In recent years, the prevalence of rheumatic diseases has increased. The virtual consultation of rheumatology could help to avoid unnecessary visits and attend those who need an early visit. The virtual consultation is associated with telemedicine and telecommunication. The objective of this study is to describe the characteristics of all virtual consultations performed in the Rheumatology Service during a one year period. More than a 50% were resolved without giving the patients an appointment. With virtual consultation we have achieved: (1) a closer contact with primary care, (2) rapid resolution of doubts about rheumatic disease in patients, (3) improvement of training in rheumatic disorders and (4) prioritizing those patients requiring early assessment by a rheumatologist.
La prevalencia de las enfermedades reumáticas ha aumentado en los últimos años y la consulta virtual de reumatología puede ser útil para reducir el número de visitas innecesarias y priorizar aquellas que requieran una atención precoz. La consulta virtual asocia la telemedicina y las telecomunicaciones. En este estudio se describen las características de las consultas virtuales realizadas a un Servicio de Reumatología en el periodo de un año, objetivándose que más de la mitad se pueden resolver sin necesidad de citar al paciente. Con la consulta virtual se ha conseguido: 1) tener un contacto cercano con el médico de atención primaria, 2) solucionar con rapidez las dudas sobre la enfermedad reumática de sus pacientes, 3) mejorar su formación en las enfermedades reumáticas y 4) priorizar a aquellos pacientes que requieran una valoración precoz por parte de un reumatólogo.
Rheumatic diseases constitute one of the first work disability causes and generate a socioeconomic impact that involves an elevated use of health care resources. 15 years ago, the EPISER study was performed.1 It was the first and only study on the prevalence and impact of rheumatic diseases on the Spanish adult population over 20 years of age. This study estimated that the prevalence of these diseases in Spain was of 22.6%, a higher prevalence than for other chronic diseases like hypertension and diabetes. Although there are no updated studies on the actual prevalence of rheumatic diseases in our area, the general perception is that they have increased, probably as a consequence of the population ageing. What we do have records of is that the demand for assistance in osteoarticular processes in the general population is constantly increasing, which has forced rheumatologists to start performing part of their health care activity in specialized care centres (SCC) and primary care centres in the last few years. However, and in spite of the increase in on-staff rheumatologists during the last 10 years, the public health system is not capable of covering the demand for osteoarticular disease health care required by our society.
We consider virtual practice an alternative health care model to respond to the increase of demand. Technological advances have favoured the development of this type of practice. It is one form of telemedicine that can be performed by phone, via video, computer, etc., and more and more countries are starting to implement this form of practice within their health care system.2
PurposeThe purpose of this study is to describe our experience with the virtual consultation of rheumatology and assess its advantages and disadvantages.
Materials and MethodsThis is an observational and retrospective study that assessed all virtual practices of rheumatology performed within the period of one year (from 1 April 2013 to 31 March 2014), requested by 44 primary care physicians corresponding to 3 health care centres, with a reference population of 70,693 inhabitants. Virtual practices were made through a computerized program called DRAGO. This program has been consolidated and accepted within the health care environment of the Autonomous Community of Canary Islands and it is used in clinical practice, both in primary care as well as in specialized care. The system develops a centralized medical record which is “unique” for the patient and has longitudinal and interdisciplinary character.
Primary care physicians performed an average of 5 virtual practices a day. These included a brief medical record, the question at issue and a link to the patient's most recent laboratory tests and X-rays. Practices were answered by an on-staff rheumatologist with more than 25 years of experience, with a maximum delay of 2 working days. When it was considered that the patient needed a rheumatologist assessment, an outpatient service rheumatology appointment was set up within the following 15 days at the latest. Suspicions of inflammatory disease or connective tissue disease were given preference. As part of the program assessment, we conducted satisfaction surveys among the primary care physicians involved in this project. They all have more than 10 years of experience and 60% of them having received training via MIR. The surveys were anonymous and optional.
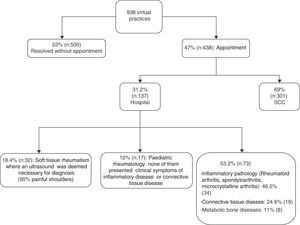
ResultsDuring the period of one year, there were a total of 938 virtual practices, more than half of which (53%; n=500) were resolved without the need for a patient's appointment at the rheumatology offices. Requests for virtual practices were not repeated for the same patient within a minimum period of 6 months after the first practice report. Consultations that were resolved through virtual practice were related to cases brought before the primary care physician, such as: (a) doubts regarding therapeutic options in cases of flare-ups of chronic diseases previously diagnosed by a rheumatologist, such as tendinosis, osteoarthritis and fibromyalgia; (b) doubts on the interpretation of laboratory investigations (for example: anti-nuclear antibodies title of 1/80 or borderline rheumatoid factor in patients without clinical background of inflammatory rheumatoid disease or connective tissue disease); (c) doubts regarding radiographic findings and (d) doubts regarding the path to follow in patients with metabolic bone diseases, mainly osteoporosis.
47% (n=438) of the practices requested by the primary care physician were considered cases that needed to be assessed at a rheumatologist office, so the patients were summoned. Out of these practices, 69% (n=301) were referred to the SCCs due to suspicion of fibromyalgia, soft tissue or degenerative disease, without detecting an inflammatory disease at the follow-up. The remaining 31% (n=137) were directly referred to the Rheumatology Service of the hospital due to: (a) suspicion of inflammatory disease or connective tissue disease, (b) a disease for which the performance of an interventionist or diagnostic musculoskeletal ultrasound was deemed necessary, or (c) patients younger than 16 years of age referred to a Paediatric Rheumatology Unit for assessment (Fig. 1). All the primary care physicians were given satisfaction surveys. The survey consisted of 8 questions with a score between 0 (highly disagree) and 4 (highly agree). 28 physicians (63.3%) answered the survey. More than 75% of them were satisfied with the virtual practice and 89% considered that it was conclusive (Table 1).
Satisfaction Surveys Summary.
| % | Highly disagree | Disagree | Agree | Highly agree |
|---|---|---|---|---|
| What score would you give to the virtual practice of rheumatology? | 7 | 18 | 50 | 25 |
| Does it seem efficient to you? | 3 | 7 | 75 | 14 |
| Do you think it contributes to your training? | 3 | 36 | 53 | 7 |
| Do you think it brings benefits to the patient? | 3 | 3 | 71.4 | 21.4 |
| Does it pose disadvantages? | 21.4 | 46.4 | 21.4 | 11 |
| Is the answer quick (less than 48hours)? | 3 | 25 | 43 | 28.5 |
| Do you think it is an ideal model to be implemented in other centres? | 7 | 11 | 46.4 | 36 |
| Would you change anything from this new model? | 7 | 32.1 | 46.4 | 14 |
This is the first study describing the experience with virtual practices of rheumatology in Spain. Currently, there are different autonomous communities, such as Catalonia, Madrid and Castile and León, implementing this system not only in the speciality of rheumatology, but also in other specialities.3 However, there is a shortage of publications on this subject.
Virtual practice started to be implemented as a health care alternative in rural geographical areas or in areas distant from the city to facilitate the access by the resident population of that area to the health care service.4–6 Thus, it was possible to provide coordinated assistance with the participation of the patient, the primary care physician and the specialist. Currently, it is also being implemented in urban areas due to the increase in health care demand. Radiology and dermatology were the pioneers of telemedicine, and more and more specialities are implementing it.7,8
Rheumatology practices have experienced a change in the last decade due to an increase in the prevalence of locomotor system diseases and rheumatology has gone from being an exclusively hospital speciality to currently having a great part of its activity dealt with in outpatient offices outside the hospital. The virtual practice of rheumatology development seems to be a promising bet due to its efficiency, efficacy and effectiveness.9,10 Davis2,6 made a review of telemedicine in rheumatology to assess its sustainability, feasibility and applicability and reached positive conclusions: good development of patient, primary care physician and specialist communication was obtained and, on the other hand, it also seemed to be cost/time effective although this interpretation may vary depending on the technology used and the cost to implement it. In this Davis study,6 84% of the patients were satisfied with the virtual practice. Although the general first impression is that telemedicine would imply savings and not expenses, there are also some studies that indicate otherwise.6,11,12 Legget13 et al. carried out a prospective study evaluating the primary care physician and specialist's patient diagnosis and satisfaction from 100 virtual practices performed by phone and via video-conference. The specialist set up appointments at the office for 75% of the patients after the virtual practice by phone and for 6% of them when it was via video conference. It was demonstrated that diagnostic accuracy exceeded 60% and reached 97% for practices performed via video conference and 71% for practices performed by phone. On the other hand, patient satisfaction with virtual practices was lower than the doctors’ but exceeded 50%. Virtual practice was rated as worse when it was performed by phone, but patients are satisfied if the practice is performed via video conference, since they do not perceive a lack of care for their health.14,15 Other authors5 state that the ideal model would be a mixed model in which virtual practice and physical practice are present.
We have also described virtual practice in paediatric rheumatology and the prevalence of chronic rheumatic diseases in children is higher every time. Measures such as conducting training programs regarding rheumatic diseases for primary care physicians and paediatricians working in rural health care centres away from the city or educating the child and their relatives on line to help them face the disease may help improve their health condition.16
In our study, virtual practice was performed between the primary care physician and the specialist and they were able to quickly identify patients that really needed an early treatment or quick assessment. Although no analysis has been performed to assess the costs, no extra expenses have been accrued on this form of communication because it was already implemented before the virtual consultation started. The amount of first visits and follow-up visits decreased significantly although the main purpose of virtual practice is not to reduce the waiting list, but to avoid delay in the diagnosis and treatment of rheumatic diseases. We agree with other authors in their opinion14 that virtual practice implies a series of advantages: it facilitates contact with the primary care physician, thus contributing to improve the training regarding the locomotor system diseases, it encourages team work, it makes the first visit with the rheumatologist more efficient since he can advise the primary care physician beforehand on the additional tests he should request, avoiding unnecessary additional tests, and it helps to identify those patients that really need an urgent visit. In a study7 carried out in Canada, virtual practices from several specialities were assessed and they showed that the waiting list was reduced to almost half. This favoured patients who really needed a preferred visit since they could get a visit quickly. Virtual practice presents positive aspects but it also poses disadvantages: rheumatology is mainly a clinical speciality and, in these cases, we do not have direct contact with the patient, we cannot perform a medical history or a directed medical record and we have to rely on information provided by the primary care physician. For this reason, it is important to stress that, in our case, in the face of the slightest diagnostic or therapeutic doubt, we set up an appointment for the patient at the rheumatology's outpatient office.
On the other hand, and focusing on the items which were more negatively assessed in the survey, the disadvantages stated by some of the primary care physicians are related to the reiterative demand, by many patients, to be assessed by the specialist. In many occasions, patients need to see a specialist to be reassured regarding their disease, even though they have been previously diagnosed by the rheumatologist with some musculoskeletal disease which does not require a specific follow-up or even when the primary care physician does not have any doubts regarding diagnosis and treatment.
Moreover, not all primary care physicians agree with the training aspect of the virtual practice, although the reasons are not stated in the survey. However, from our point of view, if used correctly, this is a tool that is useful to provide teaching and advice on how to handle the different rheumatic diseases and thus avoid unnecessary additional tests and transfers for the patient.
This study has an obvious limitation: no patient satisfaction surveys have been performed and their opinion is very important for this practice system to work and develop in the future.
ConclusionsOur experience with virtual practice is positive if we omit the limitation derived from the lack of contact with the patient. We have achieved: (1) quick resolution of doubts raised to the primary care physician, (2) contribution to a better training on locomotor system diseases, (3) health care overload prevention, (4) more efficient first visits and (5) early detection of inflammatory diseases that really need an early treatment or assessment.
Ethical ResponsibilitiesProtection of people and animalsAuthors state that no experiments were performed on human beings or animals as part of this investigation.
Confidentiality of dataAuthors state that this article does not contain patient data.
Right to privacy and informed consentAuthors state that this article does not contain patient data.
Conflict of InterestsThe authors declare that there are no conflicts of interest.
Please cite this article as: Tejera Segura B, Bustabad S. Una nueva forma de comunicación entre reumatología y atención primaria: la consulta virtual. Reumatol Clin. 2016;12:11–14.