Complex regional pain syndrome (CRPS) type 1 is characterized by the presence of pain, edema, functional impotence, impaired mobility, trophic changes, vasomotor instability and bone demineralization.
Material and methodsWe carried out a retrospective and prospective, descriptive, observational study of 108 patients over 18 years of age with suspected CRPS who met Doury's criteria. We recorded demographic data, clinical characteristics, comorbidities, previous predisposing conditions and triggering factors, such as injury or fracture. We evaluated laboratory data, serial plain X-rays, 3-phase bone scintigraphy with technetium 99 and bone density scan, as well as drug treatment, rehabilitation and disease course.
ResultsIn all, 89% of the 108 patients were women with an average age of 54.8±12.4 years. The time between the onset of the symptoms and the first visit to a physician was 3.1 months. The most common triggering factor was injury (91.7%). The most frequent psychological factor was anxiety (42.6%). All the patients reported pain and 99.07% had impaired mobility. The most frequently affected part of the body was the hand (75%; 81/108 patients) followed by the shoulder, in the shoulder-hand syndrome. All the patients had serial X-rays and changes were observed in 93.5%. Three-phase bone scintigraphy revealed evidence of disease in all 32 of the patients who underwent this study. Bone density scanning was performed in 54 patients (50%). All the patients were treated with nonsteroidal anti-inflammatory drugs, mainly diclofenac (60%). Calcium therapy was initiated in 106 patients (98.2%) and vitamin D3 therapy in 97.2%. All the patients received bisphosphonates, primarily alendronate and ibandronate (67.6% and 27.8%, respectively). Thirty-six patients (33.3%) received corticosteroids. All of the evaluated patients underwent rehabilitation involving occupational therapy. The average time to recovery was 6.31 months (range, 4–24). The outcome was favorable in 88.9% of the patients.
ConclusionThis paper describes the clinical characteristics, therapeutic features and outcome of CRPS type 1 in 108 patients. This syndrome is known to be heterogeneous, and does not always present with the well-known symptoms. We recommend establishing a differential diagnosis including other infectious and inflammatory conditions, and point out the importance of early referral, which enables early treatment.
El síndrome doloroso regional complejo (SDRC) tipo 1 se caracteriza por la presencia de dolor, edema, impotencia funcional, limitación de la movilidad, cambios tróficos, inestabilidad vasomotora y desmineralización ósea.
Material y métodosSe realizó un estudio observacional, descriptivo, retrospectivo y prospectivo de 108 pacientes de más de 18 años de edad, con sospecha clínica de SDRC, que cumplieran criterios de Doury. Se registraron datos demográficos, características clínicas, comorbilidades, antecedentes predisponentes y factores desencadenantes como traumatismo o fractura. Se evaluaron datos de laboratorio, radiografía simple comparativa, gammagrafía ósea en 3 fases con tecnecio 99 y densitometría ósea, al igual que tratamiento farmacológico, rehabilitación y evolución.
ResultadosSe incluyó a 108 pacientes, el 89% de sexo femenino, con una edad promedio de 54,8±12,4 años. El tiempo de evolución desde el comienzo de los síntomas en el momento de la consulta fue de 3,1 meses. Dentro de los factores desencadenantes, prevaleció el traumatismo con el 91,7%. La ansiedad se asoció como el factor psicológico más frecuente (42,6%). El dolor estuvo presente en el 100% de los pacientes y la limitación de la movilidad en 99,07% de los mismos. La localización más frecuente fue mano en el 75% (81/108 pacientes), seguido de síndrome hombro mano (10,9%). Se realizó radiografía comparativa en todos los casos, observando alteraciones en el 93,5%. A 32 pacientes se les realizó gammagrafía ósea en 3 fases que fueron patológicos en el 100% de los casos. Se solicitó densitometría ósea en 54 pacientes (50%). De los tratamientos indicados, todos los pacientes recibieron antiinflamatorios no esteroideos y el más frecuente fue el diclofenaco (60%). Ciento seis pacientes (98,2%) utilizaron terapia con calcio, el 97,2% vitamina D3. El 100% recibió bifosfonatos y los más utilizados fueron el alendronato y el ibandronato (el 67,6 y el 27,8%, respectivamente). Treinta y seis pacientes (33,3%) utilizaron glucocorticoides. Todos los pacientes evaluados recibieron terapia ocupacional como tratamiento rehabilitador. El tiempo de curación presentó una media de 6,31 meses (4-24). La evolución fue favorable en el 88,9% de la presente serie.
ConclusiónEl trabajo muestra las características clínicas, terapéuticas y evolutivas de SDRC tipo 1 observadas en 108 pacientes. Se reconoce como un síndrome heterogéneo, que no siempre presenta la sintomatología conocida y se recomienda plantear diagnóstico diferencial con otras patologías infecciosas e inflamatorias. Es importante destacar que la derivación precoz, permite un tratamiento oportuno.
Complex regional pain syndrome (CRPS) type 1 is characterized by pain, edema, functional impairment, limited mobility, trophic changes, vasomotor instability and bone demineralization. It affects 1 or several joint regions. Its etiology is unknown and the most common triggering factor, occurring in more than 50% of the cases, is injury.1–3 The diagnosis is based mainly on the clinical examination. The Doury criteria (Annex 1) were applied for years and, in 1994, the International Association for the Study of Pain (IASP) developed new criteria, referring to Sudeck's syndrome, as CRPS, divided into type1 and type 2, depending on the absence or presence of peripheral nerve injury, respectively.4,5 Laboratory findings are mostly utilized to rule out other disorders.6 The imaging techniques most widely used are serial plain radiographs and three-phase bone scintigraphy.7 The outcome depends on early diagnosis and appropriate treatment, and rehabilitation should be included from the very moment therapy is begun.6
The objective of the present study was to evaluate the clinical characteristics, radiological changes, therapeutic response and disease course of patients referred to our unit with suspected CRPS.
Material and MethodsWe carried out a retrospective and prospective, descriptive, observational study of 108 patients of over 18 years of age, evaluated by rheumatologists in Hospital Ricardo Gutiérrez de la Ciudad de La Plata, Argentina, in whom there was a clinical suspicion of CRPS. They retrospectively met the Doury criteria4 from December 2002 to December 2011, and were prospectively studied from December 2011 to July 2013.
We recorded demographic data, time elapsed until the initial visit (in months) and clinical characteristics. The latter included pain (inflammation, mechanical or mixed); its intensity, measured using a visual analog scale (VAS) from 0 to 100mm; its onset—acute or surreptitious; the presence of edema, hyperthermia, hypothermia, stiffness, flushing, cyanosis, sweating, limited range of motion and soft tissue retraction; and the location—affecting one joint or polyarticular, simultaneous, additive, migratory or recurrent. We evaluated predisposing factors: anxiety, depression, dyslipidemia, alcoholism, stroke and diabetes. Triggering events such as injury or a fracture and its location, previous surgery and period of immobilization. Personal history included cardiological, neurological, endocrinal, pulmonological and inflammatory history, pregnancy and medications consumed. The laboratory tests required were complete blood count, liver and renal function, lipid profile, calcium and phosphorus metabolism, blood glucose, C reactive protein, erythrocyte sedimentation rate, 24-h urinary deoxypyridinoline and vitamin D3. Rheumatoid factor and additional immunological data could be determined to rule out other possible diseases. Serial plain radiographs were requested. They were defined as normal or were found to depict localized demineralization. Three-phase bone scintigraphy was performed with technetium-99. It was reported by specialists in nuclear medicine to demonstrate the presence of CRPS type 1, according to criteria established for this disorder.7,8 Typically, it showed a diffuse increase in tracer uptake in the blood flow images and/or a characteristic increase during the delayed bone scan in the affected limb, with marked juxta-articular tracer uptake.7–9 Bone densitometry was normal, osteopenic or osteoporotic. The patients took analgesics, nonsteroidal anti-inflammatory drugs (NSAID), glucocorticoids, gabapentin, pregabalin, carbamazepine, tricyclic antidepressants, calcitonin, bisphosphonates and vitamin B complex. The period of time and the dose prescribed were recorded. Likewise, rehabilitation comprised of occupational therapy was indicated, as was the use of an orthotic device, contrast baths and sympathetic blocks. Finally, we verified whether the diagnosis employed for referral coincided with CRPS type 1 and if the outcome was favorable.
All of the participants in the study were informed that their clinical and biological data and their images would be utilized.
Statistical MethodsThe categorical variables were expressed in terms of frequencies and percentages, and the continuous variables as medians.
ResultsWe included 108 patients, 89% women, with a mean age of 54.8±12.4 years. The time elapsed between the onset of the symptoms and their visit to a physician was 3.1 months. The most prevalent of the triggering factors was injury, in 91.7%. Forty-five participants (41.7%) had injuries without surgery and 54 patients (50%) had injuries followed by surgery. Eighty patients (74.1%) had injury followed by fracture and only 9 (8.3%) had surgery without a previous injury. Associated anxiety was the most common psychological factor (42.6%), followed by depression in 23.15%. Other analyzed data were dyslipidemia in 16 patients (14.81%), diabetes in 10 patients (9.25%) and stroke in 2 (1.85%), and alcoholism was not detected in any of the patients.
Pain was present in 100% of the participants, with a mean VAS score of 87mm, and 99.07% of them reported a limited range of motion. Stiffness was observed in 94 patients (87.04%), cyanosis in 68 patients (63%) and sweating in 57 (52.8%) (Table 1).
The region most commonly affected was the hand (75%; 81/108 patients), followed by shoulder-hand syndrome (10.9%) (Table 2).
Serial radiographs were available in every case, and changes could be seen in 101 patients (93.5%). Sixty-three patients had homogeneous demineralization (58.33%) (Fig. 1), which was patchy in 38 patients (35.18%). Seven patients (6.5%) had normal radiographs at the time of evaluation.
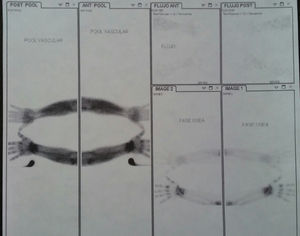
Thirty-two participants (29.9%) underwent three-phase bone scintigraphy, which showed evidence of disease in 100% of the cases (Fig. 2).
Bone densitometry had been requested for 54 of the participants (50%). The results indicated osteopenia in 25 patients (23.14%), osteoporosis in 22 (20.37%), and were normal in 7 (6.48%).
Of the indicated treatments, all of the patients received a NSAID; the agent most frequently prescribed was diclofenac (60%) (Table 3). Sixty-five (60%) of the patients received vitamin B complex, 9 (0.83%) took pregabalin, and 1 patient (0.1%) received gabapentin. In all, 106 patients (98.2%) utilized therapy involving calcium, vitamin D3 in 97.2%. One hundred percent received bisphosphonates, those most widely used being alendronate and ibandronate (67.6% and 27.8%, respectively) (Table 4).
Thirty-six patients (33.3%) utilized glucocorticoids; there were no differences between this group and those who did not. All of the patients evaluated underwent rehabilitation with occupational therapy, and they all received contrast baths. Orthotic devices were employed by 78% of the participants.
None of the patients had recurrent, additive or migratory forms.
The time required to achieve recovery was 6.31 months (4–24), corresponding as follows: 5 patients, 4 months; 87 patients, 6 months; 8 patients, 7 months; 6 patients, 12 months; and 2 patients, 24 months,
The outcome was favorable in 88.9% of the present series.
DiscussionThe mean time between the onset of symptoms and the visit of the patient to a rheumatology clinic was 3.10 months, similar to the findings in the series of Bruscas Izu et al. Another series reports longer times.10–12 Allen et al.12 went into detail on the number of physicians the patients had seen before arriving at the pain unit, and found a mean of 4.8 different professionals. This point was not evaluated in our study.
In our series, there was a predominance of the female sex (89.2%), similar to that demonstrated in other populations.10,11 The mean age was 55 years and the major triggering factor was injury. Anxiety was associated as the most common psychological factor (42.6%), followed by depression.
In our population, the hand was the part of the body most frequently affected (75% patients; 81/108), followed by the shoulder-to-hand syndrome (10.19%), similar to findings reported by other authors.11,13 This differs from the series of Bruscas Izu et al.,10 in which the lower limbs were the region most often involved.
According to other authors, the majority of the clinical findings associated with the acute phase, like hyperthermia, edema, flushing and sweating, were most frequently observed in distal sites,10 similar to what we found in our patients.
The range of motion was limited in 99.07% of the participants, a level higher than that reported by Bruscas Izu et al.10
Concerning the polyarticular (additive, simultaneous or migratory) and monoarticular forms, there is a large disparity between the different series. Gougeon et al. presented a patient population in which 42% had polyarticular involvement.13 Allen et al. found 7% to be polyarticular. Bruscas Izu et al. reported that 20% of their series had a polyarticular form, in which 16% were simultaneous, 3% additive and 0.6% migratory. In our population, 12 patients (11.1%) had polyarticular involvement, all of them simultaneous, and 1 case of recurrence affecting the same site of the carpus.
In our work, we did no other imaging studies, such magnetic resonance, computed tomography or ultrasound, as the indication was, according to the criteria of the evaluating physician, to rule out other diseases.
With respect to the rehabilitating approach, we observe that occupational therapy, when begun early, is essential for improving osteoarticular functional recovery.1
Steroids were used in 33.3% of the patients and did not change the course, when compared with the 66.7% who did not receive them. In the series of Bruscas Izu et al., glucocorticoids were indicated in 30.4% of the patients who had a predominantly inflammatory component. Although corticosteroids have shown, in several trials, that they have a beneficial effect on pain, edema and mobility during the acute phase, their administration is controversial because of their negative effects on bone mass.2
No patient was treated with calcitonin. Despite its therapeutic efficacy, we should comment that, in Argentina, it is utilized infrequently.14
In our study, we did not analyze the impact on the participants’ employment or whether there was any relationship to their occupation. Allen et al. mention that 56% of the patients associated CRPS with work, especially those employed as bakers, as police officers or in restaurants.12 Up to 54% had a claim for compensation in relation to the syndrome and 17% had some lawsuit associated with the disease.13
With respect to the outcome, the response to treatment was favorable in 88.9% of our participants. This high percentage of patients is probably due to the low incidence of comorbidities and early intervention with occupational therapy.
ConclusionThis report describes the clinical and therapeutic features and outcome of CRPS type 1 observed in 108 of our patients. This syndrome is highly heterogeneous and the symptoms can vary. A differential diagnosis including other infectious and inflammatory disorders should be established. It is important to point out that early referral of these patients from the neurology department, occupational therapy, rehabilitation, the orthopedic department and the pain clinic to the rheumatology department ensures that they receive the necessary treatment.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
- (1)
Localized mechanical, inflammatory, or mixed pain
- (2)
Cutaneous hyperesthesia
- (3)
Vasomotor alterations: localized hyper- and hypothermia
- (4)
Modification of the integument: flushing, pallor, or localized cyanosis
- (5)
Localized hyperhidrosis
- (6)
Localized edema
- (7)
Fascial or tendon retraction
- (1)
Localized homo- or heterogeneous bone demineralization without osteosclerosis or alteration of the interline
- (2)
Hyper- or hypo-uptake on the bone scan
- (1)
Absence of biological signs of inflammation (normal erythrocyte sedimentation rate)
- (1)
Noninflammatory joint fluid
- (2)
Synovial histology with evidence of vascular congestion and without inflammatory infiltrates
- (3)
Normal bone histology or with rarefaction of the trabeculae or with osteoclastic or osteoblastic hyperactivity
- (1)
Spectacular effectiveness of calcitonin, beta-blockers or sympathetic blocks
Certain diagnosis: (a) at least one criterion from each of groups A, B, and C; (b) at least one criterion from each of groups A, C, and E.
Probable diagnosis: (a) 1 criterion from each of groups B, C, and D; (b) 2 criteria from group A and at least one criterion from groups C and D; (c) 2 criteria from group A and the criterion from group E.
Possible diagnosis if a criterion from each of the double groups A and B or A and C or A and E or B and C.
Please cite this article as: Pendón G, Salas A, García M, Pereira D. Síndrome doloroso regional complejo tipo 1. Análisis de 108 pacientes. Reumatol Clin. 2017;13:73–77.