The aim of the study was to investigate the demographic and clinical characteristics of Venezuelan patients with systemic sclerosis (SSc) seen in a tertiary hospital.
MethodsConsecutive patients 18 years and older who fulfilled the 2013 ACR/EULAR classification criteria for SSc and who were followed up in the outpatient clinic of the Division of Rheumatology at the Hospital Universitario de Caracas were selected for the study. Demographic and clinical variables were registered at the time of inclusion using a standard protocol.
ResultsForty-eight SSc patients were included; 46 (95.8%) were female; the mean age was 55.1±13.7 (mean±SD) years and all were of Hispanic ethnicity. Thirty-one (64.6%) had limited SSc and 17 (35.4%) had diffuse SSc. The mean duration of disease was 13.4±11.7 (mean±SD) years, 16.74±12.99 years for limited SSc and 7.52±5.25 years for diffuse SSc (p=0.0077). Raynaud's phenomenon was the most frequent manifestation (100%), followed by arthritis (68.8%), telangiectasia (60.4%), dyspnea (60.4%), dysphagia (58.3%) and puffy hands (56.3%). The modified Rodnan Skin Score (mRSS) and the frequency of dyspnea were higher in those with diffuse as compared to limited SSc (p=0.0211 and p=0.0003, respectively). We performed high-resolution computed tomography (HRCT) of the lungs in 31 patients; 14 (45.2%) had evidence of interstitial lung disease (ILD), 11 (68.8%) with diffuse SSc (p=0.0052). The most frequent anti-nuclear antibody pattern was nucleolar, accounting for 18 (42.8%) of the cases. Anti-centromere antibodies were present in 16.7% of the cases and were associated with the limited SSc subset (p=0.0443) and with calcinosis (p=0.0020). Anti-topoisomerase antibodies were associated with ILD (p=0.0077).
ConclusionsTypical clinical and serological manifestations were present in this sample of Venezuelan patients with SSc, with an expected distribution according to disease subtype. The autoantibody profile allows clinicians to identify those patients with limited forms of the disease and those without pulmonary involvement.
El objetivo de este estudio fue investigar las características demográficas y clínicas de los pacientes venezolanos con esclerosis sistémica (ES) examinados en un hospital terciario.
MétodosSe seleccionaron para el estudio pacientes consecutivos mayores de 18 años, que cumplieron los criterios de la clasificación ACR/EULAR de 2013 para ES, sometidos a seguimiento en la clínica ambulatoria del Departamento de Reumatología del Hospital Universitario de Caracas. Se registraron las variables demográficas y clínicas en el momento de la inclusión, utilizando un protocolo estándar.
ResultadosSe incluyó a 48 pacientes con ES, de los cuales 46 (95,8%) eran mujeres; la edad media fue de 55,1±13,7 (media±DE) años, todos ellos de etnia hispana. Treinta y uno de ellos (64,6%) tenían ES limitada y 17 (35,4%) ES difusa. La duración media de la enfermedad fue de 13,4±11,7 (media±DE) años: 16,74±12,99 años para ES limitada y 7,52±5,25 años para ES difusa (p=0,0077). El fenómeno de Raynaud fue la manifestación más frecuente (100%), seguida de la artritis (68,8%), la telangiectasia (60,4%), la disnea (60,4%), la disfagia (58,3%) y la hinchazón de manos (56,3%). La puntuación de la escala cutánea de Rodnan modificada (mRSS) y la frecuencia de la disnea fueron más altas en aquellos sujetos con ES difusa con respecto a los sujetos con ES limitada (p=0,0211 y p=0,0003, respectivamente). Realizamos una TAC de alta resolución pulmonar a 31 pacientes; 14 (45,2%) tenían evidencia de enfermedad pulmonar intersticial (EPI), 11 (68,8%) de ellos con ES difusa (p=0,0052). El patrón más frecuente de anticuerpos anti-nucleares fue de tipo nucleolar, representando 18 (42,8%) de los casos. Los anticuerpos anti-centrómeros estuvieron presentes en el 16,7% de los casos, asociándose al subconjunto de ES limitada (p=0,0443) con calcinosis (p=0,0020). Los anticuerpos anti-topoisomerasa estuvieron asociados a la EPI (p=0,0077).
ConclusionesLas manifestaciones clínicas y serológicas típicas estuvieron presentes en esta muestra de pacientes venezolanos con ES, con una distribución prevista con arreglo al subtipo de la enfermedad. El perfil de anticuerpos permite a los clínicos identificar a aquellos pacientes con formas limitadas de la enfermedad, y aquellos con compromiso pulmonar.
Systemic sclerosis (SSc) is a systemic autoimmune disease characterized by progressive skin and internal organ fibrosis, with various degrees of severity according to the disease subtype. Although skin fibrosis is the hallmark of the disease, it is the visceral damage that is responsible for increased morbidity and mortality.1 The clinical presentation of SSc is heterogeneous, ranging from mild fibrosis of acral portions of extremities and organs, to extensive generalized fibrosis and severe organic damage.1 The two major SSc subsets are limited cutaneous SSc (lcSSc) and diffuse cutaneous SSc (dcSSc). In patients with lcSSc, skin thickening occurs in distal extremities, whereas in patients with dcSSc skin thickening occurs proximally to the elbows or knees and often extends to the trunk.1 Visceral involvement varies between subtypes; lcSSc is more frequently associated with pulmonary arterial hypertension and severe gut disease,1 whereas dcSSc involves a higher risk of interstitial lung disease2 and renal damage.3
The disease has a low prevalence worldwide, affecting between 7.2 and 33.9 per 100,000 in Europe and North America, respectively.4 As also seen in other autoimmune diseases, the natural history and clinical phenotype of SSc may vary across geographic regions, races and ethnicities.5 For example, African American patients have an earlier onset of disease, more severe clinical manifestations and more aggressive lung disease as compared to Caucasian patient populations.6
In Latin America some studies seem to indicate a lower prevalence of the disease relative to the other world regions7,8 as well as differences in its natural history. For example, the mean age at the time of disease onset was 32 years in Dominican patients, comparable to that of their African American counterparts, and lower than in Caucasian patients.9 Also, Mexican patients showed a lower frequency of renal crisis, higher prevalence of pulmonary arterial hypertension (PAH), as well as a higher frequency of anticentromere antibodies (ACA) and anti-topoisomerase antibodies (ATA) than in the African American patient population.10 A cohort of Argentinean patients had a lower prevalence of ATA, compared to other cohorts from Europe and USA.11
To our knowledge, there are few studies on the clinical and serological characteristics of SSc patients in Venezuela. In a study of rheumatic disorders in a population of a native indigenous population in eastern Venezuela, the prevalence of SSc was estimated at 0.06% per 100.12 The aim of our study was to investigate the demographic and clinical characteristics of urban Venezuelan SSc patients seen in a tertiary hospital.
MethodsPatientsAll patients fulfilled the 2013 ACR/EULAR classification criteria of SSc and were followed in the outpatient clinic of the Rheumatology Division at the Hospital Universitario de Caracas-Venezuela during the period of April to September 2018. Patients were older than 18 years of age and were given a written informed consent form, which described clearly the goals of the study, their rights and voluntary participation. Patients with overlapping syndromes, localized scleroderma (morphea or linear disease) and previous or current cancer were excluded. The total number of patients included in this study was 48. The study was approved by the Ethics Committee of the Hospital Universitario de Caracas and was performed according to the Helsinki declaration. All patients provided signed informed consent.
MeasuresDemographic variables included age, gender, years of formal education, employment status and partner status. To assess the socioeconomic status of patients, the Graffar Scale of Méndez-Castellanos was administered. This tool is based on the study of the social characteristics of the family such as father's occupation, mother's level of education, the main source of family's income and housing conditions. It comprises five levels, ranging from the lowest (class V) to the highest (class I) socioeconomic status.13 The following comorbidities were also recorded: hypertension, diabetes mellitus and hypothyroidism. Smoking habit was registered as current, former or never smoker.
Clinical evaluationPatients were being followed at the Division of Rheumatology of Hospital Universitario de Caracas and a diagnosis of SSc previously revised and confirmed by experienced attending rheumatologists. A rheumatologist fellow with two years of training (DRV) performed the interview and physical examination at the time of recruitment. The time of appearance of the first symptom attributable to the disease (Raynaud or non-Raynaud symptom) was used to determine the onset of the disease. Duration of the disease and time of definitive diagnosis were also registered. The modified Rodnan Skin Score (mRSS) was used to evaluate the degree and extent of fibrosis. The mRSS was calculated by the sum of measurements of skin thickness in 17 different body sites, including the face, upper arms, forearms, dorsum of the hands, fingers, chest, abdomen, thighs, legs and feet. The total score (maximum of 51) was obtained by scoring 17 body areas from 0 to 3 points14; each area was graded as follows: 0=normal skin, 1=mild skin thickening, 2=moderate skin thickening with difficulty in making skin folds and no wrinkles and 3=severe skin thickness with inability to make skin folds between two examining fingers. The interobserver and intraobserver variability was calculated by measuring the results from two blinded trained rheumatologists. The interobserver and intraobserver variability between the two trained rheumatologists, using the kappa coefficient, was 0.64 (good agreement) and 0.82 (excellent agreement), respectively. Patients were classified into limited or diffuse SSc following the LeRoy criteria.15
Patients underwent spirometry and a six-minute walk test (6MWT). The presence of pulmonary fibrotic changes was evaluated by high-resolution computed tomography (HRCT), and pulmonary artery pressure (PAH) was estimated by transthoracic echocardiography; the cut-off established for PAH was >32mmHg.16 Serum samples were taken for determination of antinuclear antibodies (ANA) by indirect immunofluorescence on HEp-2 cells as substrate; and for ACA and ATA by enzyme-linked immunosorbent assay.
Statistical analysisResults are presented as mean±standard deviation or frequencies and percentages. Differences between groups were estimated by the Student's t-test for variables with normal distribution, Mann–Whitney test for variables with non-normal distribution and Chi-square or Fisher Exact tests for categorical variables. Data analyses were performed with Stata 12.0 for Windows (StataCorp, LLC, College Station, TX, USA).
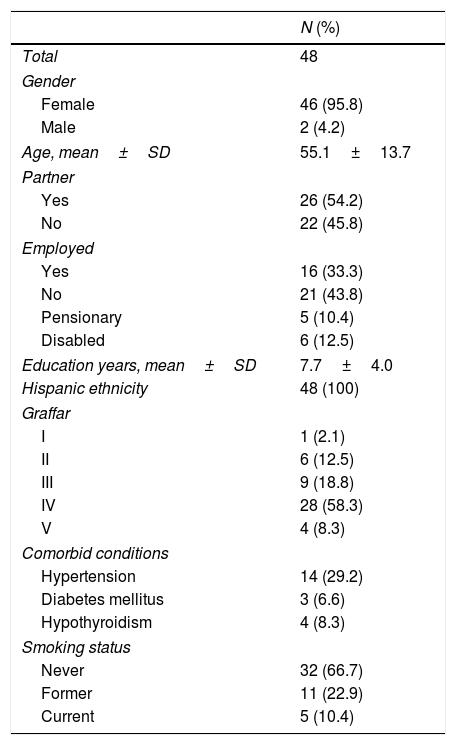
ResultsDemographic characteristicsForty-eight SSc patients were evaluated. Mean age was 55.1±13.7 years, 46 (95.8%) were female and all were of Hispanic ethnicity. The mean education was 7.7±[Standard Deviation (SD)=4.0] years. The predominant socioeconomic level was Graffar class IV (58.3%), followed by III (18.8%), II (12.5%), V (8.3%) and I (2.1%). Thirty-two patients (66.7%) reported never having smoked, 11 (22.9%) were former smokers and 5 (10.4%) were current smokers at the time of the study. Other demographic characteristics are shown in Table 1.
Sociodemographic characteristics of Venezuelan patients with systemic sclerosis.
| N (%) | |
|---|---|
| Total | 48 |
| Gender | |
| Female | 46 (95.8) |
| Male | 2 (4.2) |
| Age, mean±SD | 55.1±13.7 |
| Partner | |
| Yes | 26 (54.2) |
| No | 22 (45.8) |
| Employed | |
| Yes | 16 (33.3) |
| No | 21 (43.8) |
| Pensionary | 5 (10.4) |
| Disabled | 6 (12.5) |
| Education years, mean±SD | 7.7±4.0 |
| Hispanic ethnicity | 48 (100) |
| Graffar | |
| I | 1 (2.1) |
| II | 6 (12.5) |
| III | 9 (18.8) |
| IV | 28 (58.3) |
| V | 4 (8.3) |
| Comorbid conditions | |
| Hypertension | 14 (29.2) |
| Diabetes mellitus | 3 (6.6) |
| Hypothyroidism | 4 (8.3) |
| Smoking status | |
| Never | 32 (66.7) |
| Former | 11 (22.9) |
| Current | 5 (10.4) |
Note: SD: Standard deviation.
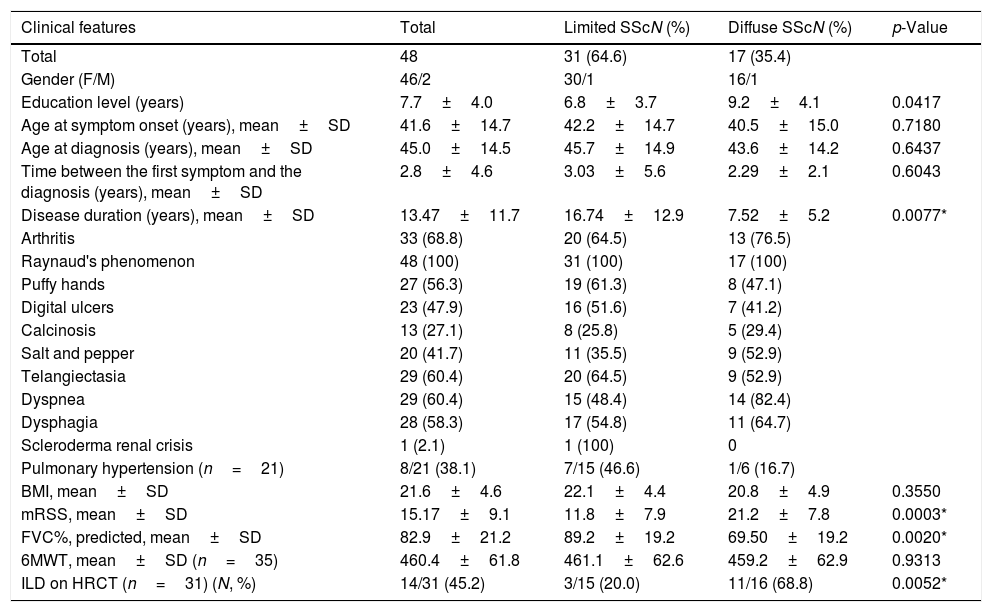
Limited SSc occurred in 64.6% of cases, while dcSSc was found in 35.4%. Patients with lcSSc had a lower mean years of education as compared to those with dcSSc: 6.8 (SD=3.7) vs 9.2 (SD=4.1) years, respectively (p=0.0417). The mean age at onset of disease was 41.6 (SD=14.7) years, and the time from the onset of symptoms to SSc diagnosis was 2.8 (SD=4.6) years, with no significant differences in these parameters between SSc subtypes. The mean duration of illness was 13.4 (SD=11.7) years, being significantly greater in the limited group (16.7 vs 7.5 years, respectively, p=0.0077) (Table 2).
Clinical characteristics of Venezuelan patients with systemic sclerosis.
| Clinical features | Total | Limited SScN (%) | Diffuse SScN (%) | p-Value |
|---|---|---|---|---|
| Total | 48 | 31 (64.6) | 17 (35.4) | |
| Gender (F/M) | 46/2 | 30/1 | 16/1 | |
| Education level (years) | 7.7±4.0 | 6.8±3.7 | 9.2±4.1 | 0.0417 |
| Age at symptom onset (years), mean±SD | 41.6±14.7 | 42.2±14.7 | 40.5±15.0 | 0.7180 |
| Age at diagnosis (years), mean±SD | 45.0±14.5 | 45.7±14.9 | 43.6±14.2 | 0.6437 |
| Time between the first symptom and the diagnosis (years), mean±SD | 2.8±4.6 | 3.03±5.6 | 2.29±2.1 | 0.6043 |
| Disease duration (years), mean±SD | 13.47±11.7 | 16.74±12.9 | 7.52±5.2 | 0.0077* |
| Arthritis | 33 (68.8) | 20 (64.5) | 13 (76.5) | |
| Raynaud's phenomenon | 48 (100) | 31 (100) | 17 (100) | |
| Puffy hands | 27 (56.3) | 19 (61.3) | 8 (47.1) | |
| Digital ulcers | 23 (47.9) | 16 (51.6) | 7 (41.2) | |
| Calcinosis | 13 (27.1) | 8 (25.8) | 5 (29.4) | |
| Salt and pepper | 20 (41.7) | 11 (35.5) | 9 (52.9) | |
| Telangiectasia | 29 (60.4) | 20 (64.5) | 9 (52.9) | |
| Dyspnea | 29 (60.4) | 15 (48.4) | 14 (82.4) | |
| Dysphagia | 28 (58.3) | 17 (54.8) | 11 (64.7) | |
| Scleroderma renal crisis | 1 (2.1) | 1 (100) | 0 | |
| Pulmonary hypertension (n=21) | 8/21 (38.1) | 7/15 (46.6) | 1/6 (16.7) | |
| BMI, mean±SD | 21.6±4.6 | 22.1±4.4 | 20.8±4.9 | 0.3550 |
| mRSS, mean±SD | 15.17±9.1 | 11.8±7.9 | 21.2±7.8 | 0.0003* |
| FVC%, predicted, mean±SD | 82.9±21.2 | 89.2±19.2 | 69.50±19.2 | 0.0020* |
| 6MWT, mean±SD (n=35) | 460.4±61.8 | 461.1±62.6 | 459.2±62.9 | 0.9313 |
| ILD on HRCT (n=31) (N, %) | 14/31 (45.2) | 3/15 (20.0) | 11/16 (68.8) | 0.0052* |
Note: SSc: Systemic Sclerosis; F: female; M: male: SD: standard deviation; BMI: Body Mass Index; mRSS: Modified Rodnan Skin Sore; 6MWT: Six-Minute Walk Test; FVC: Forced Vital Capacity; ILD: Interstitial Lung Disease; HRCT: High-Resolution Computed Tomography.
* p<0.05.
Among clinical manifestations, Raynaud's phenomenon was the most frequent (100%), followed by arthritis (68.8%), telangiectasia (60.4%), dyspnea (60.4%), dysphagia (58.3%) and puffy hands (56.3%) (Table 2). The prevalence of clinical characteristics according to SSc subtype showed that those with the limited phenotype had more arthritis (64.5%), telangiectasia (64.5%) and puffy hands (61.3%) (Table 2). Those with the diffuse form of SSc had more dyspnea (82.4%), arthritis (76.5%) and dysphagia (64.7%). Only dyspnea showed a statistically significant difference between groups, being higher in the dcSSc subtype (82.4% vs 48.4%, p=0.0211). Regarding the extent of fibrosis by mRSS, a mean total score of 15.1 (SD=9.0) was found, being higher in patients with dcSSc (21.2 vs 11.8, respectively, p=0.0003). Other clinical manifestations are shown in Table 2.
The results of the spirometry testing showed a mean forced vital capacity (FVC) of 82.93% (SD=21.26). The dcSSc subset reported lower FVC as compared to the limited subtype (69.50% vs 89.27% predictive value, respectively, p=0.0020). The spirometric pattern was normal in 54.3%, restrictive in 39.1%, obstructive in 4.3% and mixed in 2.1% of patients. The 6MWT showed a mean of 460.42 meters (SD=61.82) and there were no significant differences between the SSc subtypes (Table 2).
Forty-five percent of patients had evidence of interstitial lung disease (ILD), as assessed by HRCT (n=31), being predominant in dcSSc as compared to lcSSc patients (78.6% vs. 21.4%, respectively, p=0.0052). Of the twenty-one patients who underwent transthoracic echocardiography, 8 (38.1%) had criteria for PAH, 7 (87.5%) with lcSSc and 1 (12.5%) with dcSSc (Table 2).
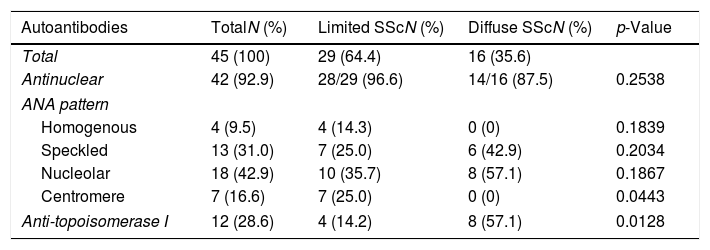
AutoantibodiesOf forty-eight patients, 45 patients underwent ANA determination. ANA were present in 42 (92.9%) patients. The most frequent ANA patterns were nucleolar (n=18, 42.8%) and speckled (n=13, 31.0%) (Table 3). ACA were detected in 7 (16.7%) patients, all in the lcSSc subset (p=0.0443). Six of these patients (85.7%) had calcinosis vs.14.3% in those patients who were ACA negative (p=0.0020). Twelve patients were positive for ATA, 8 (66.7%) in the dcSSc subset and 4 (33.3%) in the lcSSc subset. Patients seronegative for these autoantibodies were less likely to have ILD: 82.4% vs 17.6%, respectively (p=0.0077).
Distribution of autoantibodies in Venezuelan patients with systemic sclerosis.
| Autoantibodies | TotalN (%) | Limited SScN (%) | Diffuse SScN (%) | p-Value |
|---|---|---|---|---|
| Total | 45 (100) | 29 (64.4) | 16 (35.6) | |
| Antinuclear | 42 (92.9) | 28/29 (96.6) | 14/16 (87.5) | 0.2538 |
| ANA pattern | ||||
| Homogenous | 4 (9.5) | 4 (14.3) | 0 (0) | 0.1839 |
| Speckled | 13 (31.0) | 7 (25.0) | 6 (42.9) | 0.2034 |
| Nucleolar | 18 (42.9) | 10 (35.7) | 8 (57.1) | 0.1867 |
| Centromere | 7 (16.6) | 7 (25.0) | 0 (0) | 0.0443 |
| Anti-topoisomerase I | 12 (28.6) | 4 (14.2) | 8 (57.1) | 0.0128 |
Note: SSc: Systemic Sclerosis; ANA: Antinuclear Antibody by indirect immunofluorescence using HEp-2 cells as a substrate; Anti-topoisomerase I antibody by enzyme-linked immunosorbent assay.
In the present study, we looked at the sociodemographic and clinical characteristics in a sample of Venezuelan patients with SSc seen in a tertiary hospital. Differences in the demographic and clinical characteristic of those with the limited and diffuse subsets were described. Several differences were observed in the phenotypic expression and natural history of the disease compared to other populations. In contrast to results reported in Mexican10 and African American patients,3,17 our cohort showed a higher mean age, higher mean age at disease onset and higher disease duration, more comparable to the results reported in white patients of the EULAR Scleroderma Trials And Research18 (EUSTAR) and the Genetic versus Environment In Scleroderma Outcome Study19 (GENISOS) cohort studies. The female/male ratio in our study was 23:1, higher than that reported in other cohorts.4,9,11 This trend may be a result of cultural factors (for example, male patients are less likely than female patients to attend to outpatient health centers20,21) or it may be a random effect due to the relative small population studied.
Similar to the Mexican10 and Argentinean11 studies, our cohort showed a lower proportion of dcSSc cases as compared to those seen in African American patients,17 the ethnic group with the highest proportion of this SSc subset.3,17,22 The mean disease duration in our patients with dcSSc were markedly lower than in lcSSc patients, which may be explained by an earlier consultation due to the more severe clinical manifestations in patients with of dcSSc.3,22
The prevalence of ILD in our patients was 45.2%, comparable to that of Mexican10 and Caucasian EUSTAR18 patients and that of African American patients from a US cohort.17 It was also higher than that reported in the Asian, Caucasian and Hispanic patients from Northern California reported by Schmajuk et al.23 Unlike other racial/ethnic groups, in which lung damage predominated in dcSSc, in African American patients the pulmonary condition was distributed equally in both subsets.17 In our cohort, patients with dcSSc showed a higher prevalence of ILD and a lower level of FVC than patients in the lcSSc subset, as expected by the association of dcSSc with severe lung disease.2
Results of autoimmune serology showed a high frequency of ANA (92.9%), as previously reported in other cohorts.3,10,18 A close relationship was observed between ACA and the lcSSc subtype, with a similar frequency to that reported in other populations.10,17,24 Venezuelan patients had a lower frequency of ACA (15% vs 29%) but similar frequency of ATA as compared to Mexicans.10 The presence of ATA in SSc patients has been estimated to vary between 9.4% and 42%,25 which is in line with our observed prevalence of 22.7%. We found a lower frequency of ACA (15% vs 30%) and ATA (26% vs 37%) than that observed in a cohort of Caucasian patients,18 but similar to those reported in Japanese patients.24
Our study has some limitations. It was carried out in a single referral hospital, limiting the generalizability of the study, and it was based in a small sample population. There were also limitations in the extent of evaluation, such as the lack of capillaroscopic examination and a wider profile of autoantibodies due to the current humanitarian crisis and its impact on the health system in Venezuela.26 Also, we might have missed some early-onset SSc patients, some of them with nailfold capillary abnormalities.27 The strengths include the additional data to supplement the relatively scant information on the clinical expression of this disease in Latin America, and the ethnic homogeneity of the population studied.
In summary, this sample of Venezuelan patients with scleroderma presented with a clinical and serological phenotype with minor differences but otherwise comparable to other patient sample populations. The autoantibody pattern profile contributes to distinguishing the two main SSc subgroups and can help in the prediction of lung involvement.
ConclusionVenezuelan patients with SSc show a demographic and clinical pattern of expression comparable to that described in other races and ethnicities and in patient populations in different geographic latitudes. Unlike in other autoimmune conditions, the uniformity of clinical expression of the disease may suggest a relatively constrained number of shared genetic and environmental factors contributing to the triggering and development of the disease worldwide.
Ethical approvalThe study was approved by the Ethics Committee of the University Hospital of Caracas. All procedures performed in our studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki.
Informed consentInformed consent was obtained from all individual participants included in the study.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interestAuthors declare no conflict of interest.
The authors acknowledge Francisco J. Bustamante-López, MD for his contribution in the mRSS scoring and Sarah Toombs Smith, PhD, ELS for her assistance in reviewing and editing the manuscript prior to our submission, without additional salary compensation. Dr. Rodriguez is a Visiting Scholar at the Sealy Center on Aging and is partly supported by a grant from IIE-Scholar Rescue Fund.