Calf pseudohypertrophy due to radiculopathy is an exceptional phenomenon rarely described. We report a 67 year old woman with a previous history of lumbar disc surgery consulting by progressive increase for more than a year of evolution painless right calf associated loss of strength. Electromyographic findings showed chronic S1 radiculopathy and radiologically was appreciated in the medial gastrocnemius and soleus rights substitution of normal muscle tissue by adipose tissue without evidence of myopathy or sarcomatous degeneration.
La pseudohipertrofia gemelar secundaria a una radiculopatía es un fenómeno excepcional raramente descrito. Presentamos el caso de una mujer de 67años con antecedentes de cirugía discal lumbar que consultaba por aumento progresivo de más de un año de evolución, no doloroso, de la región gemelar derecha con ligera pérdida de fuerza asociada. Los hallazgos electromiográficos evidenciaron una radiculopatía crónica S1 y radiológicamente se apreciaba, en territorio del gastrocnemio medial y sóleo derechos, una sustitución del tejido muscular normal por tejido adiposo, sin evidencia de miopatía o degeneración sarcomatosa.
An increase in the volume of an anatomical region is not a common reason for being sent to a rheumatology department. We report the case of a patient with a progressive increase in the circumference of her right leg. She was referred to us to rule out a possible rheumatic disease.
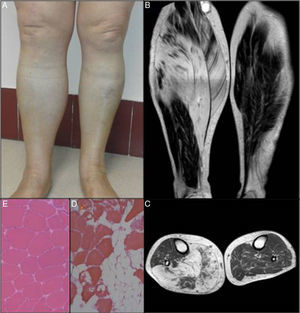
Case ReportThe patient was a 67-year-old woman who, in January 2012, was sent from general surgery to be studied for a possible myopathy. She had a history of non-insulin-dependent diabetes mellitus and chronic low back pain secondary to disc herniation surgery at lumbar 5–sacral 1 (L5–S1) more than 30 years ago. She had the feeling that the thickness of her right calf had been increasing progressively for more than a year, and associated it with a more significant gradual weakening in recent months. The physical examination found no evidence of connective tissue disease. She had negative results on sciatic tests and a painless increase in the circumference of right calf region (45cm) with respect to the left side (39cm). She found it difficult to maintain her right foot in a tiptoe posture and right Achilles reflex was abolished (Fig. 1A). We also performed an analytical study, both general (complete blood count, laboratory findings including liver function, creatine phosphokinase, aldolase, erythrocyte sedimentation rate and C-reactive protein) and immunological (rheumatoid factor, anti-cyclic citrullinated peptide antibodies, antinuclear antibodies, extractable nuclear antigen autoantibodies and antineutrophil cytoplasmic antibodies), with normal results. An electromyogram of lower limbs showed severe chronic neurogenic changes in right S1 myotome. There were no signs of active denervation, and magnetic resonance imaging (MRI) of the lower limbs revealed marked atrophy of medial gastrocnemius and soleus muscle and partial atrophy of the lateral gastrocnemius muscle. The latter were nearly totally replaced and generated a diffuse signal, which appeared to behave with a signal similar to that of connective tissue fat in all the pulse sequences, compatible with areas of fat replacement (Fig. 1B and C). Muscle biopsy revealed no dystrophic changes, necrosis, regeneration or histological evidence of active denervation. There was a slight variability in the size of the fibers, and marked infiltration of adipose tissue and, less pronounced, of connective tissue in both the endomyseum and perimyseum (Fig. 1D). The study was completed with MRI of the lumbar spine, which showed degenerative discovertebral changes at L5–S1, with right foraminal stenosis and slight swelling of the root, probably secondary to radicular involvement. With no evidence of malignancy or of autoimmune or metabolic disease, and in the absence of symptoms implicating the sciatic nerve and of significant low back pain, we opted for a conservative approach. There have been no changes in the course of the follow-up of our patient to date.
DiscussionMuscle atrophy due to denervation is the most characteristic consequence of a lesion affecting a nerve structure or tissue. However, although much less frequently, there can be phenomena like muscle hypertrophy and pseudohypertrophy (replacement of muscle tissue by connective and fatty tissue) associated with different situations, such as post-polio syndrome, spinal muscle atrophy and polyneuropathies, like radiculopathies. With respect to the latter, most of the reported cases usually coincide with unilateral calf hypertrophy secondary to S1 radiculopathy; no reason is provided to explain why the territory of this nerve root is more susceptible to developing this rare disorder.1 Muscle pseudohypertrophy is a phenomenon classically related to hereditary muscular dystrophy and post-polio syndromes. Here it is exceptional in that it is associated with a radiculopathy, although some authors have advocated considering muscular hypertrophy and pseudohypertrophy as different stages of the same disease process, resulting from radicular injury. A review of the reported cases outlines quite a similar presentation: an increase in the circumference of the calf in patients with a history of lumbar disc disease, characterized as progressing slowly, and often painlessly, associated by limited debility, after tumor, bone and vascular diseases have been ruled out.2 Nevertheless, this phenomenon is so infrequent that authors are usually obliged to opt for a pathological diagnosis. The differential diagnosis should include hereditary myopathy, spinal muscle atrophy, hypothyroidism (Werdnig–Hoffman disease) and infiltrative diseases such as focal myositis, amyloidosis, parasites and tumors, especially sarcomas. The main cause of radiculopathy is degenerative disc and lumbar disease, and cases associated with intraspinal neurinoma3 and lipoma of the sacral roots,4 have also been reported. Stability or even an improvement in the prognosis of hypertrophy is usually achieved with a conservative or a surgical approach. The effect of disc decompression surgery seems to have a major influence on relieving pain and alleviating debility more than on the intent to revert the muscle hypertrophy, where the postoperative improvement may be less evident. There are therapeutic experiences with steroids, radiotherapy and botulinum toxin with modest results.5
ConclusionsMuscle pseudohypertrophy secondary to radiculopathy is an exceptional finding. Most of the few cases reported to date correspond to a true muscle hypertrophy secondary to S1 radiculopathy in the setting of a degenerative disc disease of the spine. This should be considered to avoid unnecessary tests, in which the benefit of the surgical approach should be assessed for each individual.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Zurita Prada PA, Faré García R, Urrego Laurín CL, Pérez Toledo R, Tabernero García C, Hernández Laín A. Pseudohipertrofia gemelar. Reumatol Clin. 2017;13:173–175.