Adult Still's disease (ASD) was described by George Still in 1896. ASD is a rare inflammatory disorder, of unknown etiology, whose clinical manifestations are manifold. Diagnosis requires high clinical suspicion and exclusion of different etiologies. We report the case of a 20 year old male with fever, arthritis, dyspnea and chest pain. Laboratory findings showed increased levels of cardiac enzymes, and a pleuropericardic effusion was detected in imaging tests, both of them showing myopericarditis. Corticosteroid treatment was started with initial improvement, although the addition of methotrexate was necessary in the following months.
La enfermedad del Still del adulto (ESA) fue descrita en niños por George Still en 1896. La ESA es una entidad inflamatoria, infrecuente, de etiología desconocida cuyas manifestaciones clínicas son múltiples. El diagnóstico requiere una alta sospecha clínica y la exclusión de diferentes etiologías. Presentamos el caso de un varón de 20 años que consultó por fiebre, artritis, disnea y dolor costal. Se objetivaron elevación de enzimas cardiacas, y en las pruebas de imagen, derrame pleuropericárdico compatibles con miopericarditis. Se inició tratamiento con corticoides con mejoría inicial, precisando en los meses posteriores la adición de metotrexato.
Adult Still's disease (ASD) is more common in young adults. We report the case of a man 20 years with cardiac manifestations as initial presentation.
Case ReportWe report the case of a 20 year old male, without past medical history who was admitted because of 3 weeks with fever, joint pain in the spine, shoulders and wrists, right rib pleuritic pain, dyspnea and orthopnea. The examination revealed cutaneous-mucous pallor, tachypnea, jugular venous distention, latero-cervical lymphadenopathy, systolic murmur, pericardial friction rub, bibasal hypophonesis, hepatosplenomegaly and bilateral malleoli edema.
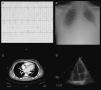
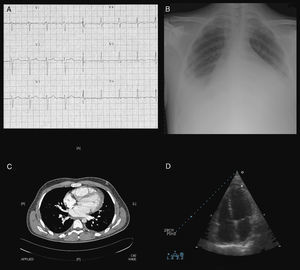
Laboratory tests revealed hemoglobin 9.3g/dl, WBC 33200/mm3 (93.8% neutrophils), platelets 512000/mm3, prothrombin activity 51.9%, AST 177U/l, ALT 108U/l, gamma-glutamyl transpeptidase 225U/l, LDH 1044U/l and troponin I 3ng/ml. C-reactive protein was 262.8mg/l, ESR 97mm/h and ferritin 37640ng/ml. Thyroid hormones, immunoglobulins and complement were normal. Rheumatoid factor, ANA, extractable nuclear antigen, anti-nDNA, antineutrophil cytoplasmic and antiphospholipid antibodies were negative. Serology, blood cultures, urine cultures and Mantoux testing was negative. A blood smear showed no abnormalities. Arterial blood gas showed partial respiratory failure. Electrocardiogram revealed sinus tachycardia with negative T in V4–6 (Fig. 1A). A chest radiography (Fig. 1B) showed global cardiomegaly and bilateral pleural effusion. Exudative pleural fluid, with smears, cultures and cytology were negative. The horaco-abdominal CT (Fig. 1C) revealed minimum pleuropericardial effusion, cardiomegaly and hepatomegaly. The echocardiogram (Fig. 1D) revealed mild-moderate pericardial effusion, an ejection fraction of 41% of the left ventricle, moderate-severe mitral regurgitation and mild to moderate mitral stenosis.
Studies that showed the presence of myopericarditis: sinus tachycardia and negative T waves in V4–V6 ECG (A), global cardiomegaly and bilateral pleural effusion on chest X-ray (B), pleuropericardial effusion and cardiomegaly on thoraco-abdominal CT (C), mild to moderate pericardial effusion on echocardiography (D).
The presence of pericardial chest pain, physical examination characteristics and elevated cardiac enzymes were consistent with myopericarditis. Treatment was initiated with NSAIDs and broad-spectrum antibiotics to cover infectious etiology. Given the presentation with fever, arthritis, liver dysfunction, leukocytosis, pleural and organ enlargement, ASD was diagnosed by the criteria proposed by Yamaguchi and intravenous bolus of corticosteroids started, followed by oral prednisone in a descending pattern. Progressive improvement was shown in clinical, biochemical, radiological (normal) and echocardiography (mild pericardial effusion and grade II mitral insufficiency with Valsalva) parameters. Later, coinciding with the decline of prednisone dosage, an outbreak similar to the initial one occurred, which improved with an increase of prednisone, leading to the addition of methotrexate, which helped to stabilize the disease and lower the dose of prednisone.
DiscussionFever is the most common clinical manifestation of ASD, followed by arthritis of the knees and wrists.1 Our patient has not presented an evanescent rash with fever that is typical and frequent. Up to 30–40% of cases have serosal involvement.2–7 Pericarditis is the most common cardiac manifestation and is usually subclinical in up to 50%. Myocarditis is rare and can cause arrhythmias. Other, exceptional manifestations are cardiac tamponade, constrictive pericarditis or endocarditis. Hepatic dysfunction is common with cytolysis pattern, usually mild to moderate, and in our patient was associated with impaired coagulation.
The characteristic elevation of acute phase reactant ferritin, considered a marker of active disease and response to treatment, does not occur in other rheumatic diseases.8
The diagnosis9 is clinical, with Yamaguchi's criteria being the most used; 5 criteria are required, with at least 2 in adults:
- -
Main criteria: fever of at least 39°C over 7 days, joint pain or arthritis of more than 2 weeks, rash, and leukocytosis (≥10000/mm3) with at least 80% neutrophils.
- -
Minor criteria: sore throat, lymphadenopathy, hepato/splenomegaly, liver dysfunction (primarily AST, ALT and LDH), negative ANA and rheumatoid factor. It is necessary to exclude infections, lymphoproliferative or granulomatous disease.
At the start of treatment,10 oral or intravenous steroids are used if the situation is serious. Subsequently, immunosuppressants, mainly methotrexate, may be associated to control the disease and reduce the dose of corticosteroids. If no response is seen, biological therapies may be administered.
ConclusionsASD is a multisystemic inflammatory disease of unknown etiology. Its initial presentation with pleural and myopericardial manifestations is uncommon.
Please, cite this article as: García-García G, et al. Miopericarditis aguda como presentación de enfermedad de Still del adulto. Reumatol Clin. 2012;8(1):31–33.