Efforts have been made to standardise evidence-based practice, but clinical practice guidelines do not always follow strict development methods. The objective of this review is to identify the current guidelines, analyse the variability of its recommendations and make a synthesis for clinical practice.
Materials and methodsA systematic review of clinical practice guidelines was made in electronic databases and guidelines databases; using “fibromyalgia” AND [“guideline” OR “Clinical Practice guideline”] as terms, from January 2003 to July 2013. Guidelines were selected according to the following criteria: (a) aimed to fibromyalgia treatment in adults; (b) based on scientific evidence, systematically searched; (c) evidence levels and strength of recommendation included; (d) written in English or Spanish.
ResultsFrom 249 initial results, six guides fulfilled the inclusion criteria. Clinical practice guidelines analysed in this review show great variability both in the presence and level of evidence and in the strength of recommendation of many treatments. Physical exercise and cognitive-behavioural therapy are first-line treatments, showing high level of evidence. Amitriptyline, used for short periods of time for pain control, is the pharmacologic treatment with the most solid evidence. The multimodal approach reported better results than the isolated application of any treatment.
ConclusionsFinal recommendations in this review identify optimal treatments, facilitating the translation of evidence into practice and enabling more efficient and effective quality care.
Se han hecho esfuerzos en estandarizar una práctica basada en la evidencia, pero las guías de práctica clínica no siempre siguen métodos rigurosos de desarrollo. El objetivo de esta revisión es identificar las guías actuales, analizar la variabilidad de sus recomendaciones y hacer una síntesis para su uso clínico.
Material y métodoSe realizó una búsqueda sistemática de guías de práctica clínica en las bases de datos electrónicas y bases de guías; con los términos: “fibromyalgia” AND [“guideline” OR “Clinical Practice guideline”], desde enero de 2003 a julio de 2013. Se seleccionaron las guías según los siguientes criterios: (a) dirigidas al tratamiento de la fibromialgia en población adulta, (b) basadas en evidencia científica, buscada de forma sistemática, (c) incluyen niveles de evidencia y fuerza de recomendación, (d) escritas en inglés o español.
ResultadosDe los 249 resultados, 6 guías cumplieron con los criterios de inclusión. Las guías analizadas en esta revisión muestran gran variabilidad tanto en presencia como en nivel de evidencia y fuerza de recomendación de muchos tratamientos. El ejercicio físico y la terapia cognitivo-conductual son las terapias de primera elección, con alto nivel de evidencia. La amitriptilina, usada por periodos cortos para controlar el dolor, es el tratamiento farmacológico con evidencia más sólida. El abordaje multimodal reporta mejores resultados que la aplicación aislada de cualquier tratamiento.
ConclusionesLas recomendaciones finales identifican los tratamientos óptimos, facilitando la translación de la evidencia a la práctica y permitiendo mayor eficiencia y efectividad en una actividad asistencial de calidad.
At the present time, our knowledge about fibromyalgia (FM) is very limited. Its diagnosis is mainly based on symptoms, the treatment complex, and follow-up ill-defined; its main feature is generalized chronic pain of uncertain prognosis and great impact on the quality of life of the patients, their families and society itself. The latest research indicates that it is the second most prevalent disease among those that are characterized by chronic pain.1 Its prevalence has been estimated to be between 0.4% and 9.3% of the population in many countries around the world, with an overall mean of 2.7%. Specifically, this average is closer to those in Europe and Spain, at 2.5% and around 2.3%–2.4%, respectively.2 Moreover, FM is intimately related to other rheumatic and musculoskeletal conditions, psychological disorders and systemic diseases,2,3 which further complicate the strategies for its management.
Currently, the criteria of the American College of Rheumatology4 are those most widely accepted for diagnosing the disease; even so, they continue to be of limited value for ruling out other diseases, and there is no gold standard for the clinical diagnosis. All this, together with the lack of knowledge about the pathophysiological mechanisms of the disease, limit the therapies available for symptom relief.
These difficulties in the diagnosis and management translate into a considerable drain of resources, raising costs, both direct5 and indirect.6
The objective of this review consists in identifying, analyzing and summarizing, clearly and explicitly, the recommendations posed by the clinical practice guidelines (CPG) regarding the treatment of FM, for the purpose of offering professionals an evidence-based reference that is as informative as possible regarding the management of FM.
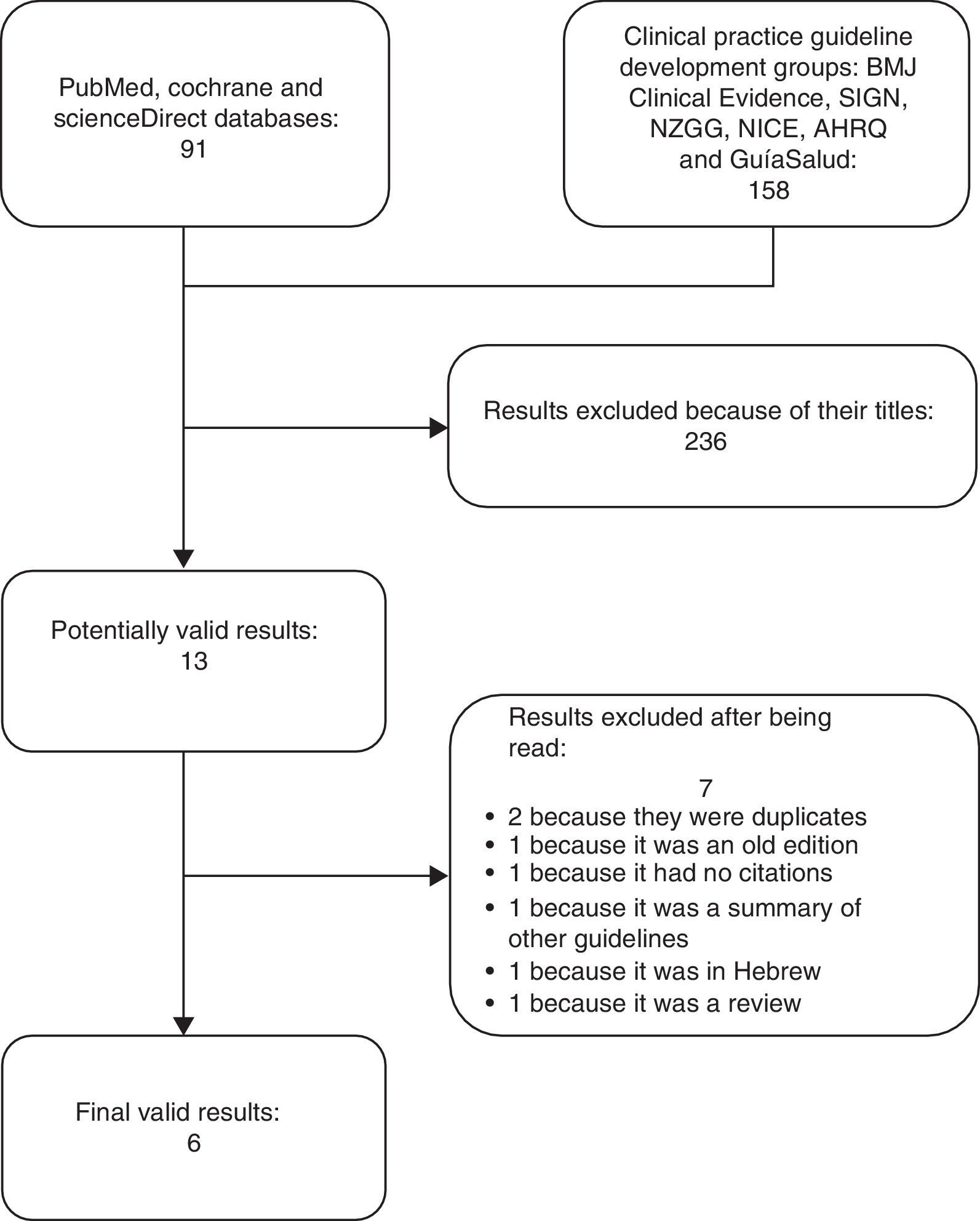
Materials and MethodsThe SearchA systematic search was conducted using the PubMed, Cochrane and ScienceDirect databases, as well as the following CPG development groups: Clinical Evidence, Scottish Intercollegiate Guidelines Network (SIGN), New Zealand Guidelines Group (NZGG), National Institute for Health and Clinical Excellence (NICE), Agency for Healthcare Research and Quality (AHRQ) and GuíaSalud. The following terms were used: “fibromyalgia” (MeSH), “guideline” (MeSH) and “clinical practice guideline”. In addition, we carried out hand searches for the most relevant articles and Google Scholar was checked. The searches were limited to literature published from January 2003 to December 2014.
Those CPG that met the following requirements: (a) be focused on the treatment of FM; (b) be based on scientific evidence (clinical trials, systematic reviews, meta-analyses); (c) include the level of evidence (LOE) and strength of recommendation (SOR), in addition to clear references; (d) involve a systematic evidence search; (e) be performed in an adult population; and (f) be written in English or Spanish. The latest available edition of each guideline was evaluated. Any complementary information provided by the guidelines was taken into account. Protocols designed by hospitals and/or departments were excluded because of their specificity and the difficulty in adapting them to other settings.
Selection of RecommendationsOnce the CPG were identified, their recommendations were analyzed and grouped according to type of treatment: general, pharmacological, physiotherapeutic, psychological, or alternative therapy. Only explicit recommendations were considered: an affirmation or easily identified statement summarizing the evidence regarding the therapies that should be used, those that can be used and others for which advice concerning their use is provided.
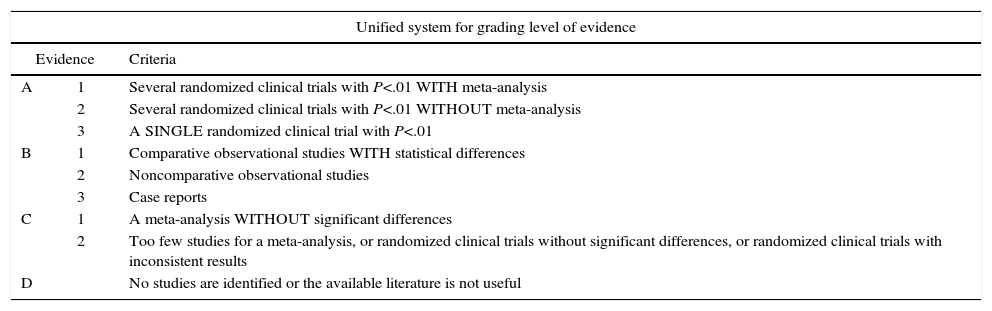
The LOE and SOR of each was identified and translated to our own standardized evidence-grading system (Table 1), developed by harmonizing the proposals of the U.S. Preventive Services Task Force7 and the SIGN8 and GRADE9 systems. This classification makes it possible to compare guidelines in terms of the LOE and SOR of the recommendations.
System for Grading Evidence.
| Unified system for grading level of evidence | ||
|---|---|---|
| Evidence | Criteria | |
| A | 1 | Several randomized clinical trials with P<.01 WITH meta-analysis |
| 2 | Several randomized clinical trials with P<.01 WITHOUT meta-analysis | |
| 3 | A SINGLE randomized clinical trial with P<.01 | |
| B | 1 | Comparative observational studies WITH statistical differences |
| 2 | Noncomparative observational studies | |
| 3 | Case reports | |
| C | 1 | A meta-analysis WITHOUT significant differences |
| 2 | Too few studies for a meta-analysis, or randomized clinical trials without significant differences, or randomized clinical trials with inconsistent results | |
| D | No studies are identified or the available literature is not useful | |
| Unified system for grading strength of recommendation | |
|---|---|
| Strength of recommendation | Scope |
| TYPE A (Is recommended) | It is suggested that the treatment be applied in all the eligible patients. The benefit is significantly greater than the possible adverse effects |
| TYPE B (Is reasonable) | It is suggested that the treatment be applied in patients. The benefit is greater than the possible adverse effects |
| TYPE C | There are no recommendations against the use of the treatment. The benefits and the adverse effects offset each other. It is not recommended in routine clinical practice |
| TYPE D (Is not recommended) | The recommendation is that the treatment not be used. Evidence suggests that the adverse effects outweigh the benefits |
| TYPE I | The evidence is poor or insufficient and does not support arguments either for or against |
Finally, the most relevant recommendations for the treatment of FM were identified on the basis of the evidence and of the variability among the guidelines, a complete recommendation has been formulated in line with the proposals in the most recent guidelines, and 2 independent collaborators reviewed the final text.
ResultsThe search provided 249 results, 13 of which were potentially valid. Of these, 7 were ruled out: 2 duplicates; an outdated version of one of the CPG; a guideline that did not provide references for the recommendations10; a systematic review11; a guideline published in Hebrew12 and a summary of other guidelines.13 Thus, ultimately, 6 publications were valid3,14–18 (Fig. 1).
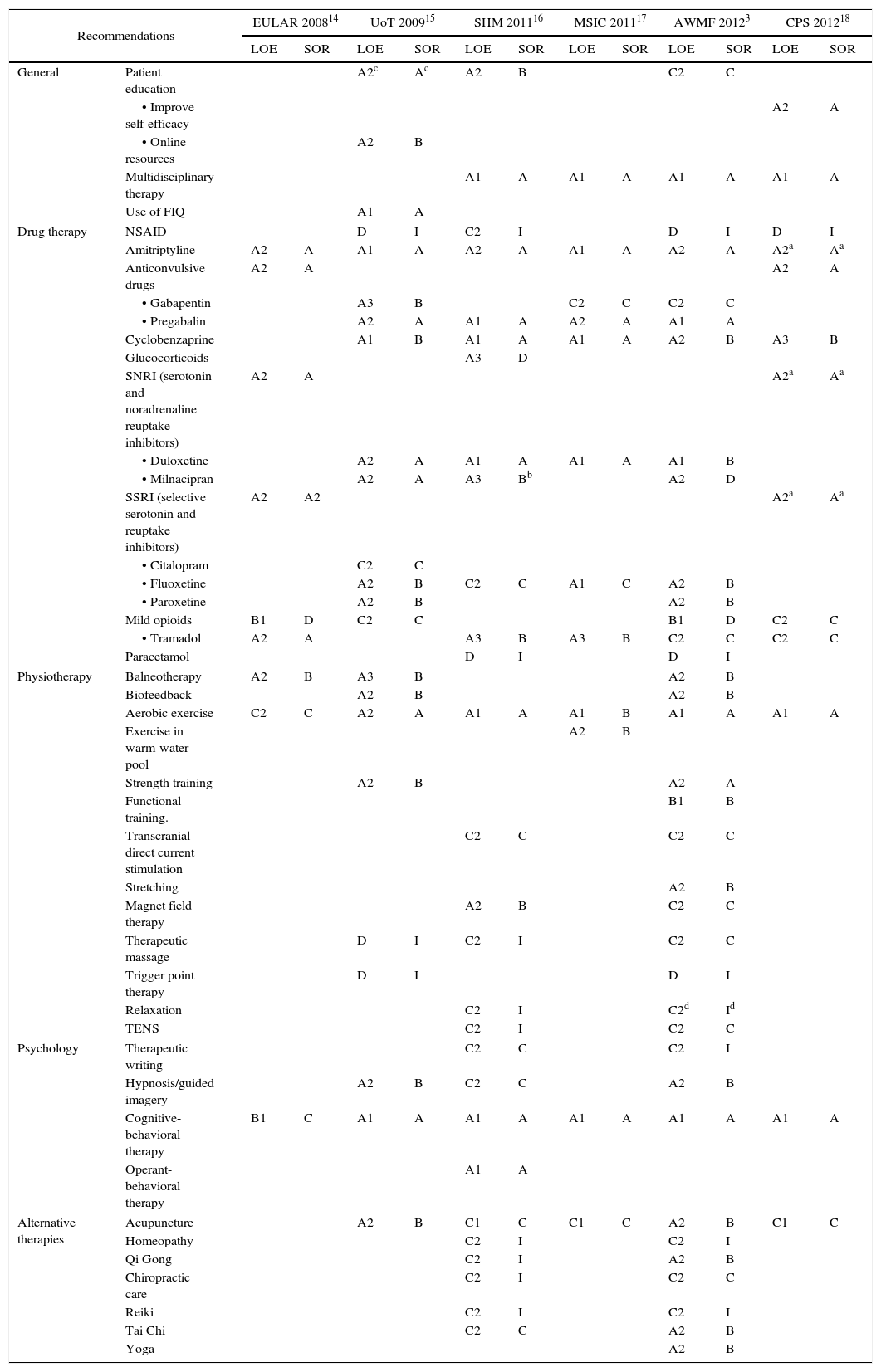
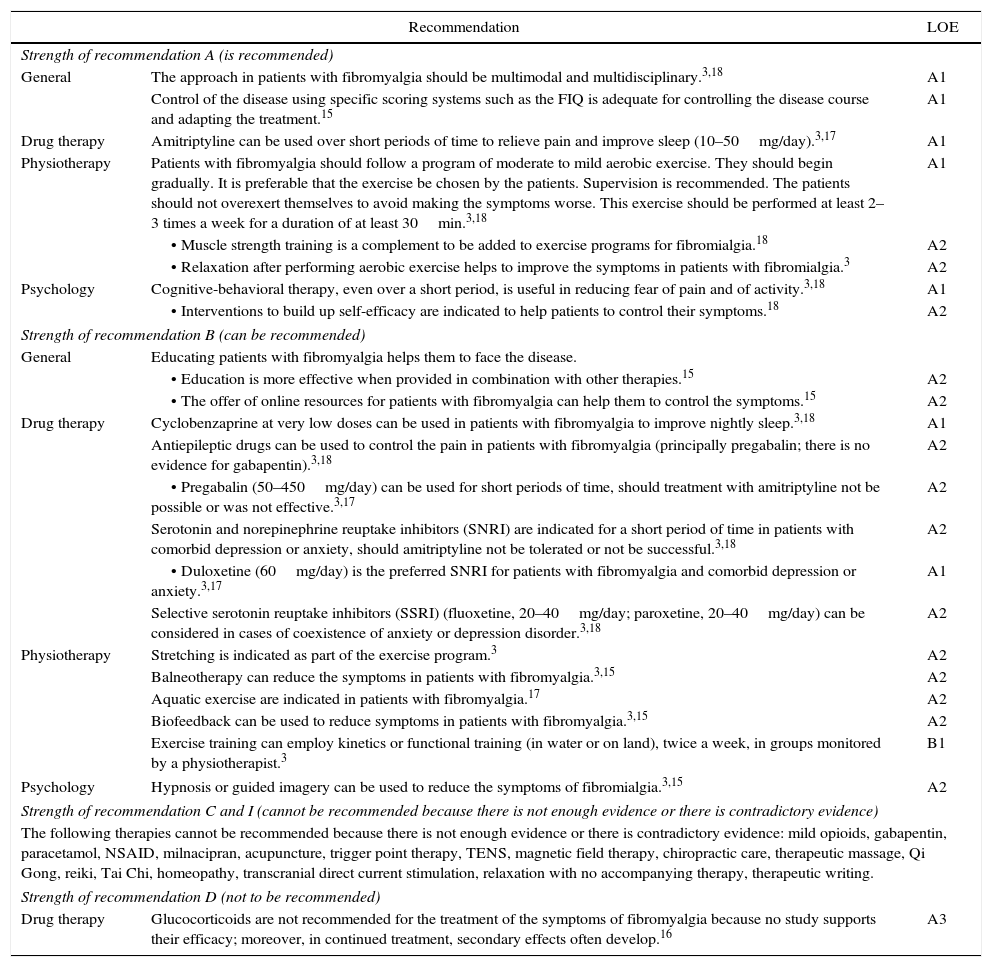
Table 2 shows the recommendations with their respective LOE and SOL for each of the CPG analyzed. In Table 3, we summarize the recommendations drawn up from the analysis of the guidelines.
LOE and SOR of the Treatments According to the Clinical Practice Guidelines.
| Recommendations | EULAR 200814 | UoT 200915 | SHM 201116 | MSIC 201117 | AWMF 20123 | CPS 201218 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LOE | SOR | LOE | SOR | LOE | SOR | LOE | SOR | LOE | SOR | LOE | SOR | ||
| General | Patient education | A2c | Ac | A2 | B | C2 | C | ||||||
| • Improve self-efficacy | A2 | A | |||||||||||
| • Online resources | A2 | B | |||||||||||
| Multidisciplinary therapy | A1 | A | A1 | A | A1 | A | A1 | A | |||||
| Use of FIQ | A1 | A | |||||||||||
| Drug therapy | NSAID | D | I | C2 | I | D | I | D | I | ||||
| Amitriptyline | A2 | A | A1 | A | A2 | A | A1 | A | A2 | A | A2a | Aa | |
| Anticonvulsive drugs | A2 | A | A2 | A | |||||||||
| • Gabapentin | A3 | B | C2 | C | C2 | C | |||||||
| • Pregabalin | A2 | A | A1 | A | A2 | A | A1 | A | |||||
| Cyclobenzaprine | A1 | B | A1 | A | A1 | A | A2 | B | A3 | B | |||
| Glucocorticoids | A3 | D | |||||||||||
| SNRI (serotonin and noradrenaline reuptake inhibitors) | A2 | A | A2a | Aa | |||||||||
| • Duloxetine | A2 | A | A1 | A | A1 | A | A1 | B | |||||
| • Milnacipran | A2 | A | A3 | Bb | A2 | D | |||||||
| SSRI (selective serotonin and reuptake inhibitors) | A2 | A2 | A2a | Aa | |||||||||
| • Citalopram | C2 | C | |||||||||||
| • Fluoxetine | A2 | B | C2 | C | A1 | C | A2 | B | |||||
| • Paroxetine | A2 | B | A2 | B | |||||||||
| Mild opioids | B1 | D | C2 | C | B1 | D | C2 | C | |||||
| • Tramadol | A2 | A | A3 | B | A3 | B | C2 | C | C2 | C | |||
| Paracetamol | D | I | D | I | |||||||||
| Physiotherapy | Balneotherapy | A2 | B | A3 | B | A2 | B | ||||||
| Biofeedback | A2 | B | A2 | B | |||||||||
| Aerobic exercise | C2 | C | A2 | A | A1 | A | A1 | B | A1 | A | A1 | A | |
| Exercise in warm-water pool | A2 | B | |||||||||||
| Strength training | A2 | B | A2 | A | |||||||||
| Functional training. | B1 | B | |||||||||||
| Transcranial direct current stimulation | C2 | C | C2 | C | |||||||||
| Stretching | A2 | B | |||||||||||
| Magnet field therapy | A2 | B | C2 | C | |||||||||
| Therapeutic massage | D | I | C2 | I | C2 | C | |||||||
| Trigger point therapy | D | I | D | I | |||||||||
| Relaxation | C2 | I | C2d | Id | |||||||||
| TENS | C2 | I | C2 | C | |||||||||
| Psychology | Therapeutic writing | C2 | C | C2 | I | ||||||||
| Hypnosis/guided imagery | A2 | B | C2 | C | A2 | B | |||||||
| Cognitive-behavioral therapy | B1 | C | A1 | A | A1 | A | A1 | A | A1 | A | A1 | A | |
| Operant-behavioral therapy | A1 | A | |||||||||||
| Alternative therapies | Acupuncture | A2 | B | C1 | C | C1 | C | A2 | B | C1 | C | ||
| Homeopathy | C2 | I | C2 | I | |||||||||
| Qi Gong | C2 | I | A2 | B | |||||||||
| Chiropractic care | C2 | I | C2 | C | |||||||||
| Reiki | C2 | I | C2 | I | |||||||||
| Tai Chi | C2 | C | A2 | B | |||||||||
| Yoga | A2 | B | |||||||||||
AWMF, Association of the Scientific Medical Societies in Germany; CPS, Canadian Pain Society; EULAR, European League Against Rheumatism; FIQ, Fibromyalgia Impact Questionnaire; LOE, level of evidence; MSIC, Ministry of Science & Innovation of Catalonia, Spain; NSAID, nonsteroidal anti-inflammatory drugs; SMH, Spanish Ministry of Health; SOR, strength of recommendation; TENS, transcutaneous electrical nerve stimulation; UoT, University of Texas.
Summaries of Recommendations Collected From the Guidelines.
| Recommendation | LOE | |
|---|---|---|
| Strength of recommendation A (is recommended) | ||
| General | The approach in patients with fibromyalgia should be multimodal and multidisciplinary.3,18 | A1 |
| Control of the disease using specific scoring systems such as the FIQ is adequate for controlling the disease course and adapting the treatment.15 | A1 | |
| Drug therapy | Amitriptyline can be used over short periods of time to relieve pain and improve sleep (10–50mg/day).3,17 | A1 |
| Physiotherapy | Patients with fibromyalgia should follow a program of moderate to mild aerobic exercise. They should begin gradually. It is preferable that the exercise be chosen by the patients. Supervision is recommended. The patients should not overexert themselves to avoid making the symptoms worse. This exercise should be performed at least 2–3 times a week for a duration of at least 30min.3,18 | A1 |
| • Muscle strength training is a complement to be added to exercise programs for fibromialgia.18 | A2 | |
| • Relaxation after performing aerobic exercise helps to improve the symptoms in patients with fibromialgia.3 | A2 | |
| Psychology | Cognitive-behavioral therapy, even over a short period, is useful in reducing fear of pain and of activity.3,18 | A1 |
| • Interventions to build up self-efficacy are indicated to help patients to control their symptoms.18 | A2 | |
| Strength of recommendation B (can be recommended) | ||
| General | Educating patients with fibromyalgia helps them to face the disease. | |
| • Education is more effective when provided in combination with other therapies.15 | A2 | |
| • The offer of online resources for patients with fibromyalgia can help them to control the symptoms.15 | A2 | |
| Drug therapy | Cyclobenzaprine at very low doses can be used in patients with fibromyalgia to improve nightly sleep.3,18 | A1 |
| Antiepileptic drugs can be used to control the pain in patients with fibromyalgia (principally pregabalin; there is no evidence for gabapentin).3,18 | A2 | |
| • Pregabalin (50–450mg/day) can be used for short periods of time, should treatment with amitriptyline not be possible or was not effective.3,17 | A2 | |
| Serotonin and norepinephrine reuptake inhibitors (SNRI) are indicated for a short period of time in patients with comorbid depression or anxiety, should amitriptyline not be tolerated or not be successful.3,18 | A2 | |
| • Duloxetine (60mg/day) is the preferred SNRI for patients with fibromyalgia and comorbid depression or anxiety.3,17 | A1 | |
| Selective serotonin reuptake inhibitors (SSRI) (fluoxetine, 20–40mg/day; paroxetine, 20–40mg/day) can be considered in cases of coexistence of anxiety or depression disorder.3,18 | A2 | |
| Physiotherapy | Stretching is indicated as part of the exercise program.3 | A2 |
| Balneotherapy can reduce the symptoms in patients with fibromyalgia.3,15 | A2 | |
| Aquatic exercise are indicated in patients with fibromyalgia.17 | A2 | |
| Biofeedback can be used to reduce symptoms in patients with fibromyalgia.3,15 | A2 | |
| Exercise training can employ kinetics or functional training (in water or on land), twice a week, in groups monitored by a physiotherapist.3 | B1 | |
| Psychology | Hypnosis or guided imagery can be used to reduce the symptoms of fibromialgia.3,15 | A2 |
| Strength of recommendation C and I (cannot be recommended because there is not enough evidence or there is contradictory evidence) | ||
| The following therapies cannot be recommended because there is not enough evidence or there is contradictory evidence: mild opioids, gabapentin, paracetamol, NSAID, milnacipran, acupuncture, trigger point therapy, TENS, magnetic field therapy, chiropractic care, therapeutic massage, Qi Gong, reiki, Tai Chi, homeopathy, transcranial direct current stimulation, relaxation with no accompanying therapy, therapeutic writing. | ||
| Strength of recommendation D (not to be recommended) | ||
| Drug therapy | Glucocorticoids are not recommended for the treatment of the symptoms of fibromyalgia because no study supports their efficacy; moreover, in continued treatment, secondary effects often develop.16 | A3 |
FIQ, Fibromyalgia Impact Questionnaire; NSAID, nonsteroidal anti-inflammatory drugs; TENS, transcutaneous electrical nerve stimulation.
The CPG included evaluate the available evidence on general, pharmacological, physiotherapeutic, psychological, and alternative therapies. Only 7 therapies appear in all the guidelines: aerobic exercise, cognitive-behavioral therapy, amitriptyline, selective serotonin reuptake inhibitors (SSRI), serotonin and noradrenaline reuptake inhibitors (SNRI), anticonvulsive drugs and mild opioids. These recommendations show discrepancies in the LOE and SOR, except in the case of amitriptyline; however, in 1 guideline,18 the latter is grouped with the antidepressants. The SSRI, SNRI and anticonvulsive drugs are also analyzed as groups (without specifying any given agent) in 2 guidelines.14,18 Exercise and cognitive-behavioral therapy remain constant in all the guidelines issued after 2008, with the highest LOE.
Recommendations With a High Level of EvidenceWe identified 22 types of therapy that had a high LOE (A1, A2) in at least 1 of the guidelines. The appearance of recommendations of high LOE varies among the different guidelines. The guideline of the European League Against Rheumatism (EULAR)14 is that which includes the fewest of these therapies, only 8 of the 22 recommendations, and the update of the German S3 guidelines (AWMF),3 with 19, is that which includes the highest number. The analysis of the types of therapy, together with their LOE and SOR (Table 2), enables the identification of the most relevant activities in the treatment of FM.
GeneralFor evaluation, the Fibromyalgia Impact Questionnaire (FIQ) ensures reliable and valid monitoring of the disease course, making it possible to adjust treatments when necessary. For patient management, the results with the multimodal approach were better than those with any single therapy by itself.
Drug TherapyAmitriptyline, used for pain relief over short periods, is the drug therapy for which the evidence is most solid, although it requires a close follow-up of the secondary effects.3 In the case of failure, intolerance or interactions of amitriptyline, there are alternative agents such as SNRI, SSRI or antiepileptic drugs; duloxetine, fluoxetine or paroxetine, and pregabalin, respectively, are the drugs of choice. The role of mild opioids in FM is limited; tramadol, which has the best results, receives contradictory recommendations.3,14,16–18 Its use can be recommended if all other options have been unsuccessful and the patient continues to feel moderate to severe pain. Treatments with these drugs should be short and resorted to in specific cases, when the symptoms are uncontrolled, and they should be discontinued as soon as possible; the medication should be titered and periodical monitoring is required.3,18
PhysiotherapyExercise programs are the treatment of choice depending on the results, as they obtain the highest LOE and SOR. They have few secondary effects and act on different variables that affect the disease, like the physical, psychological and hormonal aspects and quality of life. Among the physiotherapeutic options we find other useful therapies, such as stretching (when it complements exercise), aquatic exercise, balneotherapy and biofeedback therapy. We also took note of the therapies with a high LOE that are mentioned in only 1 guideline: exercise in a warm-water pool, functional training, stretching and yoga, all of which are related to physical activity.
PsychologyAlthough it is the area with the least recommendations, psychology offers another activity that is based on solid evidence and positive results: cognitive-behavioral therapy. It is an activity to be taken into account, whether alone or in combination with other treatments. Other psychological options, such as hypnosis, guided imagery and relaxation, only have positive results when used to complement other therapies.
Alternative TherapiesAll of the alternative therapies are subjects of controversy among the guidelines and, thus, require more and higher-quality studies to assess their applicability. Only acupuncture, Qi Gong (Chi Kung), yoga and Tai Chi receive positive recommendations in one or more of the guidelines.
Recommendations With a Low Level of Evidence That Appear in Only One GuidelineRecommendations with low LOE and SOR that appear in a single guideline were not included in the tables. For example, dietary supplements were evaluated in a meta-analysis,19 but were not found to be effective (LOE: C1, SOR: C). There are therapies that have been studied in randomized clinical trials that showed no significant differences or inconsistent results (LOE: C2) and, thus, their use cannot be recommended (SOR: C): craniosacral therapy, lymphatic drainage, hypnotic drugs, interferons, sodium oxybate, neuroleptic drugs, serotonin receptor antagonists (5-HT3), cannabinoids, thermotherapy and transcranial magnetic stimulation. In other therapies, although the LOE is the same (C2), the evidence is of poor quality or insufficient and, thus, does not support arguments either for or against their use (SOR: I): hyperbaric therapy, whole-body hyperthermia, galvanic baths, psychodynamic therapy, psychoanalysis, hormone therapy, local anesthetics, diet, dance therapy, melatonin, music therapy, cryogenic chamber, ultrasounds, laser, mindfulness, monoamine oxidase inhibitors, muscle relaxants, antiviral drugs, dopaminergic agonists, anxiolytics and potent opioids. In some cases, there is no identified evidence or the available literature is not useful (LOE: D, SOR: I) for intervention in quadrants: flupirtine, acetylsalicylic acid, acetaminophen and metamizol.
DiscussionPatient evaluation and follow-up are fundamental parts of the clinical approach, and even more so in the meticulous monitoring of the benefit and/or secondary effects of the drug therapy.20 The FIQ can be taken as an indicator of the disease course and success of the therapy, as proposed by the guidelines. Nevertheless, it is not the only tool that can serve that purpose and, thus, it is the responsibility of the professionals to use those that best adapt to the care setting of their patients.
The therapeutic approaches that should be given priority are those that do not involve drugs, among which exercise and cognitive-behavioral therapy are the treatments with the most evidence and net benefit, always respecting a multimodal approach and reserving the use of drugs for episodes of intense pain or uncontrolled symptoms. The duty of health professionals should be to base their practice on the evidence, and to offer these treatments becomes a correct clinical decision. Defining good practices for the treatment of FM is not enough; the development and use of tools for implementing and monitoring these recommendations is a fundamental step toward achieving the transmission of the evidence to practice. Evidence-based indicators for non-oncological chronic pain, including FM, have recently been published.21 The good practices on which these indicators are based coincide with the findings of this review. Thus, they should be taken into account in the monitoring of the essential processes in the treatment of FM.
Gaps in the Information in the Clinical Practice GuidelinesTwo guidelines published in 201116,17 and another 2 issued in 20123,18 differ widely in the number, type of therapy and how their recommendations are expressed, even though they were written in the same year. The differences between guidelines in terms of the recommendations of high LOE are also important. Two of the guidelines,17,18 one from 2011 and the other from 2012, present only 50% of the 22 recommendations that were classified in at least 1 other guideline as having a high LOE, whereas a guideline published earlier15 presents 68.18% of the recommendations. These should appear in all the guidelines, or at least have continuity over time once they are identified, as the continuity in the information is essential for the updating and continuing education of the professionals.
These data cast doubt on the method of creating the guidelines. The CPG are at the peak of the information pyramid,22 they are the mode of transmitting the results of research to professionals and reducing the variability in practice.23 Thus, it is necessary to draft them in accordance with the highest quality and thoroughness possible. Therefore, when it comes to developing a clinical practice guideline, it is advisable that certain recommendations be followed, like those issued by the Institute of Medicine.23 Other models for creating, developing and implementing guidelines are the elements proposed in the Appraisal of Guidelines Research & Evaluation (AGRE)24 and those of the Guide Line Implementation Appraisal (GLIA).25
The Need to Give Priority to Nonpharmacological StrategiesTo cover every aspect of FM, it is necessary to approach treatment with an interdisciplinary strategy, which has been shown to be effective,26 but some approaches must be given priority over others. The evidence shows that nonpharmacological treatment is consolidated as the first line of action in FM. Some of these therapies have been shown not only to control the symptoms, but also improve the quality of life of the patients.27 In general, they are associated with little risk and can be maintained indefinitely. For this reason, we consider that they should be given priority in all the health care settings and at every level. The establishment of exercise as the basis of the treatment should be complemented by the necessary measures, both pharmacological and nonpharmacological, for individualized patient management.
The current view of chronic diseases, which includes not only biomedical, but behavioral aspects as well, has led to a change in the molds, whereby treatment and evaluation are approached from a more biopsychosocial point of view.28 Therefore, the boom in the use of cognitive-behavioral therapy in chronic diseases is not surprising. Despite the fact that the biopsychosocial model has been established in the health care and scientific settings for some time now,29 it seems to have had a lesser impact on the organization and administration of the health systems, just like the majority of the nonpharmacological treatments that have been dealt with in this review. This, together with the lack of organization and of clear protocols, leaves patients defenseless in their confrontation with the disease.30 What FM patients need is a larger number of specialized physiotherapists and psychologists incorporated into the present health care network, as well as an improvement in their integration with the other professionals to achieve a workable interdisciplinary structure.
Drug Therapy: An Ephemeral AllyWhen we analyze drug therapy, we find that the studies evaluated by the CPG chiefly report short-term results; however, occasionally, even over these short periods of time, important secondary effects develop. This indicates that the use of drug therapy should be reserved for specific situations, to respond to uncontrolled symptoms or to intense, irruptive pain. According to the Association of the Scientific Medical Societies in Germany, even amitriptyline, the medication most widely used and studied in this disease, has important secondary effects, and the methodological quality of the evidence that supports it is relatively low.3 Other drugs, such as antiepileptic agents and antidepressants, also share these risks, and the results they offer are, at best, moderate.
Serotonin and noradrenaline reuptake inhibitors, like milnacipran, provoke a clear controversy among the guidelines. This circumstance may be influenced by the fact that the United States Food and Drug Administration (FDA) has approved this compound, whereas, in Europe, approval of its use specifically for FM has not been granted. Nevertheless, a recent meta-analysis shows that, although its benefits are similar to those of duloxetine, it is surpassed by the latter even in patients with major depression (in whom its utility has not been demonstrated).31 The opinion of the authors in every case seems to be that duloxetine should be recommended as the drug of choice as compared with milnacipran. On the other hand, SNRI could be useful to relieve pain–if fluoxetine is used–and other symptoms, such as fatigue, depression, anxiety or the overall feeling of being unwell–using fluoxetine or paroxetine, but the Spanish guidelines prefer to avoid recommending them because of the low level and controversial evidence,16,17 whereas the German guideline would recommend them, without distinguishing one type from another, in a very specific patient population and for a limited time.3
With regard to muscle relaxants, the studies are of low quality, and the results show a limited efficiency. The dilemma with using medication of this type is the possibility of undermining the capacity of the patients to perform physical activity.
The drawback in treatment with opioids is that current studies on their use are, again, limited to covering a short period of time.32 The increase in the mortality and development of important secondary effects due to different factors33 is presently creating a real public health problem in the United States,34 where their use in nonmalignant chronic disease has proliferated. In view of current evidence, the benefit of opioids in FM is not great enough for patients to accept the collateral damage that they cause. There are other methods, with fewer secondary effects and the same or greater benefits, that can be useful, and affordable, in the treatment of FM.
Implications for Future ResearchGiven the results reported in this review, it appears to be necessary to standardize the method for developing CPG. Incongruities, like those observed between the number and the LOE of the recommendations in the different guidelines are not acceptable. It is not necessary to resolve the same problem several times; if there are CPG that were developed previously, they can be adapted to our setting, supplemented or updated. In any case, it is necessary to take into account the efforts made by other authors to be efficient and congruent in the information conveyed to the health care community. It is inadmissible that in the information era and with the tools to standardize existing methodologies, there be so much difference in the contents in the guidelines analyzed in this study, and even over the years.
LimitationsThe recommendations made in this review are limited by the quality and thoroughness of the guidelines analyzed. There are limitations related to the information reported by the CPG; in some, it was taken into account whether the drugs had been approved and marketed in the country from which the guideline was issued when it came to establishing the LOE and SOR.3,17 In short, our recommendations summarize the key aspects of the guidelines included in this systematic review. They are not intended to supplant the clinical judgement of the professionals, but to serve as an aid in the principal aspects of managing this disease.
It may be interesting to know that one of the guidelines touches on the diagnosis and treatment of childhood FM syndrome,3 and concludes that there are no valid standardized criteria for diagnosing FM in children. The therapeutic processes presented are based on expert consensus due to the lack of solid evidence.
In conclusion, the variability among the existing CPG, both in the number and quality of the recommendations, continues to demonstrate the need for studies, like the present article, that review and summarize the topic. Despite these differences, there are certain effective recommendations for the management of FM that have been summarized in this text, facilitating access to the best practices. Therefore, the final step necessary for the proper management of FM is the commitment of the health care community to adhere to and implement these recommendations.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo funding of any type was received to finance the work reported in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Ángel García D, Martínez Nicolás I, Saturno Hernández PJ. «Abordaje clínico de la fibromialgia: síntesis de recomendaciones basadas en la evidencia, una revisión sistemática». Reumatol Clin. 2016;12:65–71.