To identify the main problems affecting general practitioners (GPs) and specialists in the care of the main musculoskeletal problems in Catalonia.
MethodCross-sectional, self-administered survey in a representative sample of GPs and all specialists in four areas (orthopedic surgery, rheumatology, physical medicine and rehabilitation and pain units). Variables evaluated in the survey were related to socio-demographic data, attention to musculoskeletal diseases, self-declared expertise, referral process, coordination mechanisms and major constraints to provide high quality care.
ResultsGPs value well their expertise in the management of musculoskeletal diseases (6.7±1.0 on a scale of 1–10). Less than 25% of GPs are coordinated with hospital specialists. For them, waiting lists are the main problem (8.2±1.6/10) followed by lack of feedback (8±1.9/10) and poor coordination (7.8±1.9/10). Referenced specialties should change for some diseases (back pain and osteoarthritis). Specialists are critical for GPs. For specialists, the main problems are excessive workload (7.8±2/10) and the inefficiency of healthcare information systems (7.4±2/10).
ConclusionsThe vision of the problems affecting the care of musculoskeletal diseases differs between GPs and hospital specialists. The limited accessibility and workload excess, deficiencies in the flow of information and poor coordination are the most important problems in the proper care for musculoskeletal diseases.
Detectar los principales problemas que afectan a los médicos de familia (MF) y a los especialistas hospitalarios, en la atención de las principales enfermedades del aparato locomotor en Cataluña.
MétodoEstudio descriptivo transversal realizado mediante una encuesta auto-administrada dirigida a MF y a especialistas hospitalarios de 4 ámbitos (cirugía ortopédica y traumatología [COT], reumatología [RMT], medicina física y rehabilitación [MFR] y unidades del dolor [UD]). Las variables recogidas evalúan datos socio-demográficos, dedicación asistencial, destreza autodeclarada, el proceso de derivación, los mecanismos de coordinación y las principales dificultades para ofrecer una atención de calidad.
ResultadosLos MF consideran bueno su nivel de destreza en el manejo de las enfermedades del aparato locomotor (6,7±1,0 en una escala del 1 al 10). Menos del 25% refieren coordinarse con especialistas hospitalarios. Para los MF el mayor problema son las listas de espera en las especialidades citadas (8,2±1,6/10), seguido de la falta de información de retorno (8±1,9/10) y de la escasa coordinación (7,8±1,9/10). Según su criterio, la especialidad de referencia debería cambiar en algunas patologías (como la lumbalgia y la artrosis). Los especialistas hospitalarios son críticos respecto al papel de los MF. Para ellos, los principales problemas son la propia sobrecarga asistencial (7,8±2/10) y la ineficiencia de los sistemas de información (7,4±2/10).
ConclusionesLa opinión sobre los problemas que afectan a la atención de las enfermedades del aparato locomotor difiere entre los MF y los especialistas hospitalarios. La falta de accesibilidad y la sobrecarga asistencial de la atención especializada, las deficiencias en el flujo de información y la escasa coordinación son los problemas más destacados.
Musculoskeletal diseases are the most common chronic problems in the adult European population.1 In Spain, the EPISER 20002 study showed that 44.8% of the population has suffered from back pain in the past 6 months, 10.2% suffers from knee osteoarthritis, 6.2% of hand osteoarthritis, 3.4% osteoporosis, 2.4% fibromyalgia and 0.5% rheumatoid arthritis. According to the Health Survey of Catalonia 2006,3 musculoskeletal disorders are the most prevalent chronic problems associated to a poor perception of health and a high consumption of health resources, and are the leading cause of functional restriction.4 Rheumatic processes are also a common cause of disability.5
The Spanish public health system has as its main feature a strong presence in primary care (PCP), which usually acts as a gateway to specialist care (SC), mostly in hospitals. The main problems in the functioning of the system are the burden of care, waiting lists and lack of coordination between the PC and SC.6 The PC level receives more inquiries regarding locomotor7 pathologies which are expected to increase with the aging of the population. These processes are usually derived to 4 specialties: orthopedic surgery and trauma (TOS), rheumatology (RMT), physical medicine and rehabilitation (PMR) and pain units (PUs). However, the poor implementation of clinical practice guidelines on musculoskeletal care problems, poor definition of the interconsultation criteria, and the lack of coordination between levels and causes specialty mismatches in referral to SC.8,9 It has also been postulated that the lack of training in these diseases received by PC has a negative effect on the appropriateness of referrals to SC.10
The “European Parliament declaration on rheumatic diseases” urges governments to promote plans to improve care and research on them, with the goal of reducing associated economic and social costs.11 To this end, the Department of Health of the Generalitat of Catalonia designed the Master Plan for Rheumatic Diseases and Locomotor Apparatus.12,13 In this context, and as an aid to planning, it was considered useful to have the views of professionals on different aspects related to musculoskeletal diseases and their care process by designing a survey of medical professionals. The objective of this paper is to describe, from the results of this survey, the professionals’ opinions on the major problems perceived in the care of these diseases.
MethodologyStudy design: Descriptive study based on a survey designed by the authors (available upon request), one of whom (LB) is a sociologist and an expert in questionnaire design. The survey was overseen and approved by the Department of Health of the Generalitat de Catalunya. There were 9 versions of the survey prior to the final version. There was a pre-test validation process with 3 professionals who self-administered the questionnaire and collected comments. The first 80 questionnaires (40 specialists and 40 primary) underwent a pilot test for undetected problems in understanding or interuser agreement, inconsistencies or accumulation of negative answers.
Sample and data collection: 2 questionnaires were sent, one to GPs and another to hospital specialists. We previously conducted a random sampling of primary care centers, selecting 114 (102 publicly owned and 12 privately run) of 362 existing centers where a total of 1250 PC physicians work. In addition, the questionnaire was sent to 61 specialist hospitals of the Catalan public network, in which 1036 specialists work (645 TOS, RMT 138, 123 and 130 PRM). Questionnaires were sent to the professionals’ workplace, who were able to answer on paper or electronically. The information was collected between June and December 2009 and a specific database was created. Participation was voluntary and with the survey an explanatory letter was sent about the study objectives and the commitment to maintain confidentiality.
Variables: The 2 questionnaires were common and had some specific points. Sociodemographic data and clinical activity. The diseases studied were peripheral joint osteoarthritis, back pain, osteoporosis, tendonitis, fibromyalgia and arthritis, inflammatory rheumatism, as well as sprains and bruises. Questions were made on the allocation of care (proportion of time devoted to musculoskeletal pathology) and order of frequency of the 7 diseases analyzed (scoring from 1 to 7 for each disease based on their high to low presence in the query), the self-reported skill level, the referral process, the existence of mechanisms for coordination and evaluation of a series of 15 problems described in the literature or selected by experts. Table 1 shows the survey questions and the scale of measurement of the different variables.
Comparative Variables Obtained in 2 Surveys.
| Question | Response Scale | Response Possibilities |
| 1. Sociodemographic data of professionals | • Age and gender• Years of experience• Workplace• Years in the workplace | |
| 2. Assistance dedication | ||
| Time dedicated to locomotor system problems | • % of time for each visit | |
| Order of frequency of visits for each of the 7 most common diseases of the locomotor system | 1=more frequent7=less frequent | • Peripheral osteoarthritis• Back pain• Fibromyalgia• Osteoporosis• Tendinitis (painful shoulder/soft tissue rheumatism)• Arthritis/inflammatory rheumatism• Bruises/sprains |
| 3. Self declared competency | ||
| Problem attention skill level | 1=no skill10=expert | |
| 4. Referral process | ||
| Frequency of referral of these problemsa | 1=exceptionally derives2=derives seldom3=frequently derives4=always or almost always derives | |
| PCP have clear referral criteria for different specialties | 1=generally yes2=only in some cases3=generally no | • Rheumatology (RMT)• Trauma and orthopedic surgery (TOS)• Physical medicine and rehabilitation (PMR)• Pain unit (PU) |
| Specialty to which the physicians believe the locomotor system disease case should be referreda | ||
| Specialty that should act as a referral for the diseases cited among the 4 medical specialties related to the locomotor systemb | ||
| 5. Coordination level | ||
| Evaluation of the coordination level with PCPb | 1=little or none, 10=a lotb | |
| Coordination with specialistsa | Yes/noa | |
| Existence and types of coordination mechanisms between PCP and specialists | Yes/no | • Programmed visits• Shared visits with patients• Agreed upon criteria for referral• Direct open line system• Common protocols• Formation sessions |
| 6. Problems related to care | ||
| Opinion on aspects of attention to musculoskeletal problems in PCPb | 1=little or none10=a lot | • Appropriate formation of the PCP in musculoskeletal problems• Resolution capacity of PCP• Contention capacity of PCP• Adequate information in referrals• Adequate referral to specialized care level• Adequate referral to specialized care |
| Evaluation of different problems related to care | 1=does not impede care10=impedes care a lot | • Specialist waiting list• Little definition in the services provided by each specialtya/Little definition in the function of each specialtyb• Retention of patients on the part of the specialtya• Little coordination with specialistsa• Little coordination between specilists• Assistance burden in primary care• Assistance burden in specialist careb• Assistance burden of other specialists concerned with the locomotor systemb• Little information for PCPa• Little access of PCP to diagnostic testsa/Waiting list for diagnostic testsb• Contrareferral of patients without informationa• Inefficient feedback loops• Limited access to podologya• Limited access to physiotherapya |
Statistical analysis: The margin of error for the survey was obtained by applying the calculation for finite samples (less than 100000 subjects) for a confidence level of 95.5% with p=q=0.5 (statistically the worst outcome); a descriptive analysis was performed using measures of central tendency and dispersion for quantitative variables and distribution of percentages for qualitative variables.
ResultsSociodemographic and ParticipationResponses were received from 233 PCP and 446 specialists (240 TOS, 86 RMT, 74 PRM, 46 PU). The response rate of the survey for PCP was low (18.6%, margin of error±6.5%) and highest for specialists (43%±3.7%) but variable depending on the specialty: TOS (37.2%±5.2%), RMT (62.3%±7.8%), PRM (60.2%±7.8%) and PU (35.4%±12.9%). Among GPs, the majority of respondents were female (66.4%) with a mean age of 44.7%±8.6 years. The mean duration of practice was 16±9.1 years with a mean of 9.8±8.4 years old in the workplace. The selected primary care centers are distributed in 29 regions of Catalonia, and were a total of 41, with a greater presence in Barcelona and its metropolitan area (17.1% and 42.6% respectively, compared to 39.6% in the rest of Catalonia). Regarding specialists, the gender and age distribution was heterogeneous according to the specialty. The RMT and PMR specialties are feminized and young, where more than half the sample were women and had an average age of 44.8±9.6 and 43.6±8.4 years, respectively. TOS is less feminized with 15% female and a mean age of 48.6±9.2 years. There is an increased presence of professionals who have their workplace in Barcelona and its metropolitan area (29.8% and 34.1% respectively) compared to 36.1% in the rest of Catalonia, following the population distribution. Their mean time of practice and seniority in the workplace was somewhat higher than GPs (18.1±10.1 and 12.5±9.8 years respectively).
Dedication care: GPs reported spending one-third (32.5%) of their time caring for musculoskeletal diseases compared to an average of 81.6% of the time of the 4 specialty hospitals, with differences between TOS and RMT (90.8% and 86.2% respectively), and between PMR (60.8%) and PU (43.2%). Among the pathologies of the musculoskeletal system, back pain and osteoarthritis were the first 2 reasons for visiting PCP and specialists both, except in the case of PMR, with tendinitis the second most common ahead of osteoarthritis (Table 2). Inflammatory arthritis, rheumatism, fibromyalgia and osteoporosis were less frequent and present only prominently in RMT clinics (31%, 30.1%, and 22.9% of the rheumatologists surveyed first or second in order of frequency in the questionnaire, respectively) and in the case of fibromyalgia in the PU (20.5% of specialists of the PU placed it first or second).
Most Common Diseases Seen by PCP and Specialists (%) and Level of Self-declared Skills (in Bold) vs the Different Diseases (Mean Score 1–10±Standard Deviation). Percentage of Cases of the Different Pathologies Derived From PCP to Specialized Care (%).
| Visit Frequency* | Percentage of PCP Who Always or Frequently Refer to Specialized Care, % | |||||
| Level of Self-declared Skill (Mean Score in a Scale of 1–10±Standard Deviation) | ||||||
| PCP | Hospital Specialists | |||||
| TOS | RMT | PMR | PU | |||
| Peripheral osteoarthritis | 61.3% | 69.1% | 45.8% | 26.0% | 58.1% | 4.3% |
| 7.1±1.5 | 8.7±1.4 | 8.6±1.2 | 8.5±1.0 | 6.7±2.0 | ||
| Back pain | 69.1% | 58.6% | 44.7% | 79.5% | 93.2% | 10% |
| 7.4±1.3 | 7.7±1.9 | 8.3±1.3 | 8.6±1.1 | 8.5±1.1 | ||
| Tendinitis | 23.9% | 22.9% | 17.6% | 71.2% | 7.0% | 34% |
| 6.8±1.4 | 8.4±1.5 | 8.3±1.3 | 8.6±1.1 | 5.9±1.8 | ||
| Bruises/sprains | 12.2% | 21.7% | 6.1% | 9.6% | 7.1% | 10% |
| 7.2±1.4 | 8.9±1.3 | 4.1±2.7 | 8.5±1.1 | 4.5±1.8 | ||
| Osteoporosis | 2.7% | 8.8% | 22.4% | 6.8% | 7.0% | 14% |
| 6.9±1.5 | 6.1±2.3 | 8.9±1.1 | 7.0±1.7 | 6.2±1.6 | ||
| Rheumatism-Arthritis | 5.4% | 11.2% | 30.2% | 4.1% | 4.7% | 81% |
| 5.7±1.5 | 5.9±2.3 | 9.0±1.1 | 6.4±1.5 | 5.0±1.6 | ||
| Fibromyalgia | 6.8% | 9.3% | 29.4% | 2.7% | 20.5% | 47% |
| 5.6±1.6 | 3.8±2.2 | 7.3±2.1 | 5.9±2.3 | 7.0±2.0 | ||
TOS, trauma and orthopedic surgery; PCP, primary care physicians; PMR, physical medicine and rehabilitation; RMT, rheumatology; PU, pain unit.
Self-reported skill: Self-reported levels stood at 7.2±1.2, averaged over 10 in the 4 specialties and 6.7±1 in the PCP, with the top scores for those pathologies treated (Table 2).
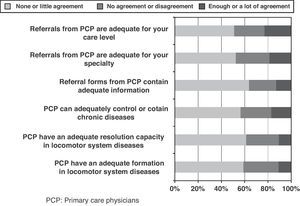
Process of referral: GPs referral to SC varies according to each pathology. The most extreme situations occur in osteoarthritis which was identified in only 4.3% of the total of 233 PCP, and were confused with arthritis, inflammatory rheumatism in 81% (Table 2). GPs were clear on which cases should be referred to TOS and RMT (92% and 89% of professionals, respectively) but showed more doubts on what cases to refer to PMR (35.2% doubt), and a greater proportion to PU, where 45.6% were not clear on which cases to refer. Conversely, many experts believe that the PCP did not have clear criteria for referral to specialty (41.6% TOS, 33.3% RMT, 22.9% PMR, 29.5% PU); in addition, 56.5% of GPs believed that they had little capacity to contain these diseases, and that referrals to hospitals or any particular specialty are inadequate (51% and 52.5%, respectively). Also, SC considered that the information provided in the referral sheet was not enough (63.8%) and GPs had insufficient specific training on musculoskeletal disorders (59%) (Fig. 1).
Table 3 shows the results on the fate of the cases: the specialty to which the patient was derived from PCP and their opinion, as well as the various specialists, the specialty that should be the benchmark in each case (provided there is no clear indication for surgery). Regarding osteoarthritis and back pain, GPs derived about half of cases (50.2% and 53.1%, respectively) to TOS while in their opinion, which coincides with the average of the experts, this percentage should be reduced by half (25.8% in osteoarthritis and 26.9% in back pain) and should increase the proportion of osteoarthritis and back pain cases referred from RMT to MFR. On the contrary, it was considered unanimously that rheumatology is and has to be the benchmark for inflammatory rheumatism, osteoporosis and fibromyalgia, while sprains and bruises are addressed and should be treated in TOS.
Specialty to Which the Case is Referred: Specialty to Which Primary Care Physicians Refer (Bold) and Specialty to Which They Should be Referred in Referral to Different Locomotor System Disease; According to the Primary Care Physicians and the Different Specialists (Results in % on the Total of Both Surveyed Samples).
| TOS | RMT | PMR | PU | |
| Peripheral osteoarthritis | ||||
| Where does the PCP derive? | 50.2 | 19.3 | 30.5 | 0 |
| Where should the case be referred? | ||||
| According to PCP | 25.8 | 36.4 | 29.3 | 8.4 |
| According to the specialist | 31.1 | 48.6 | 19.8 | 0.6 |
| Back pain | ||||
| Where does the PCP derive? | 53.1 | 4.9 | 39.7 | 2.2 |
| Where should the case be referred? | ||||
| According to PCP | 26.9 | 18.1 | 48.9 | 6.2 |
| According to the specialist | 21 | 28.7 | 42.5 | 7.80 |
| Fibromyalgia | ||||
| Where does the PCP derive? | 0.9 | 87.4 | 1.8 | 9.9 |
| Where should the case be referred? | ||||
| According to PCP | 0 | 65.6 | 8.4 | 26.0 |
| According to the specialist | 0 | 83.2 | 2.0 | 14.8 |
| Osteoporosis | ||||
| Where does the PCP derive? | 12.0 | 84.9 | 3.1 | 0 |
| Where should the case be referred? | ||||
| According to PCP | 8.4 | 87.6 | 3.1 | 0.9 |
| According to the specialist | 5.4 | 89.8 | 2.9 | 1.8 |
| Tendinitis | ||||
| Where does the PCP derive? | 51.5 | 15.9 | 32.6 | 0 |
| Where should the case be referred? | ||||
| According to PCP | 40.5 | 19.8 | 39.6 | 0 |
| According to the specialist | 35.6 | 24.3 | 39.8 | 0 |
| Bruises-Sprains | ||||
| Where does the PCP derive? | 88.6 | 0.0 | 11.4 | 0 |
| Where should the case be referred? | ||||
| According to PCP | 78.9 | 1.3 | 19.8 | 0 |
| According to the specialist | 89.1 | 0.4 | 10.3 | 0.3 |
| Arthritis-rheumatism | ||||
| Where does the PCP derive? | 1.3 | 97.8 | 0.9 | 0 |
| Where should the case be referred? | ||||
| According to PCP | 0.4 | 97.4 | 1.3 | 0.9 |
| According to the specialist | 1.3 | 98.2 | 0.4 | 0 |
TOS, trauma and orthopedic surgery; PCP, primary care physicians; PMR, physical medicine and rehabilitation; RMT, rheumatology; PU, pain unit.
Looking at one's opinion of the hospital specialties was different (data not shown), in the case of TOS, as well as RMT and PMR regarding the role in diseases such as arthritis, tendinitis and back pain.
Existence and types of coordination mechanisms: 38% of GPs mentioned they had some kind of coordination with rheumatologists, 21% with TOS and PMR and only 5% with PU. On a scale of 1–10, only rheumatologists mentioned coordination with PCP (5.4±2.1/10). Among specialists, only 20% considered that there was good coordination with the GP. The coordination mechanisms most frequently used were the agreements on referral criteria and open line systems, although little more than 25% of respondents routinely referred them when available. Other mechanisms such as more intensive face to face consulting, joint visits, training sessions or the use of common protocols are less used (<11% of cases have a usual coordination system).
Assessment of attention-related problems: Table 4 shows the evaluation of PC professionals and experts on various issues which may affect the proper care for musculoskeletal diseases. The main obstacles to the PCP are the waiting list in SC (8.2±1.6/10), the contrareferral of patients without sufficient information (7.9±1.9/10) and low coordination with specialists and between them (7.8±1.9/10). The problems arising from the burden of care itself were remarkable, and scored lower (7.6±1.9/10). Experts scored as most important issues such as their own burden of care (7.8±1.9/10) and the low efficiency of feedback loops (7.4±1.9/10), above waiting lists and coordination problems with other hospital specialties.
Evaluation of the Different Problems That may Affect the Attention to Locomotor System Diseases, According to PCP and Specialists (Mean Score on a Scale of 1–10±Standard Deviation). The Last Column Expresses the Mean Between the Specialist Sample (in Bold the Highest 4 Scores of Both Samples is Expressed).
| PCP Opinion | Problems That may Affect the Attention of Locomotor System Diseases | Specialist Opinion | ||||
| TOS | RMT | PMR | PU | Mean Specialists | ||
| 8.2±1.6 | Specialty waiting list | 7.4±2.4 | 6.6±2.1 | 6.8±2.1 | 7.5±1.8 | 7.1±2.3 |
| 7.9±1.9 | Contrareferral of patients to PCP with insufficient information | – | – | – | – | – |
| 7.8±1.9 | Little coordination with specialists | – | – | – | – | – |
| 7.8±1.8 | Little coordination among specialists | 6.7±2.2 | 6.9±1.9 | 7.0±1.8 | 7.4±1.7 | 6.9±2.0 |
| 7.6±1.9 | Care burden of PCP | 6.6±2.3 | 7.0±1.8 | 6.4±2.3 | 7.0±1.6 | 6.7±2.2 |
| – | Self burden of care | 8.2±1.7 | 7.2±2.2 | 7.1±2.2 | 7.6±1.5 | 7.8±1.9 |
| – | Burden of care of the rest of the specialties | 7.3±2.0 | 7.2±1.6 | 7.0±1.7 | 7.5±1.5 | 7.2±1.8 |
| 7.0±2.5 | Limited access to podology | – | – | – | – | – |
| 6.8±2.0 | Inefficient feedback loops | 7.3±2.0 | 7.4±1.9 | 7.6±1.7 | 7.8±1.7 | 7.4±1.9 |
| 6.6±2.3 | Limited access to physical therapy | – | – | – | – | – |
| 6.3±2.1 | Little definition in the function of each specialist | 6.7±2.1 | 6.4±2.3 | 5.9±2.6 | 7.0±2.1 | 6.5±2.3 |
| 6.0±1.9 | Lack of PCP formation | – | – | – | – | – |
| 5.6±2.4 | Retention of patients on the part of the specialist | – | – | – | – | – |
| 5.6±2.5 | Limited PCP access to diagnostic tests | – | – | – | – | – |
| – | Diagnostic test waiting list | 7.1±2.1 | 6.7±2.1 | 7.1±1.9 | 6.6±2.2 | 7.0±2.1 |
TOS, trauma and orthopedic surgery; PCP, primary care physicians; PMR, physical medicine and rehabilitation; RMT, rheumatology; PU, pain unit.
The PCP respondents spend nearly a third of their time treating diseases of the musculoskeletal system. This figure puts the relative weight of this group of disorders on primary care over something known in other countries.14,15 Also in SC, the time devoted to the care of musculoskeletal diseases is significant, even in specialties or cross disciplines as PMR and PU. The skill level declared by the PCP for each condition was better for the more frequent processes in daily practice, and these were also the least common processes referred to specialists. The case of fibromyalgia would be an exception, as it is perceived as a rare condition in consultation with AP, with lower levels of skill and greater percentage of referrals. This is in line with the results of a survey of primary care physicians performed in Great Britain.8
There are different perceptions by GPs and hospital specialists regarding the management of musculoskeletal diseases, starting with the review of the adequacy of the referral. While the PCP was concerned with the problems that deserved to be referred to these specialties, especially RMT and TOS, experts believed that there was inadequacy in the referral to hospitals and specialties. Consistent with the latter, PCP themselves recognize that they derive the majority of cases of back pain, tendinitis, sprains, bruises, and arthritis to TOS but they had less success in non-traumatic pathologies, where the proposal is to increase the referrals to other specialties such as rheumatology (especially in the case of osteoarthritis). In the same vein, some scholars claim that TOS also openly assumes a more specific reference to the surgical unit.16 This excess referral toward the orthopedic specialist also has been described in other countries.9
GPs referral derives a small percentage of the most prevalent diseases; however, experts perceive this rate as excessive, attributing it to a lack of resolution capability, containment and inadequate specific training. Although the “ideal” referral rate is not set, it seems clear that this is valued differently in the 2 health care settings. From the perspective of PCP, the very high morbidity of these processes, their chronic nature, the burden of care and the willingness of patients to obtain a specialized assessment are factors that probably influence the rate of referral to SC. On the other hand, it is clear that more training or some specific professional dedication for PCP in an area of knowledge reduce referral to the corresponding specialized level.17 Mismatched referral to different specialties may be related to their historical development in the health care in our country (with a clear predominance of TOS), the lack of definition of the burden of each specialty and the deficiency in the mechanisms for coordination. Finally, there is a lack of satisfaction with the transfer of information between levels, making it difficult to prioritize patients in SC18 and insure continuity of care.
For the PCP, the main problem in the management of these diseases is the SC waiting list, a widespread problem in western health systems.19,20 As a second problem, the lack of feedback from the hospitals is highlighted. From the standpoint of the specialist, its own burden of care is followed by inefficient information systems that are the elements that determine the quality of care. Note that in Catalonia there are different PCP service providers and hospitals, many of which are publicly owned and do not share their information systems. The current development of Shared Medical History of Catalonia as a tool for interoperability of information systems will improve access to all information professionals regarding patients.21
A limitation of our study is the low rate of responses from GPs despite repeated contacts with heads of departments requesting their participation. This was probably influenced by the time of year the questionnaires were sent, which coincided with the holiday season and the alarm generated by the first influenza A epidemic. Moreover, the data referred on the prevalence of each disease in the clinic and referral to a specialty were based exclusively on the opinion of the physician and have been compared with objective referral data and activity logs. However, the qualitative data presented, taking into account these limitations, sheds some light on the opinions and practice. We should also mention the different response rates of the participating specialties. Among these specialties, the most numerous in Catalonia, the orthopedic surgeons, represent more than half of all respondents. Still, except in very specific issues, their opinion does not differ greatly between the 4 specialties and is representative of the views of specialists dedicated to the musculoskeletal system of our public health system.
In conclusion, the waiting lists for SC as well as gaps in the information systems sharing and coordination mechanisms are the elements of greatest concern to the professionals who care for musculoskeletal diseases. The marked discrepancy in the perception of GPs and specialists in some ways reflects the existence of deficits in the definition and organization of health services involved in the care of chronic musculoskeletal problems.
FinancingDepartment of Health, Generalitat de Cataluña, Spain.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Surís X, et al. Atención a las enfermedades músculo-esqueléticas: distintas visiones del mismo problema. Reumatol Clin. 2013;9:31–37.