During the 1960s, Levamisole was used as an anthelmintic agent. It was subsequently found to have immunomodulatory effects and was used to treat several inflammatory disorders. During the last decade, attention has been focused on the use of levamisole as a cutting agent for cocaine and on several cases of severe agranulocytosis associated with cocaine use.1
Cocaine/levamisole-induced vasculitis – LIVEN – is a heterogeneous vasculopathy characterized by skin necrosis concentrated in acral areas [ears, cheeks, genitals and digital necrosis], retiform purpura, general symptoms and cytopenias.2 Histopathological samples reveal pauci-inflammatory thrombotic diathesis accompanied with intravascular monocytes and evidence of complement activation.3
In 23 consecutive patients with systemic vasculitis from Hospital Universitario San Vicente Fundación, Medellín, Colombia, we analyzed the presence of Anti C1q antibodies, including antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, (N=13), polyarteritis nodosa (N=4), LIVEN (N=4) and Takayasu arteritis (N=2). Serum Anti-C1q were measured by ELISA techniques (QUANTA Lite, Inova, USA). This study was approved by the institutional review board at our institution.
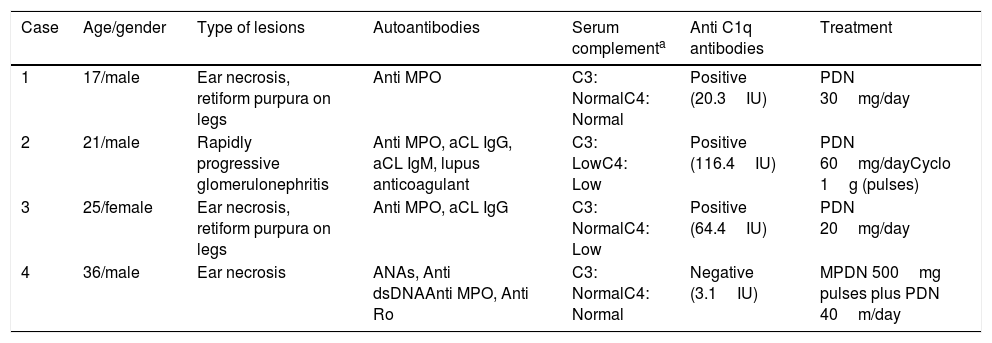
From this small pilot study, we found that anti C1q antibodies were more prevalent in LIVEN patients in comparison with other vasculitis (75% vs. 5.3%, p<0.001). Mean anti C1q titers were significantly higher in patients with LIVEN than in other vasculitis (51.0±25.3 vs. 10.4±7.1IU, p=0.04). Main clinical and serological characteristics including serum complement levels are summarized in Table 1.
Clinical and serological characteristics of LIVEN patients.
| Case | Age/gender | Type of lesions | Autoantibodies | Serum complementa | Anti C1q antibodies | Treatment |
|---|---|---|---|---|---|---|
| 1 | 17/male | Ear necrosis, retiform purpura on legs | Anti MPO | C3: NormalC4: Normal | Positive (20.3IU) | PDN 30mg/day |
| 2 | 21/male | Rapidly progressive glomerulonephritis | Anti MPO, aCL IgG, aCL IgM, lupus anticoagulant | C3: LowC4: Low | Positive (116.4IU) | PDN 60mg/dayCyclo 1g (pulses) |
| 3 | 25/female | Ear necrosis, retiform purpura on legs | Anti MPO, aCL IgG | C3: NormalC4: Low | Positive (64.4IU) | PDN 20mg/day |
| 4 | 36/male | Ear necrosis | ANAs, Anti dsDNAAnti MPO, Anti Ro | C3: NormalC4: Normal | Negative (3.1IU) | MPDN 500mg pulses plus PDN 40m/day |
Cyclo: cyclophosphamide, PDN: prednisolone, MPDN: methylprednisolone.
It is well known that levamisole induces circulating autoantibodies. Patients commonly have high levels of perinuclear ANCA (p-ANCA) but not always against myeloperoxidase (MPO). p-ANCA titers are often directed against atypical p-ANCA-associated antigens within the neutrophil granules such as: human neutrophil elastase, lactoferrin, and cathepsin G.4
Recently, our group described a series of 11 patients with LIVEN.5 ANCA (91%), lupus anticoagulant (73%), ANAS (45%), anti dsDNA (29%), anti Ro (29%) were most common autoantibodies.5 Given the social difficulties for clinical follow-up in cocaine users, anti C1q antibodies are not measured yet in all patients with LIVEN attending our center.
Anti C1q antibodies have been described in many conditions including hypocomplementic urticarial vasculitis, systemic lupus erythematosus and membranoproliferative glomerulonephritis, among others. To our knowledge, this study is the first on anti C1q antibodies in patients suffering LIVEN.
C1q is a molecule important for the clearance of apoptotic cells. Apoptotic cells express autoantigens in their surface and may induce autoimmunity. Cocaine/levamisole generates repeated release of neutrophil antigens that might act as autoantigens and leads to decreasing tolerance. Neutrophils secrete complement proteins upon activation with PMA, fMLP and C5a. Neutrophil extracellular traps (NETs) have been implied as a potential source of autoantigens.6 Leffler et al.7 demonstrated that in vitro complement interaction with NETs and that C1q bound well and C3b deposited on NETs. The authors argue that decreased degradation of NETs led to deposition of complement and autoantibodies, recruitment of more complement, perpetuating the inflammatory cycle.
Finally, metabolic products of cocaine promote complement synthesis and lead to the deposition of C5b-9. LIVEN is proposed as a membrane attack complex (C5b-9) disease with enhanced apoptosis and prominent vascular expression of ICAM-1.3
Increasing reports signal that LIVEN is a contemporary public health problem. Recent reports from different authorities in the U.S. and the U.K. suggest that cocaine samples are contaminated with levamisole in 50–80% of cases.8 According to local authorities in Colombia, levamisole contaminates 40% of the market.9 Indeed, preventing cocaine use is crucial for mitigating additional cases of LIVEN. Despite awareness of its toxicity by clinicians, identifying new biomarkers is necessary for practitioners that interface with these patients. Given our small sample size, further research is needed to confirm our findings that suggest anti C1q antibodies are useful markers in patients with LIVEN.
Conflict of interestThe authors declare no conflict of interest.
J.A. Gómez-Puerta was supported by Colciencias (convocatoria 656 de 2014). We would like to thank Catalina Perez Koller and Liliana Marcela Peñaranda (Inova/Wefen) for assisting with sample management and analysis of antibodies.