Catastrophic antiphospholipid syndrome (CAPS) is a rare entity, approximately 600 cases have been reported around the world, and the prevalence in Mexico is unknown.
ObjectiveTo determine the estimated prevalence of CAPS in Mexico.
Material and methodsA literature search of isolated clinical cases or case series was conducted in diverse search engines, using the terms: "Catastrophic Antiphospholipid Syndrome" and "Mexico" in May 2022.
ResultsWe found a series of retrospective cases in autopsies that included 12 cases, two reports that included 2 cases each, and reports of 11 isolated clinical cases; these publications were generated between 2003 and 2020. In total, we collected data on 27 cases of CAPS, of which 16 correspond to primary antiphospholipid syndrome, 10 are associated with systemic lupus erythematosus, and 1 case corresponds to systemic sclerosis. The estimated prevalence rate in the Mexican population in 2022 is 2 cases per 10,000,000 inhabitants. The estimated mortality was 68% in this case series.
ConclusionCases of catastrophic antiphospholipid syndrome in Mexico are underreported; identifying them will help improve current diagnostic and therapeutic strategies used in the country, encouraging the implementation of triple therapy and, in refractory cases, the use of eculizumab, to reduce current mortality.
El síndrome antifosfolípido catastrófico (SAFC) es una entidad rara, se han reportado aproximadamente 600 casos en todo el mundo, se desconoce la prevalencia en México.
ObjetivoConocer la prevalencia estimada de SAFC en México.
Material y métodosSe realizó una búsqueda bibliográfica de casos clínicos aislados o series de casos en los diversos buscadores, utilizando los términos: SAFC y México en mayo de 2022.
ResultadosEncontramos una serie de casos retrospectivos en necropsias que incluyeron 12 casos, dos reportes que incluyeron 2 casos cada uno, y también se encontraron reportes de 11 casos clínicos aislados; estas publicaciones se generaron entre 2003 y 2020. En total, se tienen datos de 27 casos de SAFC, de los cuales 16 corresponden al síndrome antifosfolípido primario, 10 en asociación con lupus eritematoso sistémico y 1 caso de esclerosis sistémica. La tasa de prevalencia estimada en la población mexicana en 2022 es de 2 casos por cada 10.000.000 de habitantes. La mortalidad estimada fue del 68% en esta serie de casos.
ConclusiónLos casos de Síndrome Antifosfolípido Catastrófico en México están subreportados, sin embargo, identificarlos ayudará a mejorar las estrategias diagnósticas y terapéuticas que se utilizan actualmente en el país, incentivando la implementación de la triple terapia y, en casos refractarios, el uso de eculizumab, para reducir la mortalidad actual.
Since the first descriptions by Drs Asherson, Harris and Hughes in the mid-1980s, anticardiolipin antibodies attracted attention for their thrombotic potential; but it was not until the end of that decade that the characteristics of the syndrome attributed to these autoantibodies (antiphospholipid or Hughes syndrome) were defined, in addition to identifying it as a primary or secondary syndrome, the latter being associated with other autoimmune entities, mainly systemic lupus erythematosus.1–6
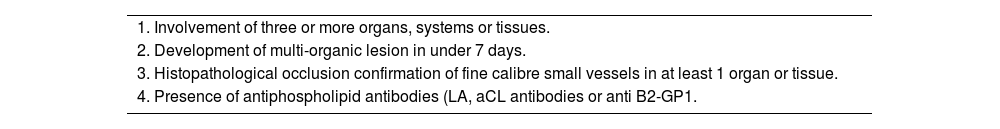
In the early 1990s, a systemic and hyperacute form of this syndrome that led to systemic or multi-organ thrombosis began to attract attention, which was called the catastrophic variety (CAPS) or Asherson's syndrome. Its pathophysiology was described at the beginning of 2000, in which the involvement of β2GP1 receptors was recognised as a proinflammatory, proadhesive and prothrombotic syndrome, and the classification criteria for CAPS were defined (Table 1); The catastrophic variety is considered a thrombotic storm with microvascular and macrovascular occlusions leading to multiple organ failure in a short period of time, with poor prognosis without timely medical attention; in this regard there are two pathophysiological processes occurring simultaneously: first, generalised thrombosis leading to multi-organ dysfunction and second, the subsequent inflammation produced by the lack of blood supply coupled with endothelitis and platelet and acute phase reactant activation, predominantly pro-inflammatory interleukins, which perpetuates the thrombotic process and leads to the multi-organ failure that characterises this catastrophic variety.7
Catastrophic Antiphospholipid Syndrome (CAPS) classification criteria.
| 1. Involvement of three or more organs, systems or tissues. |
| 2. Development of multi-organic lesion in under 7 days. |
| 3. Histopathological occlusion confirmation of fine calibre small vessels in at least 1 organ or tissue. |
| 4. Presence of antiphospholipid antibodies (LA, aCL antibodies or anti B2-GP1. |
*Definitive CAPS:
All four criteria met.
**Probable CAPS:
All 4 criteria met but involvement in only 2 organs, systems and/or tissues.
Four criteria, but without confirmation of lab tests until 6 weeks after the early death of the patient without previous APS tests.
Criteria 1, 2 and 4.
Criteria 1, 3 and 4, in addition to the development of a third posterior event after week 1, but before a month prior to beginning of symptoms, despite anticoagulant treatment.
AL, lupus anticoagulant; aCL, anticardiolipine; anti B2-GP1, anti-beta 2 glycoproteein 1.
In the same year, 2000, the international registry of cases of CAPS (CAPS Registry) was initiated by a Spanish medical group at the Hospital Clinic de Barcelona under the leadership of Dr. Ricard Cervera, who is currently leading the registry.8
One of the objectives of this initiative has been to reduce the high mortality observed in the first descriptions of this syndrome (the mortality rate was greater than 50%). A decrease in this rate has now been achieved, largely due to improvements in diagnosis and specific treatment, such that triple therapy (glucocorticoids, anticoagulation and intravenous immunoglobulin and/or plasmapheresis) is now recognised as the most beneficial in these cases and has reduced mortality by up to 28%. In recent years, in refractory cases (often associated with thrombotic microangiopathy with high activation of the complement system), eculizumab (a recombinant humanised IgG monoclonal antibody that inhibits terminal complement activation by binding to complement C5 protein) has been successfully used and complete remission rates have been observed in up to 74. 4% of these cases; other drugs used in refractory cases have been rituximab and cyclophosphamide but with lower success rates compared to eculizumab.9,10,11
Until December 2021, the international registry of cases of catastrophic antiphospholipid syndrome accumulated data of 584 cases worldwide, however, estimated figures at this time suggest approximately 600 cases (May 2022).10
The cases documented in the international registry from Mexico are approximately 4, but we consider that there may be an underreporting, therefore, there is doubt as to the true prevalence of cases in Mexico.
MethodsA bibliographic search of isolated clinical cases or case series was carried out in the search engines Web of Science, Pubmed, Scielo, Scopus, Publons, Google Scholar and Researchgate, using the terms: Catastrophic Antiphospholipid Syndrome and Mexico in May 2022, in both indexed and non-indexed journals. The diagnosis mentioned in the title of each publication was taken into consideration and it was corroborated that the clinical, laboratory and histopathological criteria for classification of the syndrome (Table 1) were met in order to classify them as definitive or probable catastrophic antiphospholipid syndrome.
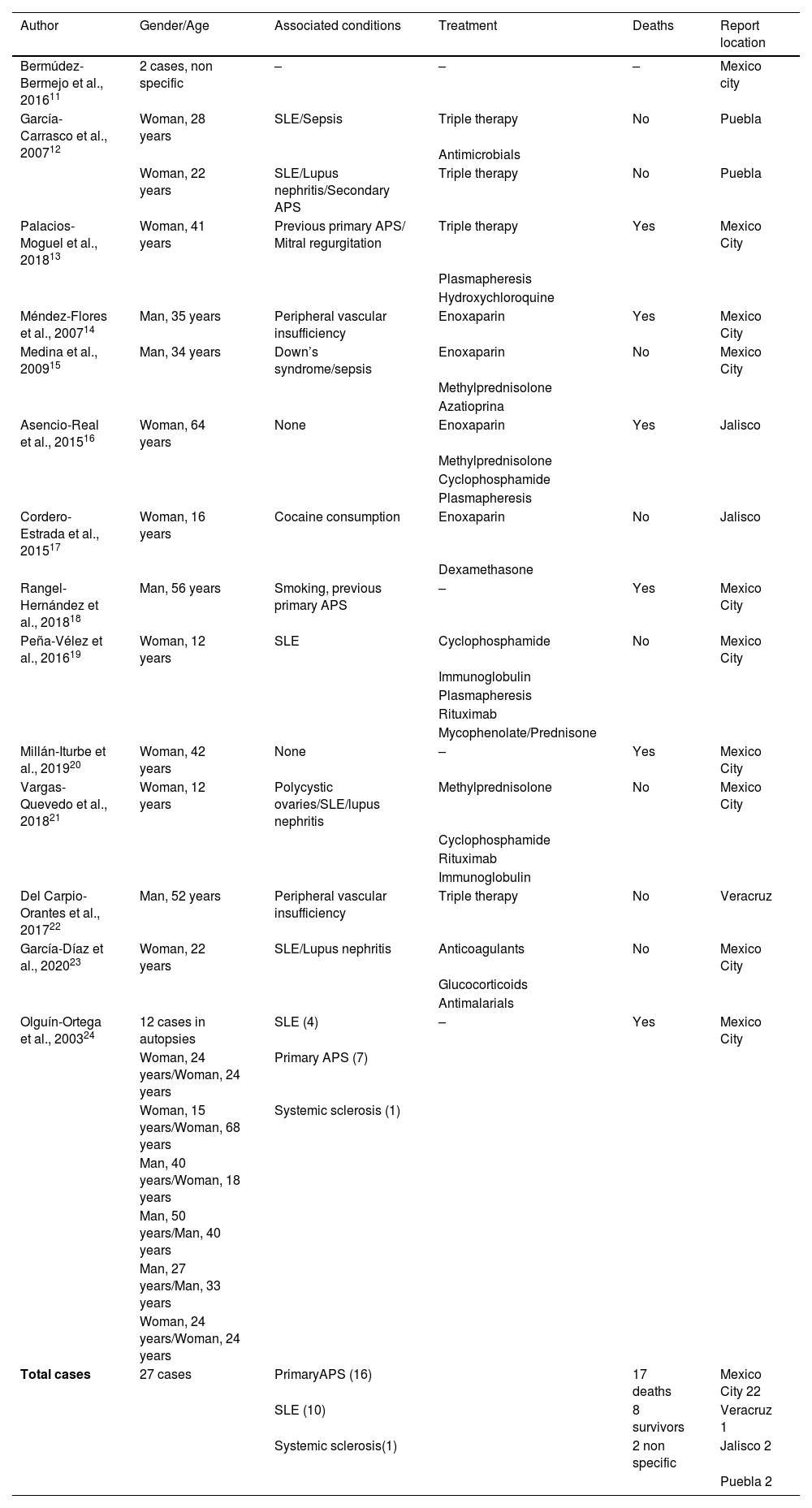
ResultsA retrospective necropsy case series including 12 cases, two reports including 2 cases each, and 11 isolated clinical case reports were found; these publications were generated between 2003 and 2020. Unfortunately, the vast majority of published reports do not clearly mention the criteria used in the classification of catastrophic antiphospholipid syndrome and some reports are brief, only mentioning the clinical diagnosis at the time; Of the documents reviewed that reliably met the classification criteria, only 10 publications (10 isolated cases, 37%) demonstrated both clinical, laboratory and histopathological classification criteria, so that these cases are categorised as definite cases of catastrophic antiphospholipid syndrome and 17 probable cases of catastrophic antiphospholipid syndrome.
In total, we found data on 27 cases of CAPS, 16 (59%) corresponded to primary antiphospholipid syndrome, 41% of cases were associated with rheumatological diseases, 10 in association with systemic lupus erythematosus and 1 case with systemic sclerosis. The majority of cases are reported de novo (93%), as only two cases (7%) had previously had primary antiphospholipid syndrome and the catastrophic presentation was the initial manifestation of these de novo cases. The states reporting cases were: Mexico City with 22 cases, Jalisco with 2 cases, Puebla with 2 cases and Veracruz with 1 case.
As predisposing factors, only two cases associated with sepsis and one case associated with cocaine use were reported, with only 18 reports with detailed information, the main organs, apparatus and systems affected were: renal (80%), pulmonary (75%), neurological (65%), cardiac (50%) and dermal (47%). The most frequently reported antibodies were: anticardiolipin IgM 100%, anticardiolipin IgG 80%, antinuclear 50%, lupus anticoagulant 33%, anti-DNA 11%, anti-B2 glycoprotein 1 11%, anti-SSB 5%, anti-centromere 5% and rheumatoid factor 5%.
Regarding outcome 17 patients died, 8 survived and in 2 cases no details are specified. Only 4 reported using triple therapy among various treatments with good outcome in 75% of those cases; 3 cases used cyclophosphamide, 3 cases used isolated plasmapheresis and 2 cases used rituximab as salvage therapies, none were treated with eculizumab. The estimated prevalence rate in the Mexican population was calculated using the 2022 population (130,262,220 inhabitants) as 2 cases per 10,000,000 inhabitants (P= #events/#population x 10,000,000). The estimated mortality was 68% in this case series; it was noted that mortality by gender was higher in men at 70% while in women it was 57% (Table 2).
Characteristics of reported cases in Mexico.
| Author | Gender/Age | Associated conditions | Treatment | Deaths | Report location |
|---|---|---|---|---|---|
| Bermúdez-Bermejo et al., 201611 | 2 cases, non specific | – | – | – | Mexico city |
| García-Carrasco et al., 200712 | Woman, 28 years | SLE/Sepsis | Triple therapy | No | Puebla |
| Antimicrobials | |||||
| Woman, 22 years | SLE/Lupus nephritis/Secondary APS | Triple therapy | No | Puebla | |
| Palacios-Moguel et al., 201813 | Woman, 41 years | Previous primary APS/ Mitral regurgitation | Triple therapy | Yes | Mexico City |
| Plasmapheresis | |||||
| Hydroxychloroquine | |||||
| Méndez-Flores et al., 200714 | Man, 35 years | Peripheral vascular insufficiency | Enoxaparin | Yes | Mexico City |
| Medina et al., 200915 | Man, 34 years | Down’s syndrome/sepsis | Enoxaparin | No | Mexico City |
| Methylprednisolone | |||||
| Azatioprina | |||||
| Asencio-Real et al., 201516 | Woman, 64 years | None | Enoxaparin | Yes | Jalisco |
| Methylprednisolone | |||||
| Cyclophosphamide | |||||
| Plasmapheresis | |||||
| Cordero-Estrada et al., 201517 | Woman, 16 years | Cocaine consumption | Enoxaparin | No | Jalisco |
| Dexamethasone | |||||
| Rangel-Hernández et al., 201818 | Man, 56 years | Smoking, previous primary APS | – | Yes | Mexico City |
| Peña-Vélez et al., 201619 | Woman, 12 years | SLE | Cyclophosphamide | No | Mexico City |
| Immunoglobulin | |||||
| Plasmapheresis | |||||
| Rituximab | |||||
| Mycophenolate/Prednisone | |||||
| Millán-Iturbe et al., 201920 | Woman, 42 years | None | – | Yes | Mexico City |
| Vargas-Quevedo et al., 201821 | Woman, 12 years | Polycystic ovaries/SLE/lupus nephritis | Methylprednisolone | No | Mexico City |
| Cyclophosphamide | |||||
| Rituximab | |||||
| Immunoglobulin | |||||
| Del Carpio-Orantes et al., 201722 | Man, 52 years | Peripheral vascular insufficiency | Triple therapy | No | Veracruz |
| García-Díaz et al., 202023 | Woman, 22 years | SLE/Lupus nephritis | Anticoagulants | No | Mexico City |
| Glucocorticoids | |||||
| Antimalarials | |||||
| Olguín-Ortega et al., 200324 | 12 cases in autopsies | SLE (4) | – | Yes | Mexico City |
| Woman, 24 years/Woman, 24 years | Primary APS (7) | ||||
| Woman, 15 years/Woman, 68 years | Systemic sclerosis (1) | ||||
| Man, 40 years/Woman, 18 years | |||||
| Man, 50 years/Man, 40 years | |||||
| Man, 27 years/Man, 33 years | |||||
| Woman, 24 years/Woman, 24 years | |||||
| Total cases | 27 cases | PrimaryAPS (16) | 17 deaths | Mexico City 22 | |
| SLE (10) | 8 survivors | Veracruz 1 | |||
| Systemic sclerosis(1) | 2 non specific | Jalisco 2 | |||
| Puebla 2 |
SLE: systemic lupus erythematosus, APS: antiphospholipid syndrome.
This literature review shows that many more cases of CAPS have occurred in Mexico than have been included in the international registry, probably because they were published in journals with low visibility and not indexed – or perhaps because of ignorance of the registry – but we consider it prudent, however, to always carry out searches in all possible medical search engines in order to identify isolated cases, which will help to create a better registry (ideally to publish all definitive and probable cases that occur in the country) and at the same time help in the analysis of the information that emanates from them in order to create better national diagnostic and treatment strategies. There are no global statistics, only the prevalence of primary antiphospholipid syndrome is reported to be 40–50 cases/100,000 inhabitants, of which 1% may develop the catastrophic variety. The calculation of the prevalence and mortality rate in this series is an approximation based on national statistical data from the year 2022, although it is a static indicator that refers to a point in time and only indicates the burden of disease borne by the population; it does not mean the real prevalence, but an estimate at the time of the review of cases.12–26
ConclusionCases of catastrophic antiphospholipid syndrome in Mexico are more prevalent than those considered in the international registry. This national registry will help to improve the current diagnostic and therapeutic strategies used in the country, stimulating the implementation of triple therapy and, in refractory cases, the use of rituximab and eculizumab, which fortunately are now available, to reduce current mortality.
Conflict of interestsNone.
FundingNone.
In memory of Dr Ronald A Asherson the discoverer and scholar of CAPS; Our thanks to Dr Ricard Cervera and his team for continuing the international CAPS Registry.