibration Differed With Regard to Recommending DXA and Indicating Antiresorptive Therapy.
| Indication for DXA | Indication for treatment | |||||
|---|---|---|---|---|---|---|
| NOGG yes, FRIDEX no | NOGG no, FRIDEX yes | P | NOGG yes, FRIDEX no | NOGG no, FRIDEX yes | P | |
| Patients (n) | 103 | 124 | 50 | 87 | — | |
| Age (years) | 53.9 (5.6) | 70.8 (9.1) | <.001 | 53.7 (5.1) | 74.4 (6.6) | <.001 |
| Weight (kg) | 64.7 (11.7) | 64.2 (10.8) | NS | 62.2 (10.3) | 65.2 (10.3) | <.05 |
| Height (cm) | 159.7 (7.0) | 154.8 (8.1) | <.001 | 158.5 (8.0) | 153.4 (6.6) | <.001 |
| BMI (kg/m2) | 25.4 (4.7) | 26.9 (4.3) | <.002 | 24.8 (3.9) | 27.7 (3.7) | <.001 |
| Tobacco use | 24 (23.3%) | 10 (8.1%) | .004 | 19 (33.9%) | 3 (3.3%) | <.001 |
| Alcohol consumption | 5 (4.9%) | 0 (0%) | NS | 2 (4.0%) | 1 (1.2%) | <.05 |
| Corticosteroids | 13 (12.6%) | 10 (8.1%) | <.001 | 6 (12.0%) | 9 (10.3%) | NS |
| Secondary osteoporosis | 45 (43.7%) | 23 (18.5%) | <.001 | 10 (20.0%) | 28 (32.2%) | <.001 |
| Rheumatoid arthritis | 9 (7.1%) | 8 (6.5%) | NS | 5 (10.0%) | 9 (10.3%) | NS |
| Parental hip fracture | 37 (35.9%) | 19 (15.3%) | <.001 | 16 (32.0%) | 14 (16.1%) | .013 |
| No clinical risk factors | 5 (4.8%) | 35 (28.2%) | <.001 | 0 (0%) | 32 (36.8%) | <.001 |
| Lumbar spine T-score | −1.1 (1.4) | −1.7 (1.4) | <.001 | −1.6 (1.4) | −1.4 (1.5) | NS |
| Femoral neck T-score | −1.0 (0.9) | −1.7 (0.9) | <.001 | −1.7 (0.7) | −1.6 (0.8) | NS |
| Total hip T-score | −1.3 (1.0) | −2.0 (1.1) | <.001 | −1.9 (1.0) | −1.9 (1.0) | NS |
| Lumbar spine osteoporosis | 16 (15.5%) | 38 (30.7%) | .009 | 11 (22.0%) | 27 (31.0%) | <.05 |
| Femoral neck osteoporosis | 5 (4.9%) | 20 (16.1%) | .007 | 4 (8.0%) | 7 (8.1%) | NS |
| Total hip osteoporosis | 16 (15.5%) | 59 (47.6%) | <.001 | 16 (32.0%) | 42 (48.3%) | .034 |
BMD, bone mineral density; BMI, body mass index; DXA, dual-energy X-ray absorptiometry; FRIDEX, Risk Factors and Densitometry by Dual-energy X-ray Absorptiometry; NOGG, National Osteoporosis Guideline Group; NS, not significant.
The application of the FRIDEX calibration in our sample would increase the cost of treatment by 60.7% in women over 65years of age, but would decrease it by 74.5% in those aged less than 65. In addition, there would be a savings of 64.6% in DXA in both groups and of 14.7% in treatment over 5years. The overall outcome would be a reduction in costs at 5years of 18.8%, equivalent to €352.4/patient (Table 2). This cost savings would be greater with the use of the NOGG guidelines, equivalent to a 5-year reduction of €725.4/patient, mainly because of the decrease in the number of densitometries indicated and treatments prescribed in women over 65years of age.
Comparison of Costs of the Approach Employed in the León Health Area and the Application of the FRIDEX Calibration and NOGG Guidelines.
| Sample | FRIDEX calibration | Difference in costs between FRIDEX and sample | NOGG guidelines | Difference in costs between NOGG and sample | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | € | n | € | % | €/patient | n | € | % | €/patient | |
| DXA | ||||||||||
| ≤65 years | 410 | 24,026 | 52 | 3047 | −87.3 | −51.2 | 120 | 7032 | −70.7 | −41.4 |
| >65 years | 197 | 11,544 | 163 | 9552 | −17.3 | −10.1 | 74 | 4322 | −62.6 | −36.7 |
| Total sample | 607 | 35,570 | 215 | 12,599 | −64.6 | −37.8 | 194 | 11,354 | −68.1 | −39.9 |
| Treatmenta | ||||||||||
| ≤65 years | 106 | 226,310 | 27 | 57,645 | −74.5 | −1591.1 | 73 | 155,855 | −31.1 | −664.7 |
| >65 years | 84 | 179,340 | 135 | 288,225 | +60.7 | +1296.3 | 56 | 119,560 | −33.3 | −711.7 |
| Total sample | 190 | 405,650 | 162 | 345,870 | −14.7 | −314.6 | 129 | 275,415 | −32.1 | −685.4 |
| Overall | ||||||||||
| 441,220 | 358,469 | −18.8 | −352.4 | 286,769 | −35.0 | −725.4 | ||||
The application of the FRIDEX calibration in our sample results in an improvement in the efficiency of the management of osteoporosis both at the diagnostic level and at the time of indicating drug therapy. Moreover, it reduces costs in comparison with routine clinical practice in the León health area.
The cost analysis includes the direct costs of DXA and 5years of drug therapy in accordance with the cost of DXA in Castile and León and the real treatment profile in Spain.11 The direct and indirect costs related to the fractures were not included in the assessment. In short, the use of the thresholds for the FRIDEX calibration in our sample would make it possible to save €37.4/patient in DXA and €314.6/patient in medication costs. The total expense (DXA and treatment) would be reduced over 5years by 18.8% with respect to the approach adopted in our area. In contrast, the NOGG guideline would reduce overall costs by 35.0% over 5years. This would mean a savings in our sample of €39.9/patient in DXA and €685.4/patient in treatment for 5years. In a study on the FRIDEX model, the overall costs decreased by 28.7% compared to the standard strategy based on DXA to detect the same number of women who had fractures.9
When the FRIDEX cost-effectiveness proposal is compared with the NOGG guideline thresholds for a population in the United Kingdom, it is observed that both recommendations reduce the number of DXA requested and that of prescribed treatments when compared with the approach adopted in our health area. However, the level of agreement between the two is low. Thus, although the absolute number of DXA and that of treatments that are indicated by the study do not differ much, the persons to which they are directed are different. The FRIDEX calibration recommends the measurement of BMD in older individuals with a high body mass index, whereas the NOGG guidelines are aimed mainly at persons who have more severe clinical risk factors. The FRIDEX proposal helps by identifying more cases of osteoporosis in the lumbar spine as well as in hip with respect to NOGG. Likewise, when it comes to suggesting therapy, the NOGG guidelines would indicate treating young persons in whom risk factors were detected, whereas the FRIDEX calibration would focus more on elderly individuals and on patients with osteoporosis involving the lumbar spine. Clinical practice guidelines should integrate in the best possible way the information from models that predict the risk of fracture to enable the identification of the individuals who would most benefit from bone densitometry. The purpose would be to evaluate risk more accurately, which would lead to a better selection of candidates for antiresorptive therapy.
The NOGG guidelines and FRIDEX calibration are based on the FRAX® score, the only tool that takes into account life expectancy and the epidemiological differences among countries.10 The thresholds proposed by the FRIDEX calibration are of interest as they focus on the Spanish population and are corroborated by cost-effectiveness studies with national considerations. Therefore, the use of these thresholds would be more appropriate than those concerning the British population. On the other hand, the NOGG guidelines are those with the best results, but they have not been validated for the Spanish population. They are different in that the intervention threshold is flexible, and varies depending on age, a parameter that is important in cost-effectiveness studies.16 However, in several studies, it has been seen that the NOGG guidelines are associated with difficulties when it comes to preventing fragility fractures, since, for example, elderly individuals should have an elevated risk as candidates for treatment, despite the fact that studies have demonstrated that the treatment in those patients is cost-effective with smaller thresholds.17,18 To make an accurate evaluation of the cost-effectiveness of guidelines, it is necessary to assess savings both over the short term—reduction in the number of bone densitometries and of prescribed treatment—and the long term, with savings related to fracture prevention.19 Thus, guidelines like those proposed by the NOGG, which are cost-effective over the short term, may not be over the long term, since they have the inconvenience of being less precise in their identification of high-risk patients, at least at the time of indicating whether or not they should be treated.18,20 This means that it is necessary to conduct national studies for the purpose of identifying the intervention thresholds at which the benefits of treatment, over both the short and the long term are maximized, while the risks and costs that accompany treatment are limited, always taking into consideration the amount society is willing to pay. In Spain, at the present time, according to FRAX®, there are no valid thresholds for high-risk of fracture. Moreover, providing a single value to represent the risk of fracture may not be wholly suitable, when the incidence of hip fractures can be up to 2-fold higher depending on the Spanish autonomous community.21 Until we have those thresholds, the proposal of the FRIDEX calibration may continue to have a role, as it is an improvement in the efficiency of the management of osteoporosis and better identifies densitometric osteoporosis in our setting than the British NOGG guidelines.
This report reveals the implications of the utilization of the NOGG guidelines and the FRIDEX calibration in the diagnostic and therapeutic efficiency in the management of osteoporosis in routine clinical practice, demonstrating a considerable heterogeneity among the recommendations for approaching this condition, which can influence decision-making concerning our patient population. However, it has certain limitations that we consider we should mention. First, the sample may have selection and reference biases, as it was made up of individuals who were referred to undergo DXA in accordance with the criteria of a physician. This may affect the results, since these persons have been subjected to some type of prior selection and the sample cannot be totally representative of the general population, compromising the external validity. However, this question would not affect analyses comparing different guidelines. Second, the Spanish version of the FRAX® tool has weaknesses, such as its underestimation of the risk of major fracture.22 The lack of robust Spanish epidemiological data concerning the incidence of major osteoporotic fractures has been approached through the application of the Swedish ratio of hip fractures to major fractures. However, the Spanish epidemiological findings on hip fractures and on nonvertebral and nonfemoral fractures indicate that, while the incidence of hip fractures in Sweden is approximately twice that reported in Spain, the frequency of the latter is relatively similar.11,22 This underestimation of the risk was one of the reasons why we decided to employ the British FRAX® when applying the NOGG decision thresholds in our study, taking into account the associated difference in risk assessment, as well.22,23 The British FRAX® tool duplicates risk in comparison with the Spanish version.23 As a result, the use of the latter would lead to a further underestimation of the risk of fracture when the NOGG thresholds are utilized. Third, the NOGG guidelines are validated for a specific population. This means that the characteristics may be different (prevalence of risk factors, fracture incidence, etc.), possibly compromising external validation and, thus, extrapolating the results requires caution. A fourth limitation is that the presence of silent vertebral fractures was not assessed, a fact that could affect therapeutic decisions based on the guidelines.
ConclusionsBoth the FRIDEX calibration and the NOGG guidelines have considerable heterogeneity. This signifies that there can be substantial variability in the number of individuals in which performance of DXA is recommended, as well as in those for whom the decision is made to initiate treatment. The use of either of them in our routine clinical practice would increase our efficiency in the management of osteoporosis, and we would achieve a significant reduction in costs. Nevertheless, further studies will help us to identify the intervention thresholds applicable in the Spanish population to maximize the cost-benefit.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Kyriakos G, Vidal-Casariego A, Quiles-Sánchez LV, Calleja-Fernández A, Ávila-Turcios D, Urosa-Maggi JA, et al. Estudio comparativo de la aplicación de la calibración FRIDEX y de la guía NOGG en el manejo de la osteoporosis en la práctica clínica habitual. Reumatol Clin. 2017;13:258–263.