To evaluate serum brain-derived neurotrophic factor (BDNF) in Egyptian patients with rheumatoid arthritis (RA) and its relation with cognitive dysfunction.
Patients and methodsThe study was carried out on 60 RA patients; 30 were active (group A) and 30 were non active (group B); and 30 controls (group C). RA disease activity was assessed via DAS28 tool, cognitive function via The Montreal Cognitive Assessment and depression via the PHQ depression scale. Serum BDNF levels were measured.
ResultsThe mean age in group A was 37.8 (±9.37) years with 83.3% females, in group B was 39.97 (±8.04) years with 86.7% females and in group C was 33.17 (±3.6) years with 93.3% females. Abnormal cognitive functions test was detected in 66.7% of group A, 66.7% of group B, and in 23.3% of group C. There was a statistically significant difference in BDNF serum level between both groups of patients (1.58±0.9ng/ml for group A, 1.81±1.17ng/ml for group B) compared with the control group (3.01±1.25ng/ml, p<0.001).
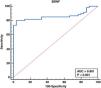
There was no statistically significant difference between BDNF and both disease duration and cognitive function, also no statistically significant difference regarding cognitive function, depression, and BNDF levels in patients with and without fibromyalgia. At a cut-off value of <2ng/ml, BDNF detected RA patients with cognitive dysfunction with a sensitivity of 80%, specificity of 96.67%.
ConclusionBDNF can be a potential biomarker of cognitive dysfunction in RA patients.
Evaluar el factor neurotrófico derivado del cerebro (BDNF) en suero en pacientes egipcios con artritis reumatoide (AR) y su relación con la disfunción cognitiva.
Pacientes y métodosEl estudio se realizó en 60 pacientes con AR; 30 eran activos (grupo A) y 30 no activos (grupo B); y 30 controles (grupo C). La actividad de la enfermedad de AR se evaluó a través de la herramienta DAS28, la función cognitiva a través de la Evaluación Cognitiva de Montreal y la depresión a través de la escala de depresión PHQ. Se midieron los niveles de BDNF en suero.
ResultadosLa edad media en el grupo A fue de 37,8 (±9,37) años con 83,3% de mujeres, en el grupo B de 39,97 (±8,04) años con 86,7% de mujeres y en el grupo C de 33,17 (±3,6) años con 93,3% de mujeres. La prueba de funciones cognitivas anormales se detectó en 66,7% del grupo A, 66,7% del grupo B y 23,3% del grupo C. Hubo una diferencia estadísticamente significativa en el nivel sérico de BDNF entre ambos grupos de pacientes (1,58±0,9ng/mL para grupo A, 1,81±1,17ng/mL para el grupo B) en comparación con el grupo control (3,01±1,25ng/mL, p<0,001).
No hubo diferencias estadísticamente significativas entre el BDNF y la duración de la enfermedad y la función cognitiva, tampoco hubo diferencias estadísticamente significativas con respecto a la función cognitiva, la depresión y los niveles de BDNF en pacientes con y sin fibromialgia. A un valor de corte de <2ng/mL, BDNF detectó pacientes con AR con disfunción cognitiva con una sensibilidad de 80% y una especificidad de 96,67%.
ConclusiónBDNF puede ser un biomarcador potencial de disfunción cognitiva en pacientes con AR.
Rheumatoid arthritis (RA) is a chronic, progressive inflammatory disorder that manifests as a symmetric polyarthritis of small and large joints that may lead to joint and periarticular structural damage and the consequences of systemic inflammation.1
Patients may also be affected by a number of extra-articular manifestations, since it is a systemic inflammatory disease.2 These manifestations usually identify a subset of patients with a more severe disease associated with a higher mortality and morbidity.3 Usually, these features are associated with the course of RA, although they are not always associated with the severity of joint involvement, and it may be dissociated from the activity of the disease.4
There has been increasing interest in the potential role of systemic inflammation in the pathogenesis of cognitive dysfunction. As intact cognitive function in RA is essential for successfully performing day-to-day activities, adhering to treatment programs, understanding the biological and clinical factors which may affect cognition is important for improving clinical outcomes and quality of life.5
Brain-derived neurotrophic factor (BDNF) stands out for its high level of expression in the brain and its potent effects on synapses. It is now widely accepted that the main function of BDNF in the adult brain is to regulate synapses, with structural and functional effects ranging from short-term to long-lasting, on excitatory or inhibitory synapses, in many brain regions. The diverse effects of BDNF on brain synapses stem from its complex downstream signaling cascades, as well as the diametrically opposing effects of the pro- and mature form through distinct receptors, tyrosine receptor kinase B(TrkB) and p75 neurotrophin receptor (NTR). Many aspects of BDNF cell biology are regulated by neuronal activity. The synergistic interactions between neuronal activity and synaptic plasticity by BDNF make it an ideal and essential regulator of cellular processes that underlie cognition and other complex behaviors.6
The aim of the present study was to assess the use of BDNF as a potential biomarker of cognitive dysfunction in Egyptian rheumatoid patients with and without activity and evaluate its relation to depression. Find a relation between cognitive dysfunction, depression, and BDNF serum levels in rheumatoid arthritis patients.
Patients and methodsThe study was carried out on 60 adult RA patients recruited from Internal Medicine Department and outpatient's clinic of Kasr Al Aini University Hospitals fulfilling European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) 2010 criteria.7 The patients were subdivided in to two groups, group A included 30 patients with active RA and group B included 30 patients with inactive RA. Patients were further classified into having fibromyalgia or not according to the 2010 American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia (ACR 2010).8 Patients with other autoimmune disease, diabetes, hypertension, coronary artery disease, cerebrovascular disease, dyslipidemia, thyroid disease, history of head trauma with loss of alertness, established neurological damage, drug abuse, dependence, or underlying psychiatric illness and those smoking were excluded from this work. Thirty apparently healthy volunteers with no history of autoimmune diseases were included as a control group. The participants provide their written informed consent to participate in this study. The study was approved by the Research Ethical committee of Cairo University (code MD-141-2021).
All patients were subjected to full history taking, complete medical examination, assessment of RA disease activity by disease activity score 28 (DAS28),9 Assessment of cognitive function was via The Montreal Cognitive Assessment (MoCA) test10 and assessment of depression using the Patient Health Questionnaire-9 (PHQ-9).11 Complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), serum level of creatinine, blood urea, uric acid, urine analysis, alanine transaminase (ALT), aspartate aminotransferase (AST), lipid profile (total cholesterol, low-density lipoprotein LDL-C, high-density lipoprotein HDL-C, Serum triglycerides TG), rheumatoid factor (RF), Anti-Cyclic Citrullinated Peptide (Anti-CCP) antibody, anti-nuclear antibody (ANA) and serum BDNF levels were measured.
Human BDNF ELISA kit (Catalog No. E1302Hu) was based on double antibody sandwich enzyme-linked immune-sorbent assay (ELISA) technology. The plate has been pre-coated with Human BDNF antibody. BDNF present in the sample is added and binds to antibodies coated on the wells. And then biotinylated Human BDNF antibody is added and binds to BDNF in the sample. Then Streptavidin-HRP is added and binds to the Biotinylated BDNF antibody. After incubation unbound Streptavidin-HRP is washed away during a washing step. Substrate solution is then added, and color develops in proportion to the amount of Human BDNF. The reaction is terminated by addition of acidic stop solution and absorbance is measured at 450nm. The optical density (OD) measured spectrophotometrically at wavelength 450±2nm is proportional to the concentration of BDNF. The BDNF concentration was calculated by comparing the sample OD to the standard curve.
Statistical analysisData were coded and entered using the statistical package for the Social Sciences (SPSS) version 28 (IBM Corp., Armonk, NY, USA). Data was summarized using mean, standard deviation, median, minimum, and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were done using unpaired t test when comparing two groups and analysis of variance (ANOVA) with multiple comparisons post hoc test when comparing more than two groups in normally distributed quantitative variables while non-parametric Kruskal–Wallis test and Mann–Whitney test were used for non-normally distributed quantitative variables.12 For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5.13p-Values less than 0.05 were considered as statistically significant.
ResultsThis study included 30 active RA patients, the mean age of them was 37.80±9.37 years with 25 females and 5 males (F:M 5:1) and 30 inactive RA patients, the mean age of them was 39.97±8.04 years with 26 females and 4 males (F:M 6.5:1). The 30 controls, the mean age was (33.17±3.6 years; with 28 females and 2 males (F:M 14:1). The mean duration of disease in group A was 56.00 (±63.29) months while in group B, it was 31.3 (±32.60) months. Characteristics of the three groups are presented in (Table 1).
Characteristics of the studied groups.
| CharacteristicsMean±SD (range) or n (%) | Active RA patients(n=30) | Inactive RA patients (n=30) | Control group(n=30) |
|---|---|---|---|
| Age (y) | 37.8±9.37 (16–50) | 39.97±8.04 (21–50) | 30.5±8.94 (19–52) |
| Duration of disease (y) | 56±63.29 | 31.3±32.6 | – |
| Gender: F:M | 25:5 (5:1) | 26:4 (6.5:1) | 28:2 (14:1) |
| BMI | 25.9±6.56 | 25.84±4.29 | 27.18±4.49 |
| Fibromyalgia | 6 (20%) | 3 (10%) | 0 (0%) |
| Cognitive dysfunction | 20 (66.7%) | 20 (66.7%) | 7 (23.3%) |
| ALT (mg/dl) | 19.4±10.58 | 17.6±6.66 | 14.73±9.53 |
| AST (mg/dl) | 2.32±10.78 | 19.2±7.69 | 15.27±7.67 |
| Urea (mg/dl) | 20.5±7.66 | 19.86±8.42 | 16.6±7.22 |
| Creatinine (mg/d) | 0.77±0.21 | 0.76±0.17 | 0.3±1 |
| Uric acid (mg/d) | 4.1±0.93 | 3.87±0.86 | 3.67±0.97 |
| ESR (mm/1st h) | 46.87±31.34 | 15.43±7.76 | 14.03±7.72 |
| CRP (mg/l) | 24.38±31.88 | 5.62±5.44 | 1.4±1.9 |
| Hb (g/dl) | 11.13±1.40 | 11.82±1.51 | 11.55±1.10 |
| TLC (109/L) | 6.79±2.59 | 6.76±2.77 | 6.61±1.69 |
| PLT (109/L) | 279.9±101.45 | 257.77±58.85 | 267.67±47.2 |
| BDNF (ng/ml) | 1.58±0.91 | 1.81±1.17 | 3.01±1.25 |
RA: rheumatoid arthritis; BMI: body mass index; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; Hb: hemoglobin; TLC: total leucocytic count; PLT: platelet; ALT: alanine transaminase; AST: aspartate transaminase; BDNF: brain-derived neurotrophic factor.
There was a statistically significant difference between the group A and B as regards depression percentage with p value 0.005. In group A, mean scale of depression was 15.17 (±6.24), while in group B, it was 10.73 (±4.18) with statistically significant p value <0.003. In group A, mean of DAS is 5.06±1.37, in group B mean of DAS is 1.85±0.58. In group A, serum BDNF was 1.58±0.91, in group B serum BDNF was 1.81±1.17 and in group C serum BDNF was 3.01±1.25ng/ml. There was a highly statistically significant difference between groups A and C as regards the BDNF (p<0.001) and between group B and C (p<0.001) (Table 2).
Comparison between active, inactive rheumatoid arthritis cases and controls.
| InvestigationMean±SD or number (percentage) | RA patients (n=60) | Control | p | |
|---|---|---|---|---|
| Active (n=30) | Inactive (n=30) | |||
| Cognitive dysfunction | 20 (66.7%) | 20 (66.7%) | 7 (23.3%) | 0.001 |
| Depression | ||||
| Scale | 15.17±6.24 | 10.73±4.18 | – | 0.003 |
| None | 2 (6.7%) | 2 (6.7%) | 3 (10%) | 0.013 |
| Mild | 4 (13.3%) | 9 (30%) | 8 (26.7%) | |
| Moderate | 7 (23.3%) | 15 (50%) | 12 (40%) | |
| Moderately severe | 7 (23.3%) | 3 (10%) | 6 (20%) | |
| Severe | 10 (33.3%) | 1 (3.3%) | 1 (3.3%) | |
| BDNF (ng/ml) | 1.58±0.91 | 1.81±1.17 | 3.01±1.25 | <0.001 |
| DAS | 5.06±1.37 | 1.85±0.58 | – | <0.001 |
RA: rheumatoid arthritis; BDNF: brain-derived neurotrophic factor.
In patients with normal cognitive function, mean of BDNF was 1.8 (±1.4), and in those with abnormal cognitive function, mean of BDNF was 1.6 (±0.9) with no statistically significance difference (Table 3).
Correlation between cognitive dysfunction and duration of disease, DAS, depression and BDNF level.
| Cognitive function | |
|---|---|
| Duration of disease | |
| Correlation coefficient | −0.149 |
| p value | 0.257 |
| DAS28 | |
| Correlation coefficient | −0.061 |
| p value | 0.645 |
| Depression | |
| Correlation coefficient | 0.113 |
| p value | 0.388 |
| BDNF | |
| Correlation coefficient | 0.079 |
| p value | 0.546 |
BDNF: brain-derived neurotrophic factor; DAS28: disease activity score 28.
In group A, 20% had fibromyalgia and only 10% in group B. The mean cognitive function in patients with FM was 23.33±3.87 while in those without FM, it was 22.9±4.51 without a statistically significant p value (p=0.561) (Table 2).
The mean depression level of patients with FM was 16.78 (±6.38), while in those without FM 12.27 (±5.39) without a statistically significant p value (p=0.034) (Fig. 1).
(A) Comparison between active and inactive rheumatoid arthritis as regards depression. (B) Compairson between patients with and without fibromyalgia as regards BDNF level. (c) Compairson between patients with and without fibromyalgia as regards depression. (D) Correlation between disease activity score and depression. (E) Correlation between RA disease duration and depression.
The mean level of BDNF of patients with FM is 1.09 (±0.17), in others without FM 1.81 (±1.10) without a statistically significant p value (p=0.013) (Fig. 1). There was no significant correlation between cognitive function and duration of disease, DAS28, depression score by PHQ-9 test or BDNF level (p=0.257, p=0.645, p=0.388, p=0.546, respectively) (Table 3). There was no statistically significant correlation between the disease duration and BDNF level (p=0.837) (Table 4). There was a positive correlation between depression and DAS score with statistically significant p value (p=0.001) and a negative correlation between depression and duration of disease with statistically significant (p=0.034). There was a non-significant correlation between depression and BDNF level (p=0.207) (Fig. 1). There was cut-off value of BDNF was ≤2ng/ml, with sensitivity and specificity of BDNF for diagnosis of cognitive dysfunction in RA patients were 80%, and 96.67 respectively. The area under the curve (AUC) was 0.861, the positive predictive value was 98 and the negative predictive value was 70.7 (Fig. 2).
Correlations between BDNF with age, disease duration, laboratory investigations, in rheumatoid arthritis patients.
| Number of each group (n=30) | Active RA | Inactive Ra |
|---|---|---|
| BDNF | BDNF | |
| Age | ||
| Correlation coefficient | −0.298 | 0.151 |
| p value | 0.109 | 0.427 |
| BMI | ||
| Correlation coefficient | −0.079 | −0.025 |
| p value | 0.677 | 0.895 |
| Urea | ||
| Correlation coefficient | −0.112 | 0.098 |
| p value | 0.556 | 0.608 |
| Creatinine | ||
| Correlation coefficient | −0.325 | 0.064 |
| p value | 0.080 | 0.736 |
| Uric acid | ||
| Correlation coefficient | −0.222 | 0.016 |
| p value | 0.239 | 0.935 |
| ALT | ||
| Correlation coefficient | −0.089 | −0.014 |
| p value | 0.639 | 0.944 |
| AST | ||
| Correlation coefficient | −0.032 | −0.206 |
| p value | 0.867 | 0.274 |
| HB | ||
| Correlation coefficient | −0.169 | 0.419 |
| p value | 0.373 | 0.021 |
| TLC | ||
| Correlation coefficient | 0.221 | 0.056 |
| p value | 0.241 | 0.770 |
| PLT | ||
| Correlation coefficient | 0.156 | 0.042 |
| p value | 0.410 | 0.824 |
| ESR | ||
| Correlation coefficient | 0.246 | −0.070 |
| p value | 0.190 | 0.713 |
| N | 30 | 30 |
| CRP | ||
| Correlation coefficient | 0.454 | 0.146 |
| p value | 0.012 | 0.441 |
| Duration of disease | ||
| Correlation coefficient | 0.027 | |
| p value | 0.837 | |
RA: rheumatoid arthritis; BMI: body mass index; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; Hb: hemoglobin; TLC: total leucocytic count; PLT: platelet; ALT: alanine transaminase; AST: aspartate transaminase.
Rheumatoid arthritis is one of the common chronic inflammatory autoimmune diseases, with synovial hypertrophy. It is a systemic disease, that not only affects joints and bones, but also there is heart, lung, eyes, psychological and dermatological affections.14
Cognitive function includes orientation, focusing, concentration, judgment, problem solving, memory, verbal, visual, spatial, and executive functions.15 Cognitive impairment in patients with RA is an annoying problem in need for more research and studies.
Brain-derived neurotrophic factor (BDNF) is a neurotrophin formed by neurons, endothelial, smooth muscle, and inflammatory cells that control transmission and synaptogenesis of glutamatergic synapses. Learning and long-term potentiation processes in the hippocampus require BDNF and its receptor, tyrosine receptor kinase B (TrkB).16
BDNF is a major member in the neurotrophin, plays a critical role not only in neurodevelopment and neuroprotection but also in synaptic plasticity, learning, and a variety of cognitive functions. Substantial evidence in animal studies showed that the up regulation of BDNF signaling pathway or endogenous BDNF levels promoted neural development and memory capability, while inhibition of BDNF signaling interfered with learning and long-term memory formation.17
We aimed in our study to find a relationship between BDNF and cognitive impairment in patients with RA and explore the possibility of using BDNF as a biomarker for this condition.
In the current study, the mean age in group A was 37.8 (±9.37), and the mean age in group B was 39.97 (±8.04). The duration of disease in group A was 56.00 months (±63.29), while the mean duration in group B was 31.3 months (±32.60).
Imran et al., who studied the level of depression in RA and its relationship with disease severity, enrolled patients with a mean age of 43.5±11.9 years, and the mean duration of disease was 7.8±5.5 years.18 While Szlachetka et al., who studied the determinants of cognitive function in RA, involved patients with a mean age of 73.7 years with RA duration of 31.3 years.19
In the current study, the median RA duration in patients with normal cognitive function was 16 months, ranging from 1 month to 180 months, while the median RA duration in impaired cognitive function patients was 24 months, ranging from 1 to 204 months. There was no statistically significant difference in the mean duration of disease between the two groups, we did not find a statistically significant correlation between RA duration and the level of cognitive dysfunction (r=−0.149, p=0.257).
In accordance with our study, Appenzeller et al., found no significant relation between the duration of the illness and cognitive impairment.20
In our study, we described cognitive dysfunction in patients with RA as compared to the control group (p=0.001) and compared it in active and inactive groups, showing that 66.7% of active RA patients had abnormal cognitive function and the same percentage in inactive patients. Bartolini et al., also observed that cognitive dysfunction was common in RA patients, with prevalence rates ranging from 38% to 71%.21
A negative correlation was found between cognitive function and the DAS score, however, without a statistically significant p value (p=0.645).
This is consistent with the findings of Abeare et al., who studied the effect of pain in RA patients on cognitive function and found that pain was inversely related to executive functioning, with higher pain levels associated with poorer performance on executive functioning tasks.5
In a study by Lee et al., a significant negative correlation was found between cognitive function and DAS28-ESR (r=−4.685) (p<0.001).22
In our study, the BDNF level was lower among patients with active RA compared with the controls (1.58±0.91ng/ml, 3.01±1.25ng/ml, p<0.001), and it was low among inactive RA patient in comparison with the control group (1.81±1.17ng/ml, 3.01±1.25ng/ml, p<0.001).
In contrast to our study, Lai et al. found that patients with RA had significantly elevated serum BDNF levels compared with those of the controls (17.9±4.2ng/ml vs. 16.4±5.3ng/ml, p=0.032), and also there was no statistically significant differences in the serum proBDNF levels (464±583pg/ml vs. 372±487pg/ml; p=0.328) between patients with RA and controls.23 The difference between our study and Lai et al. study may be related to the fact that there was high percentage of our RA patients especially active had depression especially severe depression which goes with the findings of Jin et al., who find lower levels of BDNF among patients with depression.24
Also, Forsgren et al. found that blood levels of BDNF in patients with severe RA were elevated as compared to controls, and these levels were decreased in response to anti-TNF treatment.25
ROC curve of BDNF for diagnosing cognitive dysfunction in RA patients showed that a cut-off value of BDNF was ≤2ng/ml, with sensitivity and specificity of BDNF for diagnosis of cognitive dysfunction in RA patients were 80%, and 96.67 respectively.
Consistent with our research, Rose et al. found BDNF levels were significantly lower among primary antiphospholipid syndrome patients when compared with the control group (647.3 (271.6) vs. 863.0 (318.6)pg/ml; P140.007). The calculated cut-off value was 736.5pg/ml, with a sensitivity of 70.5% (95% CI: 0.54, 0.83), specificity of 70.0% (95% CI: 0.45, 0.88), positive predictive value (PPV) of 83.8% (95% CI: 0.68, 0.94), negative predictive value (NPV) of 51.9% (95% CI: 0.32, 0.71), and accuracy of 70.3% (95% CI: 0.57, 0.81).26
In our study, we found no statistically significant correlation between the disease duration and BDNF level (p=0.837).
Consistent with our study, Haas et al., also found no correlation between plasma BDNF level and disease duration.27
Mean level of BDNF in patients with normal cognitive function 1.8 (±1.4), while in patients with abnormal cognitive function was 1.6 (±0.9).
We also found a positive correlation between cognitive function and BDNF level, however with no statistically significant p value (p=0.546).
In accordance with our results, Siuda et al., found that decreased BDNF serum levels corresponded to the severity of cognitive impairment.28
Depression is one of the most frequent comorbid conditions associated with RA, with prevalence rates ranging from 14% to 48%. Importantly, links between depression and RA appear to be bidirectional, as RA patients show an increased prevalence of depression. Conversely, patients with depression, compared to the general population, have a higher risk of developing RA.29
In our patients, either in active or inactive groups, only 6.7% were free of depression, while the remaining had depression in different degrees according to PHQ-9 test.
In group A, the mean scale of depression was 15.17 (±6.24), while in group B, it was 10.73 (±4.18) with a statistically significant p value (p=0.005). Eighty percent of patients had moderate to severe depression.
Pezzato et al. found the prevalence of depression to be 14.3% among patients with RA. Out of the 70 depressed patients, 30 subjects, already known to be depressed in the past, were still depressed at the time of the assessment, with only 11 (15.7%) on antidepressants. Their multivariate analysis showed that male sex, a higher patient global assessment (PGA) score, the use of antidepressants, and a higher health assessment questionnaire (HAQ) score were significantly associated with an increased risk of depression.30
Dickens et al. found twelve independent studies comparing depression in patients with rheumatoid arthritis with depression in healthy control subjects. Effect sizes for depression were mild to moderate.31
Imran et al. enrolled 102 cases of rheumatoid arthritis (RA) from the Rheumatology Department at Fatima Memorial Hospital. The relationship between depression and disease activity (severity) of rheumatoid arthritis was assessed by calculating the correlation coefficient between depression, disease activity score (DAS28) of rheumatoid arthritis and the health assessment questionnaire (HAQ). Arthritis patients were found to have some degree of depression, and this was directly related to the severity of the disease. Moderate and severe depression were present in 23 (22.5%) and 19 (18.6%) patients, respectively.18
We did not find a statistically significant correlation between the PHQ-9 test score and MOCA test score (p=0.388).
There was a positive correlation between depression and DAS score with a statistically significant p value (r=0.421, p=0.001).
Also, we found a negative correlation between the PHQ-9 test score and BDNF level without statistically significant (p=0.207) while Siuda et al. found no correlation between BDNF serum levels and depressive symptoms.28
In our study, the mean BDNF of patients with fibromyalgia was 1.09 (±0.17), while that of patients without fibromyalgia was 1.81 (±1.10) without a statistically significant p value (p=0.013).
These differ from the finding of Haas et al. who found higher levels of BDNF (FM=167.1±171.2pg/ml) when compared with the control group (control=113.8±149.6pg/ml) (p=0.049).27 This may be related to different populations with different gene susceptibility; the study involved Korean patients while ours are Egyptian, also there is some evidence that BDNF has a direct involvement in pain perception.32
BDNF serum level can be a potential biomarker for cognitive dysfunction in rheumatoid arthritis patients, however larger scale studies are still needed to confirm our findings.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare no conflict of interest.