To analyze the perceptions of Spanish rheumatologists, experts in spondyloarthropathies (SpA), on the role of exercise in these and in other rheumatic diseases.
MethodsA survey to 106 rheumatologists belonging to an SpA working group of the Spanish Society of Rheumatology, GRESSER, was collected. The questions were related with general aspects of professional exercise (clinical practice and generic knowledge), use of fitness in SpA (benefits, indications, contraindications, compliance, facilitators), sociodemographic characteristics and professional experience with the respondents’ exercise regimen. A descriptive analysis was performed.
ResultsThe survey was sent to 106 rheumatologists, 44 of them answered (51% female, over 20 years of experience). Over 86% believe that their patients need exercise, but the prescription is moderate. 42% believe they do not have training to prescribe specific exercises. The physical activity education materials available consisted essentially of brochures (90%), websites (52%) and videos (23%). The therapeutic importance of exercise depends on the type of underlying disease. Most agree in decreasing the intensity of exercise during disease flares. For most cases of Spa, exercise is not a trigger of flares (66%), and may be used at any stage of the disease, depending on the type and the phase of the Spa.
ConclusionsRheumatologists consider exercise as a fundamental part of the treatment of rheumatic patients, but greater knowledge and development of specific strategies in its prescription is required.
Analizar las opiniones de reumatólogos españoles expertos en espondiloartritis (EspA) sobre el papel del ejercicio en este tipo de enfermedades y en otras enfermedades reumáticas.
MétodosSe envió una encuesta a 106 reumatólogos pertenecientes al grupo de trabajo en EspA de la Sociedad Española de Reumatología, GRESSER. Se preguntó sobre aspectos generales del ejercicio (práctica clínica habitual y los conocimientos genéricos), práctica de ejercicio en las EspA (beneficios, indicaciones, contraindicaciones, adherencia, facilitadores) y las características sociodemográficas, profesionales, experiencia con el ejercicio, del encuestado. Se realizó un análisis descriptivo.
ResultadosLa encuesta se envió a 106 reumatólogos, de los que contestaron 44 (51% mujeres, y más de 20 años de experiencia). Más del 86% considera que sus pacientes necesitan realizar ejercicio, pero su prescripción es moderada. El 42% no tienen formación para la prescripción de ejercicios concretos. El material educativo sobre actividad física disponible consiste fundamentalmente en folletos (90%), páginas web (52%) y vídeos (23%). La importancia terapéutica del ejercicio depende del tipo y de la enfermedad de base. La mayoría coincide en disminuir la intensidad del ejercicio en los brotes de la enfermedad. Para la mayoría, en las EspA el ejercicio no es un factor desencadenante de brotes (66%) y debe utilizarse en cualquier fase de la enfermedad, el tipo depende de la fase de la EspA.
ConclusionesLos reumatólogos consideran el ejercicio una parte fundamental del tratamiento de los pacientes reumáticos, aunque se precisa un mayor conocimiento y desarrollo de estrategias específicas de prescripción del ejercicio en Reumatología.
The World Health Organization considers physical inactivity to be a risk factor for mortality and, thus, recommends an active role for health professionals in promoting exercise.1
In spondyloarthritides (SpA), not only has exercise been shown to relieve symptoms of disease and improve functional capacity and quality of life, it could prevent the development of deformities. The importance of exercise in these processes has led to the inclusion of specific recommendations for performing physical activity in different consensus statements on the management of SpA issued by international organizations.2–6
The response to exercise is determined by a number of components (frequency, intensity and duration), but also depends on the patient's adherence to, or compliance with, the prescribed program.7–12 The results of a Cochrane review show that exercise programs in ankylosing spondylitis (AS) fail to comply with the current recommendations, that the measurement of the efficacy is inadequate and that adherence is evaluated in few cases.13 Although compliance varies depending on the definition and the means used to measure it, some studies report it to be around 50% in AS.14
Poor adherence to exercise regimens by patients is multidimensional. In addition to their low expectations, little motivation and limited understanding of the exercises, other possible factors are the pain they experience and their lack of time, aspects that should be taken into account when prescribing any program.15,16 Patient compliance can also be affected by the difficulties faced by the physiotherapists themselves, who need to resolve the confrontation between accepted patient care standards and those that each professional judges to constitute best clinical practice. Thus, the main problems stemming from this lack of agreement is the professional's freedom and the need to individualize physiotherapy.17
In contrast to the approach to disease prevention in healthy young individuals, the range of options for the therapeutic management of physical activity in patients with chronic diseases may be limited. When prescribing exercise, physicians should be familiar with the physiological mechanisms and the underlying principles that enable an exercise regimen to act on the organism, as well as with the barriers that impede patients from carrying it out. On the other hand, the adaptation of the exercise program should be based on the patient's physical status and on establishing, together with the patient, the program of goals to achieve. Despite the available evidence,5,10,12,18 rheumatologists are not trained in techniques related to physical activity and sports.19,20 Their recommendations to patients concerning the need to exercise are usually general, without a prescription based on clear guidelines; rather they are substantiated by their own experience. Thus, it is important to record and analyze the opinions of rheumatologists regarding exercise in general and programs specific for SpA in order to improve the prescription of individualized programs and promote adherence to them.
The objective of this report is to know the opinions, perceptions and assumptions of Spanish rheumatologists, experts in SpA, concerning the role of exercise in diseases of this type and in other rheumatic diseases. The results of this study will make it possible to define criteria for the prescription of adequate exercise programs in patients with SpA and to develop effective prescribing strategies.
Material and MethodsDesignWe carried out a survey, designed on the basis of educational material and consensus statements on exercise provided by the department of rheumatology and rehabilitation of Hospital Universitario Fundación Alcorcón in Madrid, Spain. This survey was sent by e-mail, using an online platform (SurveyMonkey), to the 106 rheumatologists that make up the SpA working group of the Spanish Society of Rheumatology (GRESSER).
VariablesWith respect to the variables, the survey, shown in its entirety in Banexo Appendix A (available online), is made up of 2 large blocks of questions regarding different aspects of exercise, both general and for rheumatic diseases, and specific for SpA, in addition to a third block on the characteristics of the professional being surveyed. There are different types of responses: dichotomous (yes/no), categorical and scores obtained from a Likert scale ranging from 0 to 10.
The information to be extracted from each of the blocks of questions was focused on the following subjects: (a) general aspects of exercise (routine clinical practice in relation to exercise) such as the number of patients who need exercise, the type of exercise prescribed, qualifications of the rheumatologist to recommend exercise, specialists or related professionals to whom the patients are referred (rehabilitation providers, physical therapists, etc.), degree of accessibility of these specialists or professionals, and availability of material utilized in exercise; (b) generic knowledge regarding exercise, independent of routine clinical practice: definitions of exercise and physical activity, factors related to exercise performance, the impact of the latter on different chronic rheumatic diseases, effect of stretching and strength training, effect of exercise on specific symptoms of chronic rheumatic diseases, management during flares and factors that improve compliance; (c) opinion on performance of physical activity in SpA: moments or stages of the disease in which patients should exercise, beneficial effects in SpA, indication andcontraindication for specific exercises depending on the stage or moment of the disease; (d) characteristics of the survey respondents: sociodemographic (age and sex), position in the present department, personal experience with exercise and with other professionals whose specialties are related to it, etc.
Statistical AnalysisFollowing the process of encoding the variables, the data were introduced into a computerized database and were cleaned. Subsequently, a descriptive analysis was carried out using measures of central tendency (mean, median) and of dispersion (standard deviation and interquartile range) for continuous variables, and the categorical variables are expressed as frequency distribution and percentage.
Ethical AspectsThis study is based on the responses to an anonymous survey on the part of members of the SpA working group of the Spanish Society of Rheumatology (GRESSER). As completion of the survey was voluntary, the decision to participate was assumed to constitute a de facto consent by the professionals who responded. The study was carried out following the precepts of the guidelines for good clinical practice and the principles of the latest revision of the Declaration of Helsinki, and was submitted for approval to a clinical research ethics committee (CREC).
ResultsThe survey was completed by a total of 44 rheumatologists (Table 1), with a slight predominance of women (51%), a mean age of 47±6 years, an average of 20 years of professional practice and an average of 20 new patients and 54 patients already in treatment per week. The majority of the responders were associate physicians (77%) and their personal experience with exercise was good (78%); they devoted more than 3h a week to aerobic exercise (27%) or to strength or resistance training (56%). These findings are shown in detail in Banexo Appendix A (available online).
Characteristics of the Rheumatologists Surveyed.
| Continuous variables | n | Mean (SD) | Median (IQR) |
|---|---|---|---|
| Age | 41 | 46.7 (6.3) | 46 (42–52) |
| Relationship to the exercise specialists in the same center (0–10) | 41 | 5.7 (2.1) | 6 (5–7) |
| No. of years of professional practice (including residency) | 41 | 20.7 (6.4) | 20 (15–25) |
| No. of new patients per week | 40 | 19.7 (13.7) | 20 (10–25) |
| No. of patients already in treatment per week | 40 | 54 (17.0) | 55 (41–67) |
| Categorical variables, n (%) | |||
| Sex | |||
| Men | 20 (48.8) | ||
| Women | 21 (51.2) | ||
| Current professional status | 39 | ||
| Resident | – | ||
| Associate | 30 (76.9) | ||
| Section head | 7 (17.9) | ||
| Department head | 5 (5.1) | ||
| Other professional position | |||
| Fellow | 1 (50) | ||
| University teacher | 1 (50) | ||
| Personal experience with exercise | 41 | ||
| Good | 32 (78.0) | ||
| None | 1 (2.4) | ||
| Limited | 8 (19.5) | ||
| Type of exercise usually performed | 41 | ||
| Aerobic | 11 (26.8) | ||
| Strength training | 23 (56.1) | ||
| Combination | 2 (4.9) | ||
| Usually no exercise of any type | 5 (12.2) | ||
| Average time devoted to exercising (per week) | 41 | ||
| Zero | 1 (2.4) | ||
| Less than 1 hour | 4 (9.8) | ||
| 1–3h | 4 (9.8) | ||
| 3–6h | 13 (31.7) | ||
| More than 6h | 19 (46.3) | ||
IQR: interquartile range; SD: standard deviation.
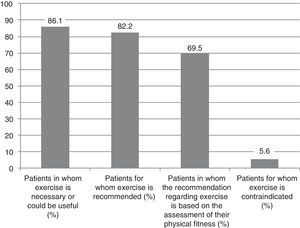
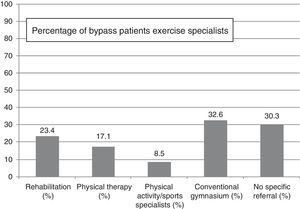
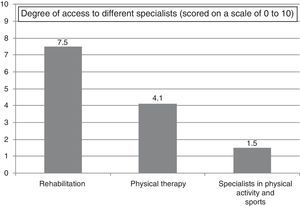
Despite the fact that the surveyed rheumatologists calculated that more than 86% of their patients needed to perform physical exercise (Fig. 1), the rate of exercise prescription was moderate, with 23% of the patients being referred for rehabilitation and 17% for physical therapy (Fig. 2). The rheumatologists reported having good access to rehabilitation providers (7/10), moderate access to physiotherapists (4/10) and practically no access to other physical activity or sports specialists (1/10) (Fig. 3).
The majority considered that the referral of a patient to the rehabilitation service for a demonstration of how exercise should be performed is the best format for recommending exercise—better than brochures, the Internet, videos or a demonstration on the part of the rheumatologist.
On the other hand, 93% of the rheumatologists considered that they could recommend exercise programs to their patients, although only 68% believed themselves to be qualified to suggest particular exercises and a little over 60% devoted a specific part of their patients’ visits to aspects related to exercise. Finally, the educational material on physical activity available in the rheumatologist's office consisted basically of informative brochures (90%) and, to a lesser extent, websites (52%) and videos (23%).
Generic Knowledge About Exercise, Independent of Routine Clinical PracticeThe majority of the participants (95%) acknowledged that the terms “physical activity”, “exercise” and “sports” were not synonyms, and that the concept “dose” was also applicable to exercise (62%). On a scale of 0 to 10, the factors considered most important when recommending exercise to rheumatic patients were the disease stage (8.7), the joints involved (8.5), patient preferences and patient access to exercise (8.3).
The therapeutic importance of exercise depended on the type and on the underlying disease. For example, aerobic exercise was especially important in fibromyalgia and osteoporosis (7.3), stretching in SpA (8.7), strength training in osteoarthritis of the knee (8.7) and active-assisted exercise in rheumatoid arthritis (7) and in soft tissue diseases (6.9). On the other hand, the beneficial effects of exercise were especially evident in functional limitation, self-care, quality of life and physical fitness, whereas its impact on pain was less marked. The greatest benefit of exercise was observed in patients with inflammatory disease of the axial skeleton, although when evaluating this finding, we must take into account the type of rheumatologists being surveyed (experts in SpA). On the other hand, the general opinion was that exercise prescription should be specific for the different groups of patients, although there was no agreement on whether prescribing should be carried out exclusively by exercise specialists, nor was there consensus on the nature of the beneficial effect or effects of stretching and strength training.
The majority of the respondents coincided in that the correct approach during inflammatory episodes was to reduce the exercise intensity, and considered that the most important factors for improving adherence were accessibility to the performance of exercise (8.7), information on the goals and benefits (8.5) and the characteristics of the patients themselves (8.3).
Exercise in SpondyloarthritidesThe general opinion of the rheumatologists was that, in patients with SpA, exercise was not a factor in the triggering of flares (66%), and they all coincided in that it should be put into practice at any stage of the disease, although there was not much agreement on whether or not its performance can delay the initiation of drug therapy.
The assessment of the beneficial effects of exercise scored over 8 out of 10 for most of the characteristics of SpA, such as spinal and joint flexibility, chest expansion, posture, muscle strength, aerobic capacity, exercise tolerance, respiratory function, functional limitation, depression, self-care and quality of life (Table 2). However, it was not considered so beneficial for the inflammation or disease activity associated with SpA, or for the radiological and structural lesions.
Spondyloarthritides: Beneficial Effect (0–10) on Different Aspects of the Disease.
| n | Mean (SD) | Median (IQR) | |
|---|---|---|---|
| Beneficial effects (0–10) of exercise on: | |||
| Spinal mobility | 40 | 8.4 (1.5) | 9 (7–9) |
| Joint mobility | 40 | 8.1 (1.5) | 8 (7–9) |
| Chest expansion | 40 | 8.2 (1.4) | 8 (8–9) |
| Posture | 40 | 8.4 (1.2) | 8 (8–9) |
| Muscle strength | 40 | 8.5 (1.1) | 9 (8–9) |
| Physical fitness (aerobic capacity) | 40 | 8.7 (1.1) | 9 (8–9) |
| Fatigue and exercise tolerance | 40 | 8.4 (1.1) | 8 (8–9) |
| Respiratory function | 40 | 8.2 (1.1) | 8 (7–9) |
| Stiffness and functional limitation | 40 | 8.3 (1.2) | 8 (7–9) |
| Pain | 40 | 7.2 (1.3) | 7 (6–8) |
| Depression and self-esteem | 40 | 8.3 (1.2) | 8 (8–9) |
| Inflammation | 39 | 4.9 (2.3) | 5 (3–7) |
| Radiological or structural lesion | 39 | 3.6 (2.6) | 8 (8–9) |
| Self-care | 40 | 8.3 (1.0) | 8 (8–9) |
| Quality of life | 40 | 8.3 (1.3) | 8 (8–9) |
| Anxiety | 39 | 7.7 (1.6) | 8 (7–9) |
| Disease activity | 37 | 5.1 (2.0) | 5 (4–6) |
| Sleep | 39 | 7.6 (1.6) | 8 (7–9) |
| Beneficial effects (0–10) on the characteristics of spondyloarthritides | |||
| Spinal and joint flexibility | 39 | 8.3 (1.5) | 9 (8–9) |
| Chest expansion | 39 | 8.1 (1.4) | 8 (8–9) |
| Posture | 38 | 8.3 (1.2) | 8 (8–9) |
| Muscle strength | 39 | 8.3 (1.2) | 8 (8–9) |
| Physical fitness (aerobic capacity) | 39 | 8.5 (1.0) | 8 (8–9) |
| Fatigue and exercise tolerance | 39 | 8.3 (1.2) | 8 (7–9) |
| Respiratory function | 39 | 8.0 (1.1) | 8 (7–9) |
| Stiffness and functional limitation | 38 | 8.4 (1.2) | 8 (8–9) |
| Pain | 39 | 7.1 (1.4) | 7 (6–8) |
| Depression and self-esteem | 39 | 8.1 (1.3) | 8 (7–9) |
| Inflammation | 39 | 5.3 (2.5) | 6 (3–7) |
| Radiological or structural lesion | 38 | 4.0 (2.8) | 4 (1–7) |
| Self-care | 38 | 8.5 (1.1) | 9 (8–9) |
| Quality of life | 39 | 8.4 (1.0) | 9 (8–9) |
| Indication for exercise according to the disease stage (0=contraindicated; 10=absolute indication) | |||
|---|---|---|---|
| Initial stage | Intermediate stage | Advanced stage | |
| Aerobic | 7.7 (2.3) | 7.2 (1.9) | 5.8 (2.6) |
| Stretching | 7.9 (1.8) | 8.2 (1.5) | 7.6 (1.9) |
| Strength training | 7.8 (1.9) | 7.6 (1.7) | 6.9 (2.0) |
| Global postural reeducation | 7.3 (2.8) | 7.9 (1.9) | 7.8 (1.6) |
| Physical means (TENS, thermotherapy, etc.) | 4.2 (2.5) | 5.5 (2.1) | 6.7 (2.3) |
| Spinal manipulation | 2.9 (2.5) | 2.8 (2.5) | 2.1 (2.5) |
| Balneotherapy | 4.1 (2.4) | 5.0 (2.3) | 6.8 (2.4) |
| Occupational therapy | 4.3 (2.6) | 5.5 (2.1) | 7.5 (1.9) |
| Breathing exercises | 6.1 (2.7) | 7.9 (1.7) | 8.7 (1.3) |
| Proprioceptive exercises | 4.9 (2.8) | 6.0 (2.2) | 6.9 (2.0) |
| Postural exercises | 6.7 (2.9) | 7.8 (1.8) | 8.0 (1.6) |
IQR: interquartile range; SD: standard deviation; TENS: transcutaneous electrical nerve stimulation.
Finally, the indication for exercise varied depending on the stage of the disease (Table 3). The rheumatologists considered types of exercise like aerobic, stretching and strength training to be especially indicated during the initial stage; during the intermediate stage, the approaches of choice were stretching, global postural reeducation, and breathing and postural exercises; the latter 2 were also those most suitable for the advanced stage of the disease. With regard to other nonpharmacological measures, the rheumatologists surveyed judged spinal manipulation to be contraindicated in all the stages of SpA. Other procedures such as physical means, balneotherapy and occupational therapy were not considered to be clearly indicated during the initial or intermediate stages.
Indication for Exercise and Physical Therapy According to the Stage of Spondyloarthritis (0=Contraindicated; 10=Absolute Indication).
| Initial stage | Intermediate stage | Advanced stage | |
|---|---|---|---|
| Aerobic (n=39) | 7.7 (2.3) | 7.2 (1.9) | 5.8 (2.6) |
| Stretching (n=39) | 7.9 (1.8) | 8.2 (1.5) | 7.6 (1.9) |
| Strength training (n=39) | 7.8 (1.9) | 7.6 (1.7) | 6.9 (2.0) |
| Global postural reeducation (n=39) | 7.3 (2.8) | 7.9 (1.9) | 7.8 (1.6) |
| Physical means (TENS, thermotherapy, etc.) (n=39) | 4.2 (2.5) | 5.5 (2.1) | 6.7 (2.3) |
| Spinal manipulation (n=39) | 2.9 (2.5) | 2.8 (2.5) | 2.1 (2.5) |
| Balneotherapy (n=39) | 4.1 (2.4) | 5.0 (2.3) | 6.8 (2.4) |
| Occupational therapy (n=39) | 4.3 (2.6) | 5.5 (2.1) | 7.5 (1.9) |
| Breathing exercises (n=39) | 6.1 (2.7) | 7.9 (1.7) | 8.7 (1.3) |
| Proprioceptive exercises (n=39) | 4.9 (2.8) | 6.0 (2.2) | 6.9 (2.0) |
| Postural exercises (n=39) | 6.7 (2.9) | 7.8 (1.8) | 8.0 (1.6) |
TENS: transcutaneous electrical nerve stimulation.
In this study, we analyze the opinions of and approaches to exercise in patients with rheumatic and musculoskeletal disease offered by a group of Spanish rheumatologists, experts in SpA.
First of all, we consider it striking that, although according to the responders to the survey, a very large percentage of their patients would benefit from exercise, as reported in the medical literature,21,22 the rate of referral to specialists in physical exercise and sports is not very high. This may be due to a number of factors, including the perception that the recommendations and explanations concerning exercise given during consultations are sufficient, or the search for greater autonomy on the part of the patients. However, we cannot rule out other possibilities, for example, the effects in some centers of a waiting list for access to rehabilitation, or the nonexistence of protocols that clearly indicate which patients should be referred to a specialist and when, or the lack of specific training of rheumatologists in this aspect.
With respect to the different formats for recommending exercise (including brochures and videos), the majority are considered to be relatively useful, although the demonstration on the part of a rehabilitation provider is thought to be the most effective approach. There is evidence of the efficacy of different methods of recommending exercise, although its quality is moderate,23 it usually focuses only on the short-to-medium term and does not always reflect other aspects that can play a role, such as the duration of patient visits, the extent to which the Internet is used, etc.
All the rheumatologists coincide in that, depending on the underlying disease, exercises of one type or another should be recommended, as is pointed out by different organizations.4,24–26 In this block of questions, there is a notable variability in the descriptions of the beneficial effects of stretching exercises and strength training. To this we should add the finding that a high percentage of responders do not consider themselves competent enough to recommend specific exercises. All this may indicate the need to attain a greater understanding of the bases and benefits of exercise. Similar results have been reported by others in settings like ours.27
On the other hand, in rheumatic diseases, there is a majority opinion with regard to the need to reduce the intensity of exercise when acute inflammation develops, but that bedrest is not required. There are data that coincide with the published evidence and the recommendations issued to date in this respect.12,24
In relation to the findings specific for SpA, the majority of those surveyed stress the beneficial role that exercise can play in multiple symptoms and signs of the disease, such as spinal and joint mobility, fatigue, stiffness, self-care and sleep. Likewise, the majority of the responders do not consider exercise to have a relevant role in the inflammation and structural damage that these patients develop. A systematic review of the literature on the effects of different exercise modalities on AS points out that it can have a moderate to good efficacy in different aspects of the disease, especially mobility and function, but also in activity as measured by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, it is important to stress that the studies on which these affirmations are based are small, and that the results are not always statistically significant, a circumstance that limits the validity of the conclusions.12 Another recent systematic review also demonstrates that exercise may have a beneficial effect on inflammation in AS, although it also concludes that, as yet, its effect on other types of SpA is unknown.28
Continuing with the discussion of the disease activity in SpA, there is no general agreement as to whether exercise can trigger a flare of the disease; two thirds of those surveyed reject this idea. To date, the data in the literature have been unable to demonstrate the existence of an association between exercise and the onset of flares.29,30 Likewise, there is no agreement as to whether or not exercise can delay the initiation of treatment, a question that remains unresolved in the literature. One aspect in which all the responders coincide is in the need to recommend exercise to patients with SpA, regardless of the disease course. In relation to other nonpharmacological measures, the level of recommendation of spinal manipulation is very low, a circumstance that coincides with the majority of the current guidelines and consensus statements.4,30 In an intermediate point, we find physical means and balneotherapy. Finally, in the early stages, aerobic exercises, strength training and stretching are those most widely recommended, whereas exercises aimed at improving respiratory function, occupational therapy and postural exercises are reserved for patients with more advanced disease. The approach employed is very similar to those proposed in the Spanish guidelines.
On the other hand, these findings should be interpreted with caution. One of the major limitations of the present study is the fact that the survey was sent to a small number of rheumatologists who belong to a SpA working group. Although these professionals can treat patients with rheumatic diseases of all types, their experience in SpA may mean, at least a priori, that they have a greater knowledge of the study subject than the general population of rheumatologists in Spain. Then again, the low percentage of participation on the part of the rheumatologists invited may have some effect on the results. Nevertheless, there were no differences between the responders and the nonresponders in terms of sex or the Spanish autonomous communities in which they lived, there being no other data on which to base a comparison between the two groups. Finally, the lack of information on the recommendation of specific exercise programs or evaluation of the degree of compliance with them may contribute to the apparent contradiction between the widespread knowledge of the beneficial effects of exercise and the low rate of referral of patients to the specialists in that area.
In conclusion, although there is general agreement on the beneficial effects of exercise in rheumatic diseases, including SpA, a greater understanding of these effects and the design of protocols for exercise regimens are needed.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest involving any of the laboratories that could be related to the objective of this manuscript either directly or indirectly (agencies, scientific societies or publishing companies), or through institutional (governmental) agencies, foundations or private entities.
This project was funded by an unrestricted grant from Merck Sharp & Dohme de España, S.A.
The SpA working group of the Spanish Society of Rheumatology.
Please cite this article as: Zarco P, Florez M, Almodóvar R, Grupo Gresser. Opinión de los reumatólogos españoles expertos en espondiloartritis sobre el papel del ejercicio en la espondilitis anquilosante y otras enfermedades reumáticas. Reumatol Clin. 2016;12:15–21.